Sunday Poster Session
Category: IBD
P1111 - Inflammatory Bowel Disease Self-Care Behaviors in Context of Disease Burden and Self-Efficacy
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JA
Jordan Anders-Rumsey, MD
University of Michigan
Ann Arbor, MI
Presenting Author(s)
Jordan Anders-Rumsey, MD1, Lauren Kasimkha, MD1, Melody Chiang, BS1, Gal Hodish, MPH1, Jessica Sheehan, MD1, Jessie Golbus, MD, MS1, Ulrica Loven Wickman, PhD, RN2, Andrew Admon, MD, MS1, Kenneth Resnicow, PhD1, John Sturgeon, PhD1, Shirley Cohen-Mekelburg, MD, MS1
1University of Michigan, Ann Arbor, MI; 2linnaeus University, Linnaeus, Kalmar Lan, Sweden
Introduction: Self-management behaviors can be classified into three components: monitoring (e.g., symptom changes), adaptation (e.g., avoiding trigger foods), and maintenance (e.g., stress management). Our primary objective was to understand variation in IBD self-management behaviors. Our secondary objective was to examine the relationship between disease burden, self-efficacy, and these IBD self-management behaviors.
Methods: We conducted a prospective observational study of adult IBD patients. Participants completed the IBD Self-Care Questionnaire (SCQ), IBD Self-Efficacy Scale (IBD-SES), and ulcerative colitis or Crohn’s disease Patient Reported Outcome measures. Spearman correlations with a p< 0.10 between monitoring, adaptation, maintenance behaviors and either IBD self-efficacy or current disease burden were included in multivariable ordinal logistic regression models. For the models, the dependent variable was the specific behavior and both self-efficacy and disease burden were key independent variables, with age, sex, and IBD type as covariates.
Results: In total, 87 participants comprised the study cohort. Demographics, IBD type, and psychosocial characteristics are reported in Table 1. Participants reported more frequently monitoring intestinal symptoms as compared to non-intestinal or psychological symptoms. A smaller but substantial subset reported adapting their diet. Activity restrictions were less common, with alcohol consumption being the most commonly avoided. Patients reported monitoring sleep and stress, but their engagement in specific treatment modalities was more variable. On multivariable ordinal logistic regressions, higher self-efficacy was significantly associated with more frequent monitoring of non-inflammatory symptoms but not adaptation of behaviors. In separate multivariable ordinal logistic regressions, higher disease burden was significantly associated with more frequent adaptation (i.e., avoiding sex, avoiding activities, planning around bathrooms, planning around IBD, Table 2).
Discussion: Study findings highlight a complex relationship between IBD self-management behaviors, self-efficacy, and disease burden. Self-management support strategies that adapt to the needs of patients at times of high disease burden may offer unique benefits. Further work is needed to explore how best to adapt these strategies into effective interventions.
