Sunday Poster Session
Category: IBD
P1022 - Should We Use Clinical Indices to Screen Symptomatic Patients With Endoscopically Quiescent Crohn’s Disease?
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Carl Samaha, MD
University of Pittsburgh
Pittsburgh, PA
Presenting Author(s)
Carl Samaha, MD1, Logan Slade, PA1, Jeffrey M. Dueker, MD, MPH1, Elyse Johnston, MD1, David Binion, MD2, Marc Schwartz, MD1, Richard Duerr, MD1
1University of Pittsburgh, Pittsburgh, PA; 2University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: Patients with Crohn’s Disease (CD) commonly report gastrointestinal (GI) symptoms despite endoscopic remission. Symptom-based tools are often used to characterize clinical remission but their utility in identifying functional impairment remains uncertain. We aimed to evaluate the burden of moderate-to-severe GI symptoms in endoscopically quiescent CD and compare the performance of sCDAI, PRO2, and ROME IV criteria in classifying patients with disruptions in daily functioning.
Methods: We retrospectively analyzed patient-reported symptoms and healthcare utilization from 112 patients with CD in endoscopic remission or near-remission (SES-CD 0-6) enrolled in the SPARC-IBD study. Patients were stratified by the presence of moderate-severe GI symptom (Abdominal pain, Frequency, Liquid stools, Urgency), sCDAI and PRO2 category, and ROME IV criteria. Logistic regression was used to assess the association between symptoms severity, clinical indices and wellbeing, work absenteeism, emergency department (ED) visits and hospitalizations. For each clinical burden indicator, we descriptively reported the proportion of affected patients identified by ROME IV, PRO2, and sCDAI.
Results: 43% of patients reported moderate-to-severe GI symptoms, yet only 20% met ROME IV criteria, 13% were classified as ‘Moderate’ and none as ‘Severe’ by PRO2 and sCDAI. In univariate analysis, moderate-to-severe symptoms were associated with poor wellbeing, work absenteeism, and recent ED visits (all p< 0.05) but not hospitalizations. Multivariate analysis confirmed poor wellbeing (OR 2.8, p=0.01) and work absenteeism (OR 4.0, p=0.006) as independently associated with moderate-to-severe symptoms after adjusting for sex, SES-CD, phenotype, and prior resection. These associations were replicated for ROME IV criteria (OR 3.7 and 7.0, respectively) and ‘Moderate’ PRO2 (OR 4.7 and 13.8, respectively) but not sCDAI category. Importantly, Rome IV criteria identified 33-70% of patients with clinical burden indicators while PRO2 captured 22-73% of these patients. sCDAI had the worst performance (22% to 50%) among indices.
Discussion: In patients with endoscopically quiescent CD, sCDAI was not associated with wellbeing and healthcare utilization and failed to capture most patients with clinically significant burden. PRO2 and ROME IV performed better but still missed a substantial proportion of symptomatic patients. These findings suggest the need for patient-centered tools that better predict functional impairment in this setting.
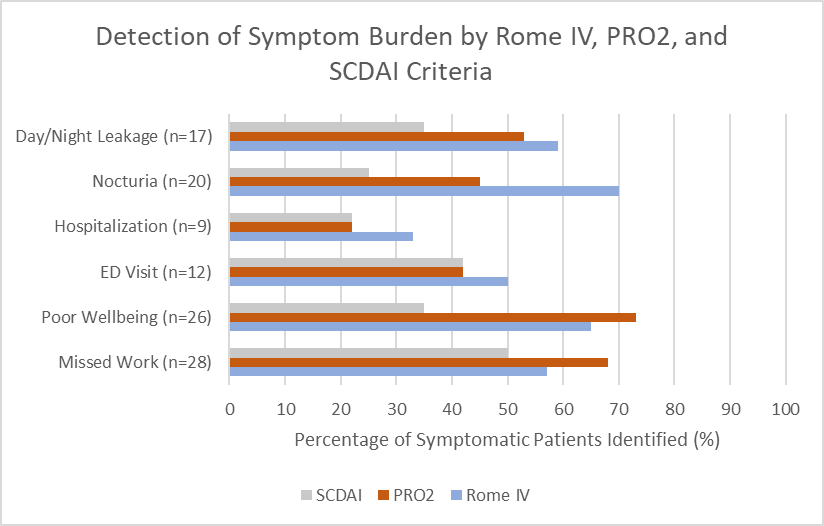
Figure: Detection of Symptom Burden by Rome IV, PRO2, and sCDAI Criteria
Disclosures:
Carl Samaha indicated no relevant financial relationships.
Logan Slade indicated no relevant financial relationships.
Jeffrey Dueker indicated no relevant financial relationships.
Elyse Johnston indicated no relevant financial relationships.
David Binion: Blueprint Medicines – Grant/Research Support. Mirador Therapeutics – Grant/Research Support. Takeda – Grant/Research Support.
Marc Schwartz indicated no relevant financial relationships.
Richard Duerr indicated no relevant financial relationships.
