Sunday Poster Session
Category: IBD
P1085 - Azotemia and Ischemic Colitis Predict Medical Management Failure in Toxic Megacolon
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Joseph Gunderson, MD
University of Texas Southwestern Medical Center
Dallas, TX
Presenting Author(s)
Joseph Gunderson, MD1, David J. Schaub, MD2, Alisia C. Gunderson, MD1, Fariba Hossain, BS3, Chiu-Hsieh Hsu, PhD4, Sasha Taleban, MD, FACG3
1University of Texas Southwestern Medical Center, Dallas, TX; 2Banner - University of Arizona Tucson, Tucson, AZ; 3University of Arizona College of Medicine, Tucson, AZ; 4University of Arizona, Tucson, AZ
Introduction: Toxic megacolon (TM) is a rare but lethal complication associated with inflammatory bowel disease (IBD) and several other etiologies. Previous studies have focused on TM associated with IBD while non-IBD-associated TM has not been well studied. Additionally, data on the most common underlying disease processes and their clinical significance, clinical features, and predictors of poor outcomes, including need for surgery, are scarce and conflicting. This study aimed to describe patients with TM, determine the most common etiologies and clinical features, and identify predictors of poor outcomes.
Methods: We conducted a retrospective chart review of patients ³18 years old with TM using ICD-9/10 codes from January 2014 to June 2024. Demographic data, clinical characteristics, signs and symptoms, TM etiologies, and treatment were collected. The primary outcomes were failure of medical management and 30-day mortality. The Chi-square test, Fisher’s exact test, and Mann-Whitney U test identified differences in patients with and without IBD. Adjusted Cox regression and logistic regression identified factors associated with each outcome.
Results: 130 TM cases were identified. The median age was 64 years (52 vs. 65 for IBD and non-IBD, P < 0.001), 40% of all patients were female, and 73.1% were non-Hispanic White. The median Charlson Comorbidity Index (CCI) was 4 (1 vs. 5, P < 0.001). TM etiologies included Clostridioides difficile (50.8%), ischemic colitis (23.1%), IBD (19.2%), and others (6.9%) (Table 1).
73.8% of all patients failed medical management, of which 29.2% (6.7% vs. 33.3%, P = 0.018) deferred surgery and pursued comfort care while the remainder underwent colectomy. The colonic perforation rate was 23.8%. Ischemic colitis (aHR 1.614, 95% CI 1.013 – 2.572, P = 0.044) and creatinine >3 mg/dL (aHR = 2.196, 95% CI 1.184 – 4.073, P = 0.013) predicted medical management failure, while higher CCI (aOR 1.214, 95% CI 1.025 – 1.437, P = 0.025), and altered mental status (aOR 3.266, 95% CI 1.326 – 8.047, P = 0.010) were linked to 30-day mortality (Table 2).
Discussion: TM more frequently occurs in older, poly-comorbid patients without IBD. Azotemia and ischemic colitis appear to predict medical management failure in TM. Mortality rates for TM are significant, owing to its frequent occurrence in poly-comorbid patients without IBD who frequently pursue comfort care in lieu of undergoing colectomy. Further studies are needed to evaluate etiology-specific factors linked to poor outcomes in TM.