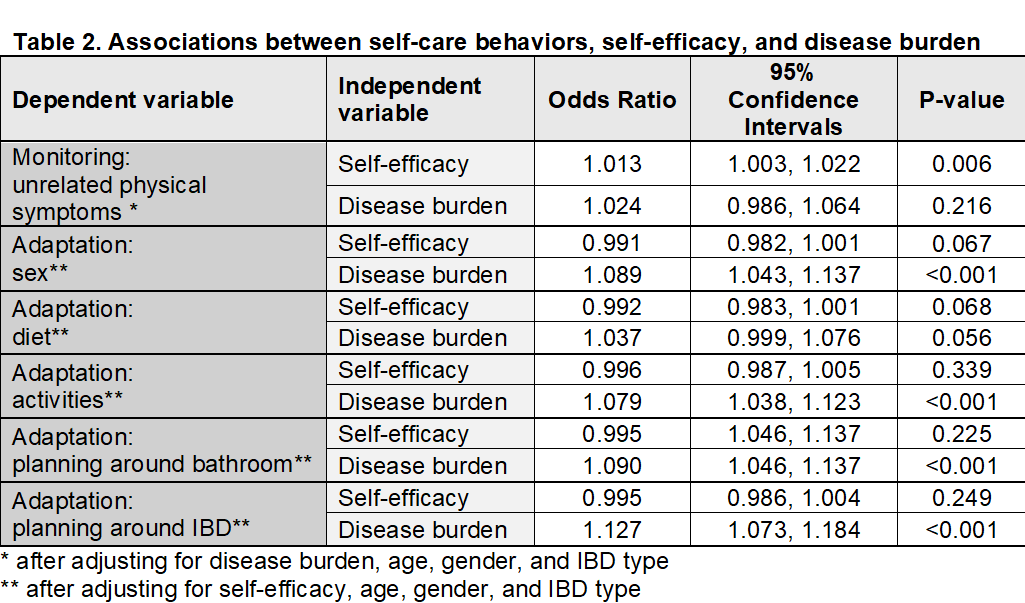
Figure: Table 1. Demographic and Individual Participants Characteristics
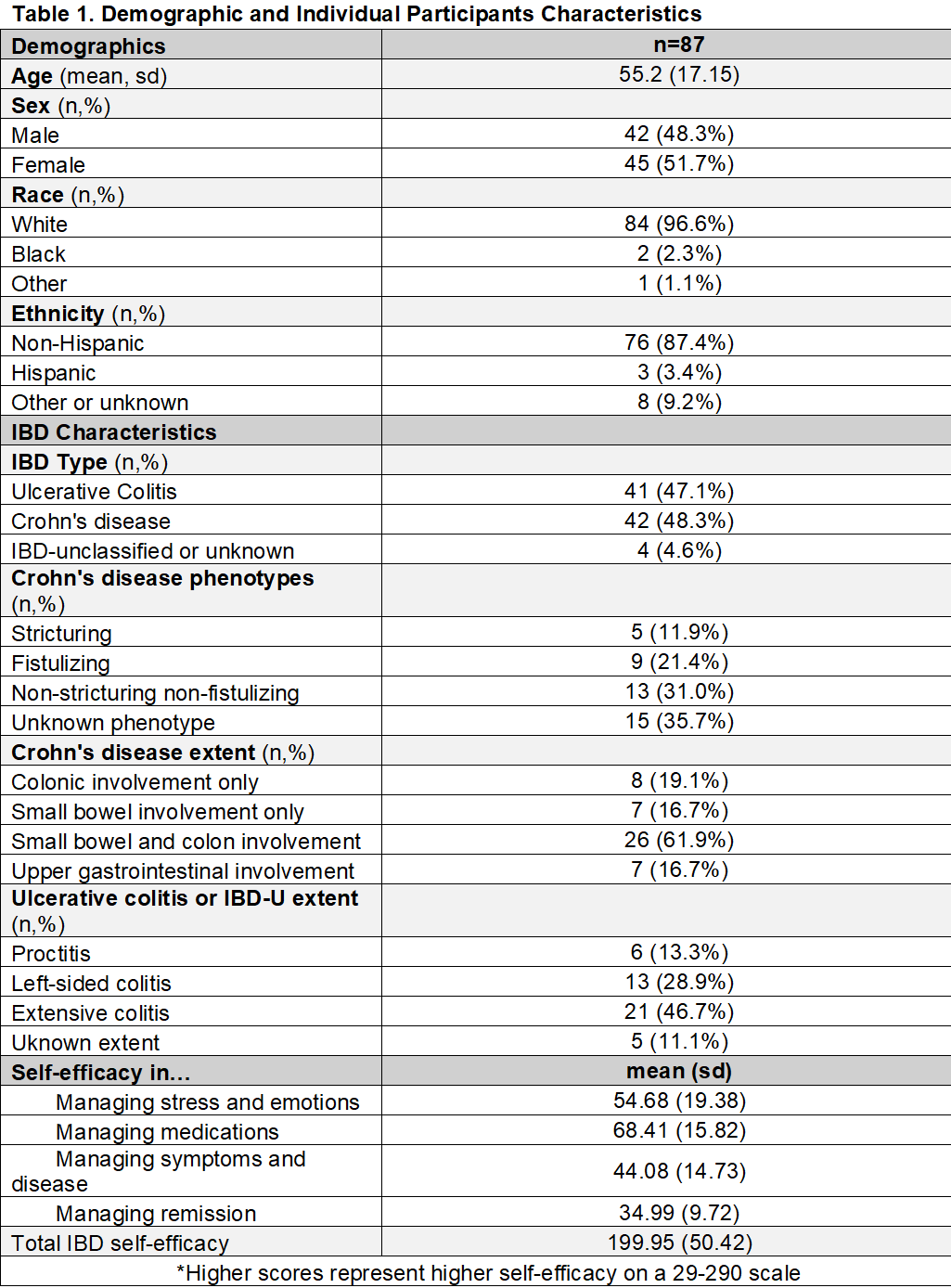
Figure: Table 2. Associations Between Self-Care Behaviors, Self-Efficacy, and Disease Burden
Disclosures:
Jordan Anders-Rumsey indicated no relevant financial relationships.
Lauren Kasimkha indicated no relevant financial relationships.
Melody Chiang indicated no relevant financial relationships.
Gal Hodish indicated no relevant financial relationships.
Jessica Sheehan indicated no relevant financial relationships.
Jessie Golbus indicated no relevant financial relationships.
Ulrica Loven Wickman indicated no relevant financial relationships.
Andrew Admon indicated no relevant financial relationships.
Kenneth Resnicow indicated no relevant financial relationships.
John Sturgeon indicated no relevant financial relationships.
Shirley Cohen-Mekelburg indicated no relevant financial relationships.
Jordan Anders-Rumsey, MD1, Lauren Kasimkha, MD1, Melody Chiang, BS1, Gal Hodish, MPH1, Jessica Sheehan, MD1, Jessie Golbus, MD, MS1, Ulrica Loven Wickman, PhD, RN2, Andrew Admon, MD, MS1, Kenneth Resnicow, PhD1, John Sturgeon, PhD1, Shirley Cohen-Mekelburg, MD, MS1. P1111 - Inflammatory Bowel Disease Self-Care Behaviors in Context of Disease Burden and Self-Efficacy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Michigan, Ann Arbor, MI; 2linnaeus University, Linnaeus, Kalmar Lan, Sweden
Introduction: Self-management behaviors can be classified into three components: monitoring (e.g., symptom changes), adaptation (e.g., avoiding trigger foods), and maintenance (e.g., stress management). Our primary objective was to understand variation in IBD self-management behaviors. Our secondary objective was to examine the relationship between disease burden, self-efficacy, and these IBD self-management behaviors.
