Sunday Poster Session
Category: IBD
P1030 - Evaluating the Key Risk Factors for Crohn’s Disease Flares in a Marginalized Population
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Himaben Gohil, DO, MSc (she/her/hers)
University at Buffalo
Buffalo, NY
Presenting Author(s)
Himaben Gohil, DO, MSc1, Xavier Zonna, DO1, Mark Rayev, DO1, Lan Nguyen, DO1, Alexander Zhu, DO1, Ravneet Kaur, DO2, Erin Ly, MD1
1University at Buffalo, Buffalo, NY; 2University of Buffalo, Buffalo, NY
Introduction: Crohn’s disease is influenced by both genetic and environmental factors. Biochemical factors to psychological factors have been associated with a Crohn’s flare. However, specific factors and their level of influence remain unclear. This study aims to identify potential risk factors for Crohn’s flares in a marginalized population.
Methods: A retrospective chart review was conducted on patients over the age of 18 admitted to a county hospital with Crohn’s flare between January 2019 and May 2024. Data collected included demographics, co-morbidities, medication history, substance use, laboratory values, endoscopic findings, social determinants of health, and inpatient management. Results are presented as the percentage of patients with each risk factor relative to the total cohort.
Results: There were equal proportions of males and females in this study. Most prevalent co-morbidities included anxiety (34%) and depression (26%). Table A shows some commonly implicated risk factors for Crohn’s flares. 53% of patients were on IBD treatment with most being on infliximab (75%). 35% reported non-adherence and 20% failed biologics. 71% reported prior hospitalizations. 63% and 53% of patients who underwent colonoscopy and esophagogastroduodenoscopy respectively had active inflammation. Average inflammatory markers were elevated in this cohort (Table B). Steroids were used for almost all inductions. Infliximab was used for maintenance in 11% of cases. Most patients did not have surgery during admission (83%). The average length of stay was 8 days. 48% of patients were discharged on steroids, and 28% were discharged on a biologic.
Discussion: Most Crohn’s flare patients did not report increased antibiotics, substance, or non-steroidal anti-inflammatory drug use. Many presented with psychosocial stressors, but most patients did not report non-adherence as a result. Most had adequate outpatient care, but progressive disease as evidenced by re-hospitalization rate and active inflammation on admission. Even with access to care, Crohn’s can progress due to biological and psychosocial mechanisms as opposed to modifiable lifestyle factors or non-adherence. However, only 53% of patients were on treatment, indicating care gaps likely due to socioeconomic and psychosocial factors with the hospital primarily serving a marginalized population. Interestingly, only 26% reported economic factors affecting access to care which may also imply health literacy affecting access to care.
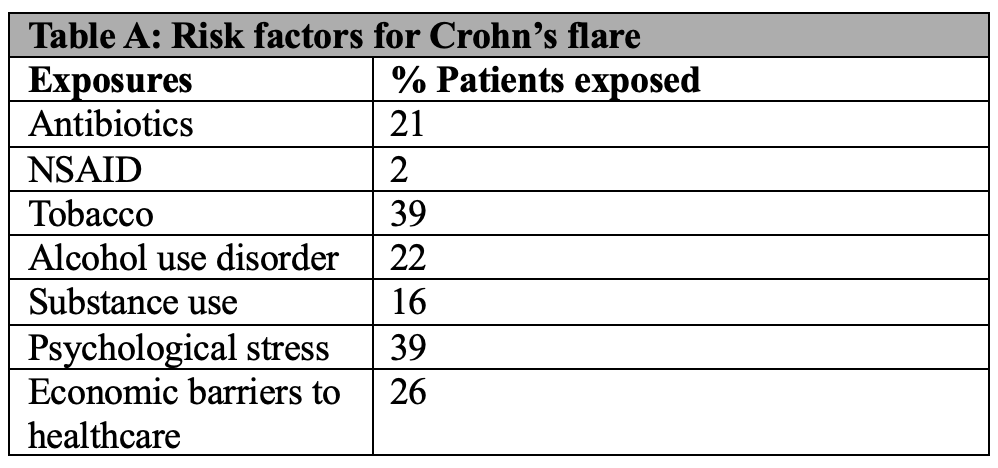
Figure: Table A: Percentage of patients exposed to commonly implicated risk factors for Crohn's flare.
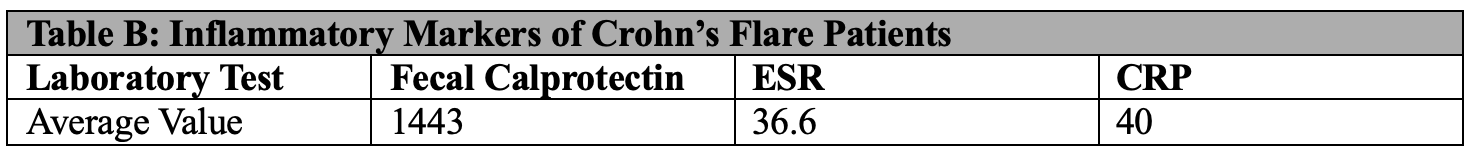
Figure: Table B: Average values of inflammatory markers in patients presenting with a Crohn's flare
Disclosures:
Himaben Gohil indicated no relevant financial relationships.
Xavier Zonna indicated no relevant financial relationships.
Mark Rayev indicated no relevant financial relationships.
Lan Nguyen indicated no relevant financial relationships.
Alexander Zhu indicated no relevant financial relationships.
Ravneet Kaur indicated no relevant financial relationships.
Erin Ly indicated no relevant financial relationships.