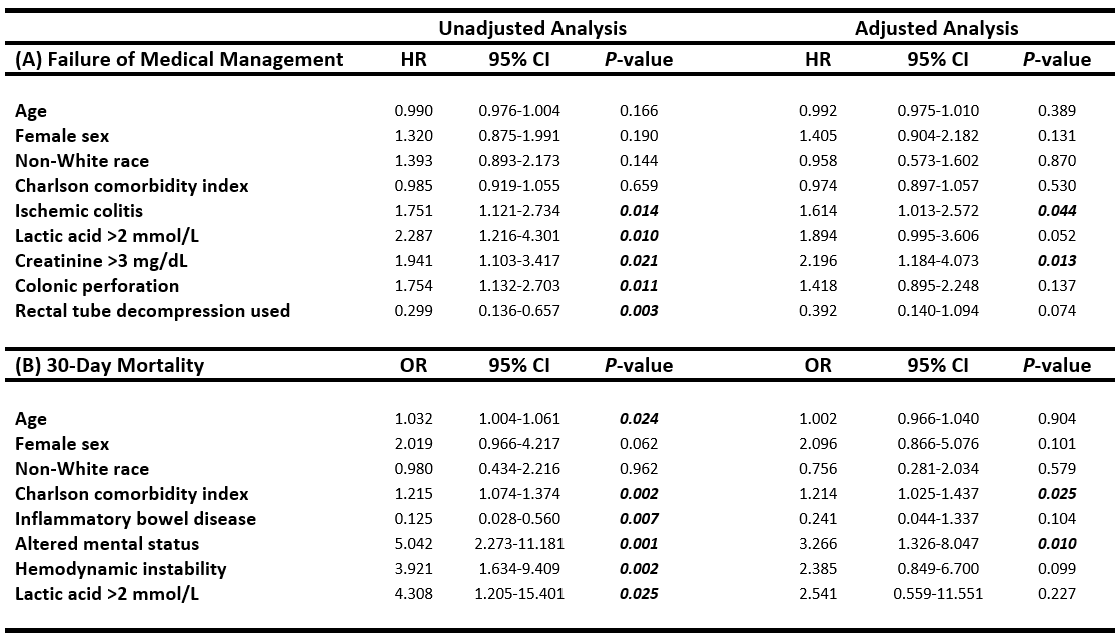
Figure: Table 1. Etiologies of toxic megacolon
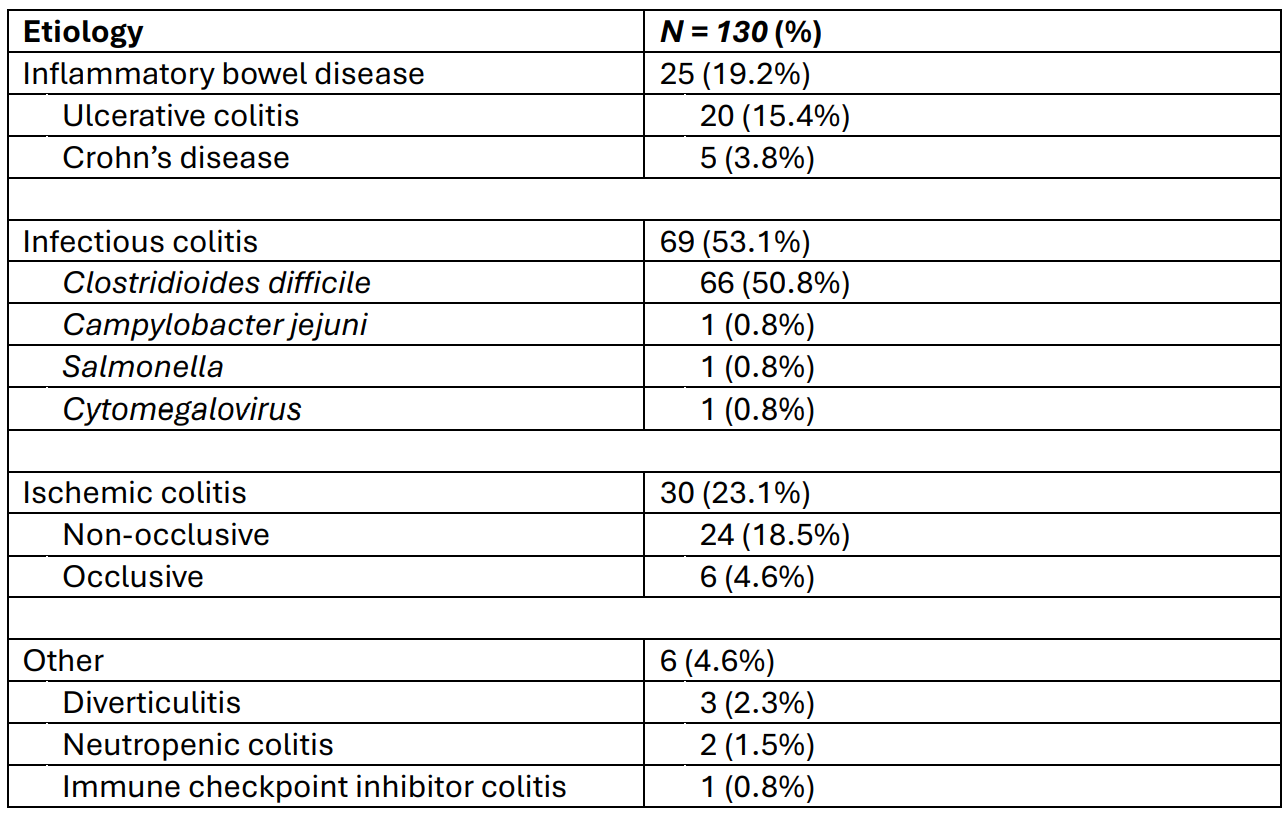
Figure: Table 2. Cox regression (A) and logistic regression (B) analyses identifying factors associated with failure of medical management and 30-day mortality, respectively
Disclosures:
Joseph Gunderson indicated no relevant financial relationships.
David Schaub indicated no relevant financial relationships.
Alisia Gunderson indicated no relevant financial relationships.
Fariba Hossain indicated no relevant financial relationships.
Chiu-Hsieh Hsu indicated no relevant financial relationships.
Sasha Taleban: AbbVie – Grant/Research Support. Boehringer-Ingelheim – Grant/Research Support. Eli Lilly – Grant/Research Support. Janssen – Advisory Committee/Board Member, Grant/Research Support. Pfizer – Grant/Research Support. Takeda – Grant/Research Support.
Joseph Gunderson, MD1, David J. Schaub, MD2, Alisia C. Gunderson, MD1, Fariba Hossain, BS3, Chiu-Hsieh Hsu, PhD4, Sasha Taleban, MD, FACG3. P1085 - Azotemia and Ischemic Colitis Predict Medical Management Failure in Toxic Megacolon, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Texas Southwestern Medical Center, Dallas, TX; 2Banner - University of Arizona Tucson, Tucson, AZ; 3University of Arizona College of Medicine, Tucson, AZ; 4University of Arizona, Tucson, AZ