Carl Samaha, MD1, Logan Slade, PA1, Jeffrey M. Dueker, MD, MPH1, Elyse Johnston, MD1, David Binion, MD2, Marc Schwartz, MD1, Richard Duerr, MD1. P1022 - Should We Use Clinical Indices to Screen Symptomatic Patients With Endoscopically Quiescent Crohn’s Disease?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Pittsburgh, Pittsburgh, PA; 2University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: Patients with Crohn’s Disease (CD) commonly report gastrointestinal (GI) symptoms despite endoscopic remission. Symptom-based tools are often used to characterize clinical remission but their utility in identifying functional impairment remains uncertain. We aimed to evaluate the burden of moderate-to-severe GI symptoms in endoscopically quiescent CD and compare the performance of sCDAI, PRO2, and ROME IV criteria in classifying patients with disruptions in daily functioning.
Methods: We retrospectively analyzed patient-reported symptoms and healthcare utilization from 112 patients with CD in endoscopic remission or near-remission (SES-CD 0-6) enrolled in the SPARC-IBD study. Patients were stratified by the presence of moderate-severe GI symptom (Abdominal pain, Frequency, Liquid stools, Urgency), sCDAI and PRO2 category, and ROME IV criteria. Logistic regression was used to assess the association between symptoms severity, clinical indices and wellbeing, work absenteeism, emergency department (ED) visits and hospitalizations. For each clinical burden indicator, we descriptively reported the proportion of affected patients identified by ROME IV, PRO2, and sCDAI.
Results: 43% of patients reported moderate-to-severe GI symptoms, yet only 20% met ROME IV criteria, 13% were classified as ‘Moderate’ and none as ‘Severe’ by PRO2 and sCDAI. In univariate analysis, moderate-to-severe symptoms were associated with poor wellbeing, work absenteeism, and recent ED visits (all p< 0.05) but not hospitalizations. Multivariate analysis confirmed poor wellbeing (OR 2.8, p=0.01) and work absenteeism (OR 4.0, p=0.006) as independently associated with moderate-to-severe symptoms after adjusting for sex, SES-CD, phenotype, and prior resection. These associations were replicated for ROME IV criteria (OR 3.7 and 7.0, respectively) and ‘Moderate’ PRO2 (OR 4.7 and 13.8, respectively) but not sCDAI category. Importantly, Rome IV criteria identified 33-70% of patients with clinical burden indicators while PRO2 captured 22-73% of these patients. sCDAI had the worst performance (22% to 50%) among indices.
Discussion: In patients with endoscopically quiescent CD, sCDAI was not associated with wellbeing and healthcare utilization and failed to capture most patients with clinically significant burden. PRO2 and ROME IV performed better but still missed a substantial proportion of symptomatic patients. These findings suggest the need for patient-centered tools that better predict functional impairment in this setting.
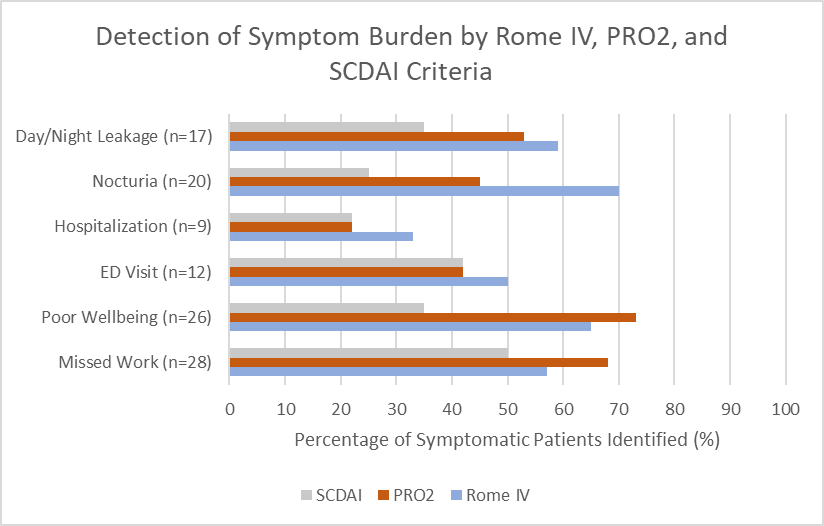
Figure: Detection of Symptom Burden by Rome IV, PRO2, and sCDAI Criteria
Disclosures:
Carl Samaha indicated no relevant financial relationships.
Logan Slade indicated no relevant financial relationships.
Jeffrey Dueker indicated no relevant financial relationships.
Elyse Johnston indicated no relevant financial relationships.
David Binion: Blueprint Medicines – Grant/Research Support. Mirador Therapeutics – Grant/Research Support. Takeda – Grant/Research Support.
Marc Schwartz indicated no relevant financial relationships.
Richard Duerr indicated no relevant financial relationships.
Carl Samaha, MD1, Logan Slade, PA1, Jeffrey M. Dueker, MD, MPH1, Elyse Johnston, MD1, David Binion, MD2, Marc Schwartz, MD1, Richard Duerr, MD1. P1022 - Should We Use Clinical Indices to Screen Symptomatic Patients With Endoscopically Quiescent Crohn’s Disease?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