Methods: We conducted a prospective observational study of adult IBD patients. Participants completed the IBD Self-Care Questionnaire (SCQ), IBD Self-Efficacy Scale (IBD-SES), and ulcerative colitis or Crohn’s disease Patient Reported Outcome measures. Spearman correlations with a p< 0.10 between monitoring, adaptation, maintenance behaviors and either IBD self-efficacy or current disease burden were included in multivariable ordinal logistic regression models. For the models, the dependent variable was the specific behavior and both self-efficacy and disease burden were key independent variables, with age, sex, and IBD type as covariates.
Results: In total, 87 participants comprised the study cohort. Demographics, IBD type, and psychosocial characteristics are reported in Table 1. Participants reported more frequently monitoring intestinal symptoms as compared to non-intestinal or psychological symptoms. A smaller but substantial subset reported adapting their diet. Activity restrictions were less common, with alcohol consumption being the most commonly avoided. Patients reported monitoring sleep and stress, but their engagement in specific treatment modalities was more variable. On multivariable ordinal logistic regressions, higher self-efficacy was significantly associated with more frequent monitoring of non-inflammatory symptoms but not adaptation of behaviors. In separate multivariable ordinal logistic regressions, higher disease burden was significantly associated with more frequent adaptation (i.e., avoiding sex, avoiding activities, planning around bathrooms, planning around IBD, Table 2).