Introduction: Toxic megacolon (TM) is a rare but lethal complication associated with inflammatory bowel disease (IBD) and several other etiologies. Previous studies have focused on TM associated with IBD while non-IBD-associated TM has not been well studied. Additionally, data on the most common underlying disease processes and their clinical significance, clinical features, and predictors of poor outcomes, including need for surgery, are scarce and conflicting. This study aimed to describe patients with TM, determine the most common etiologies and clinical features, and identify predictors of poor outcomes.
Methods: We conducted a retrospective chart review of patients ³18 years old with TM using ICD-9/10 codes from January 2014 to June 2024. Demographic data, clinical characteristics, signs and symptoms, TM etiologies, and treatment were collected. The primary outcomes were failure of medical management and 30-day mortality. The Chi-square test, Fisher’s exact test, and Mann-Whitney U test identified differences in patients with and without IBD. Adjusted Cox regression and logistic regression identified factors associated with each outcome.
Results: 130 TM cases were identified. The median age was 64 years (52 vs. 65 for IBD and non-IBD, P < 0.001), 40% of all patients were female, and 73.1% were non-Hispanic White. The median Charlson Comorbidity Index (CCI) was 4 (1 vs. 5, P < 0.001). TM etiologies included Clostridioides difficile (50.8%), ischemic colitis (23.1%), IBD (19.2%), and others (6.9%) (Table 1).