Himaben Gohil, DO, MSc1, Xavier Zonna, DO1, Mark Rayev, DO1, Lan Nguyen, DO1, Alexander Zhu, DO1, Ravneet Kaur, DO2, Erin Ly, MD1. P1030 - Evaluating the Key Risk Factors for Crohn’s Disease Flares in a Marginalized Population, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University at Buffalo, Buffalo, NY; 2University of Buffalo, Buffalo, NY
Introduction: Crohn’s disease is influenced by both genetic and environmental factors. Biochemical factors to psychological factors have been associated with a Crohn’s flare. However, specific factors and their level of influence remain unclear. This study aims to identify potential risk factors for Crohn’s flares in a marginalized population.
Methods: A retrospective chart review was conducted on patients over the age of 18 admitted to a county hospital with Crohn’s flare between January 2019 and May 2024. Data collected included demographics, co-morbidities, medication history, substance use, laboratory values, endoscopic findings, social determinants of health, and inpatient management. Results are presented as the percentage of patients with each risk factor relative to the total cohort.
Results: There were equal proportions of males and females in this study. Most prevalent co-morbidities included anxiety (34%) and depression (26%). Table A shows some commonly implicated risk factors for Crohn’s flares. 53% of patients were on IBD treatment with most being on infliximab (75%). 35% reported non-adherence and 20% failed biologics. 71% reported prior hospitalizations. 63% and 53% of patients who underwent colonoscopy and esophagogastroduodenoscopy respectively had active inflammation. Average inflammatory markers were elevated in this cohort (Table B). Steroids were used for almost all inductions. Infliximab was used for maintenance in 11% of cases. Most patients did not have surgery during admission (83%). The average length of stay was 8 days. 48% of patients were discharged on steroids, and 28% were discharged on a biologic.
Discussion: Most Crohn’s flare patients did not report increased antibiotics, substance, or non-steroidal anti-inflammatory drug use. Many presented with psychosocial stressors, but most patients did not report non-adherence as a result. Most had adequate outpatient care, but progressive disease as evidenced by re-hospitalization rate and active inflammation on admission. Even with access to care, Crohn’s can progress due to biological and psychosocial mechanisms as opposed to modifiable lifestyle factors or non-adherence. However, only 53% of patients were on treatment, indicating care gaps likely due to socioeconomic and psychosocial factors with the hospital primarily serving a marginalized population. Interestingly, only 26% reported economic factors affecting access to care which may also imply health literacy affecting access to care.
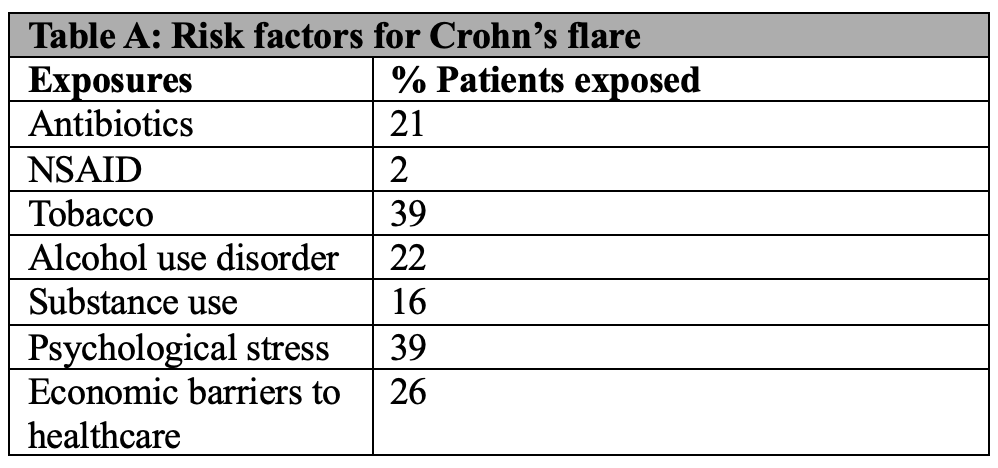
Figure: Table A: Percentage of patients exposed to commonly implicated risk factors for Crohn's flare.
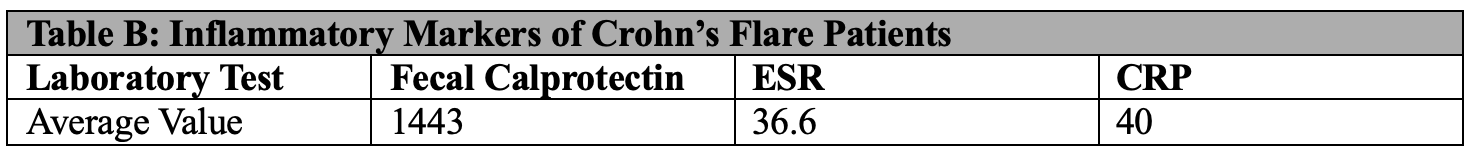
Figure: Table B: Average values of inflammatory markers in patients presenting with a Crohn's flare
Disclosures:
Himaben Gohil indicated no relevant financial relationships.
Xavier Zonna indicated no relevant financial relationships.
Mark Rayev indicated no relevant financial relationships.
Lan Nguyen indicated no relevant financial relationships.
Alexander Zhu indicated no relevant financial relationships.
Ravneet Kaur indicated no relevant financial relationships.
Erin Ly indicated no relevant financial relationships.
Himaben Gohil, DO, MSc1, Xavier Zonna, DO1, Mark Rayev, DO1, Lan Nguyen, DO1, Alexander Zhu, DO1, Ravneet Kaur, DO2, Erin Ly, MD1. P1030 - Evaluating the Key Risk Factors for Crohn’s Disease Flares in a Marginalized Population, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