Discussion: Study findings highlight a complex relationship between IBD self-management behaviors, self-efficacy, and disease burden. Self-management support strategies that adapt to the needs of patients at times of high disease burden may offer unique benefits. Further work is needed to explore how best to adapt these strategies into effective interventions.
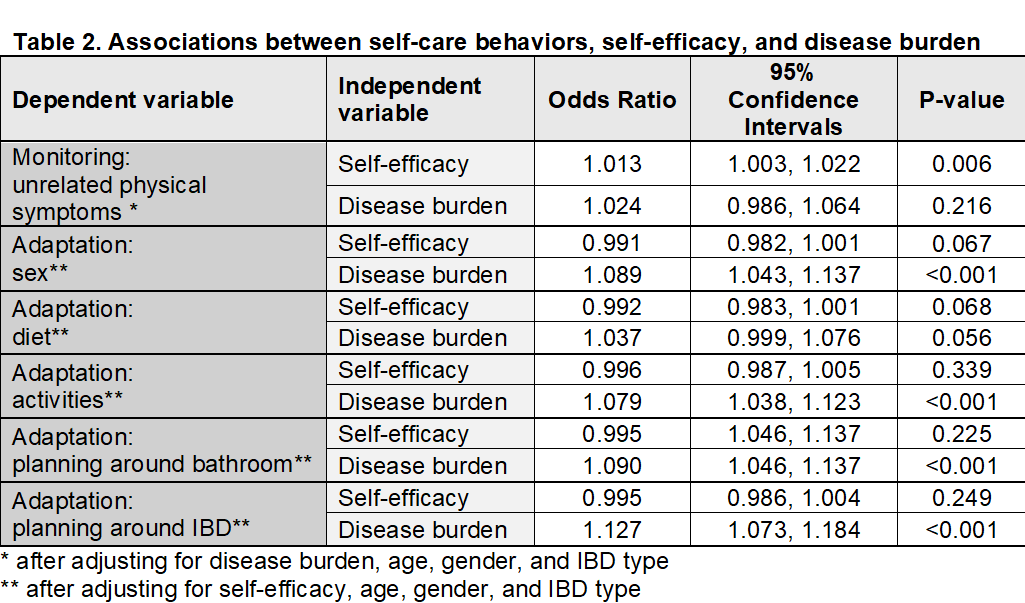
Figure: Table 1. Demographic and Individual Participants Characteristics
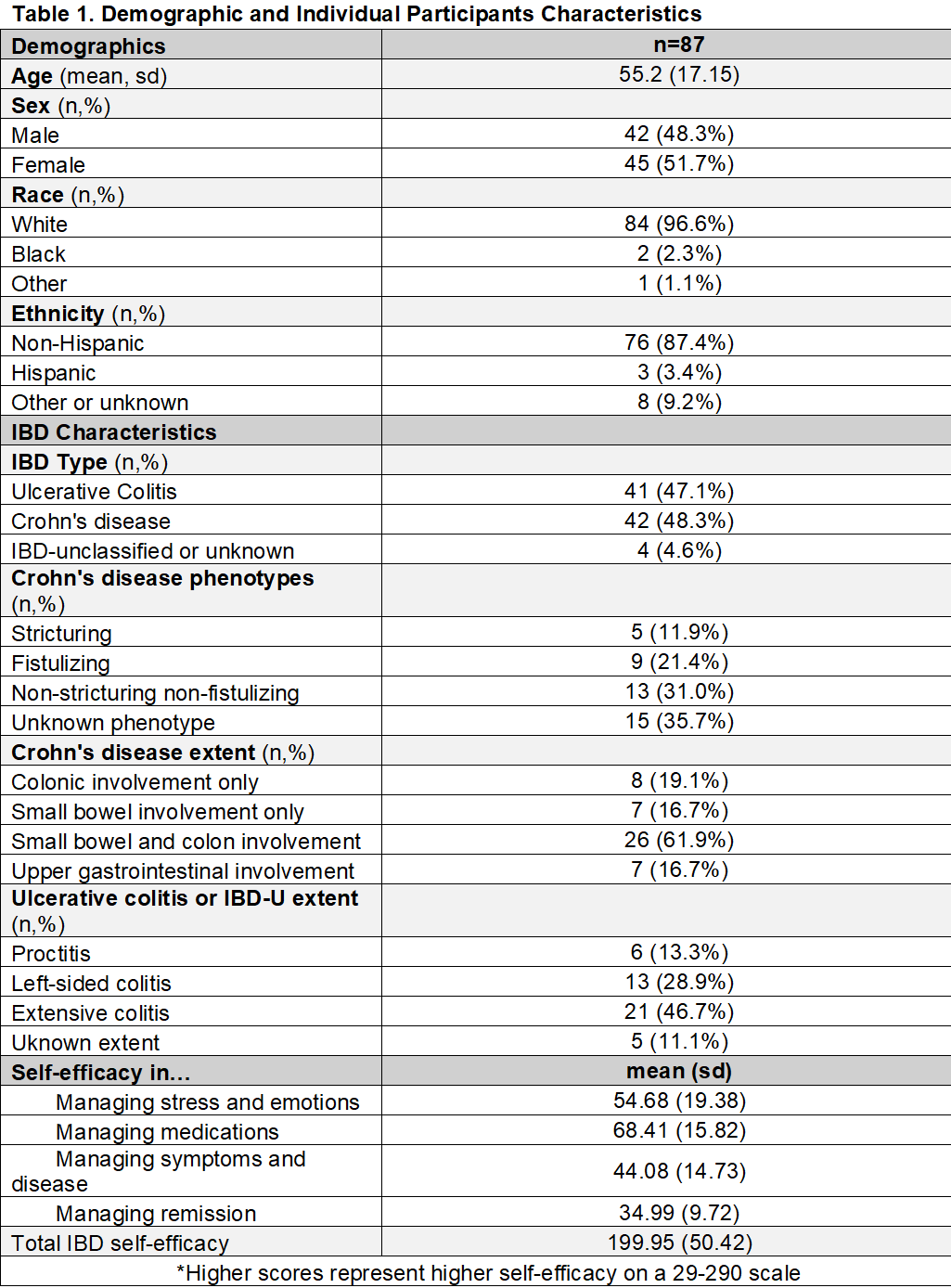
Figure: Table 2. Associations Between Self-Care Behaviors, Self-Efficacy, and Disease Burden
Disclosures:
Jordan Anders-Rumsey indicated no relevant financial relationships.
Lauren Kasimkha indicated no relevant financial relationships.
Melody Chiang indicated no relevant financial relationships.
Gal Hodish indicated no relevant financial relationships.
Jessica Sheehan indicated no relevant financial relationships.
Jessie Golbus indicated no relevant financial relationships.
Ulrica Loven Wickman indicated no relevant financial relationships.
Andrew Admon indicated no relevant financial relationships.
Kenneth Resnicow indicated no relevant financial relationships.
John Sturgeon indicated no relevant financial relationships.
Shirley Cohen-Mekelburg indicated no relevant financial relationships.
Jordan Anders-Rumsey, MD1, Lauren Kasimkha, MD1, Melody Chiang, BS1, Gal Hodish, MPH1, Jessica Sheehan, MD1, Jessie Golbus, MD, MS1, Ulrica Loven Wickman, PhD, RN2, Andrew Admon, MD, MS1, Kenneth Resnicow, PhD1, John Sturgeon, PhD1, Shirley Cohen-Mekelburg, MD, MS1. P1111 - Inflammatory Bowel Disease Self-Care Behaviors in Context of Disease Burden and Self-Efficacy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