73.8% of all patients failed medical management, of which 29.2% (6.7% vs. 33.3%, P = 0.018) deferred surgery and pursued comfort care while the remainder underwent colectomy. The colonic perforation rate was 23.8%. Ischemic colitis (aHR 1.614, 95% CI 1.013 – 2.572, P = 0.044) and creatinine >3 mg/dL (aHR = 2.196, 95% CI 1.184 – 4.073, P = 0.013) predicted medical management failure, while higher CCI (aOR 1.214, 95% CI 1.025 – 1.437, P = 0.025), and altered mental status (aOR 3.266, 95% CI 1.326 – 8.047, P = 0.010) were linked to 30-day mortality (Table 2).
Discussion: TM more frequently occurs in older, poly-comorbid patients without IBD. Azotemia and ischemic colitis appear to predict medical management failure in TM. Mortality rates for TM are significant, owing to its frequent occurrence in poly-comorbid patients without IBD who frequently pursue comfort care in lieu of undergoing colectomy. Further studies are needed to evaluate etiology-specific factors linked to poor outcomes in TM.
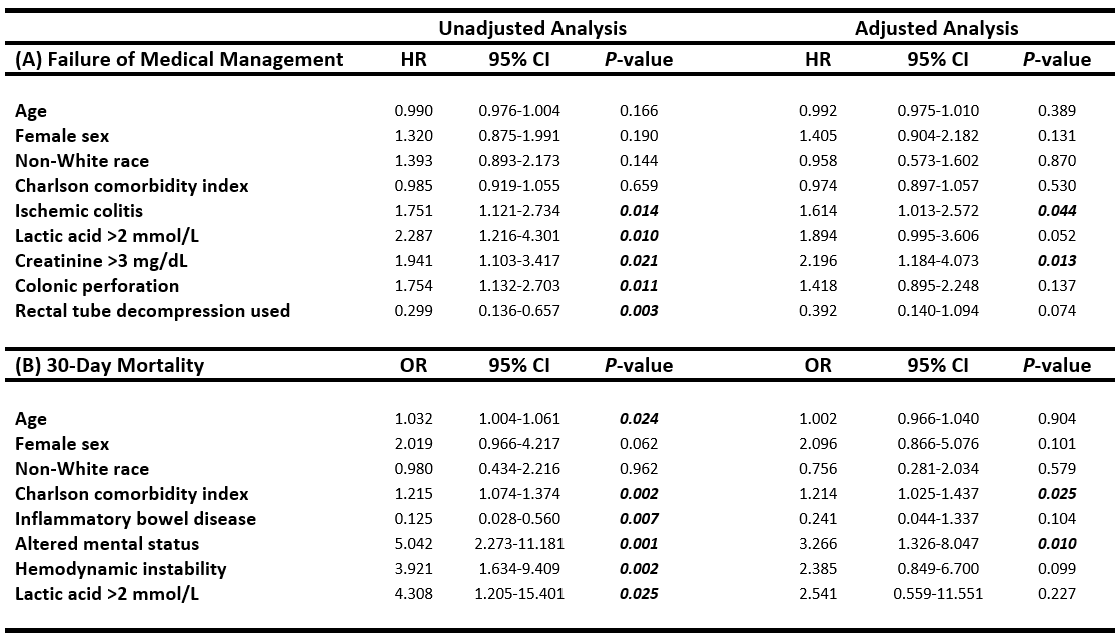
Figure: Table 1. Etiologies of toxic megacolon
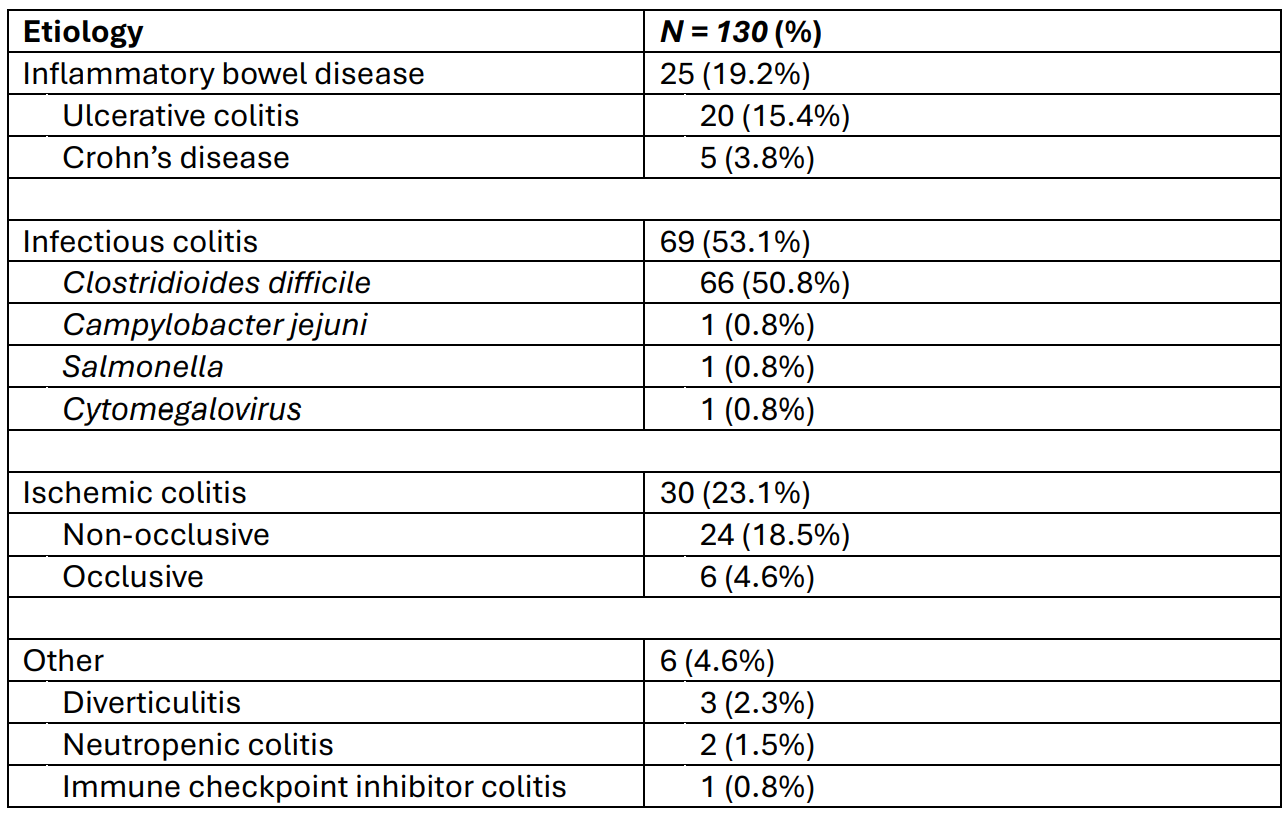
Figure: Table 2. Cox regression (A) and logistic regression (B) analyses identifying factors associated with failure of medical management and 30-day mortality, respectively
Disclosures:
Joseph Gunderson indicated no relevant financial relationships.
David Schaub indicated no relevant financial relationships.
Alisia Gunderson indicated no relevant financial relationships.
Fariba Hossain indicated no relevant financial relationships.
Chiu-Hsieh Hsu indicated no relevant financial relationships.
Sasha Taleban: AbbVie – Grant/Research Support. Boehringer-Ingelheim – Grant/Research Support. Eli Lilly – Grant/Research Support. Janssen – Advisory Committee/Board Member, Grant/Research Support. Pfizer – Grant/Research Support. Takeda – Grant/Research Support.
Joseph Gunderson, MD1, David J. Schaub, MD2, Alisia C. Gunderson, MD1, Fariba Hossain, BS3, Chiu-Hsieh Hsu, PhD4, Sasha Taleban, MD, FACG3. P1085 - Azotemia and Ischemic Colitis Predict Medical Management Failure in Toxic Megacolon, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
