Sunday Poster Session
Category: GI Bleeding
P1010 - Upper GI Bleed: A Rare Presentation of Gastric Syphilis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Fredella Lee, MD (she/her/hers)
NewYork-Presbyterian / Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Fredella Lee, MD, Lillian F. Zhang, MD, PhD, Eliza Cricco-Lizza, MD, Michelle Cohen, MD, Annika Windon, MD, Evan Grossman, MD
NewYork-Presbyterian / Weill Cornell Medical Center, New York, NY
Introduction: Syphilis, a sexually transmitted infection caused by Treponema pallidum, is most recognized during its primary stage, with a genital chancre as its presenting symptom. However, secondary syphilis can affect any organ via hematogenous dissemination. We present a rare case of an upper gastrointestinal bleed in the setting of gastric syphilis, an uncommon extracutaneous manifestation of syphilis that occurs < 1% in patients.
Case Description/
Methods: A 37-year-old female, with fibromyalgia, asthma, and history of Lyme disease in 2013, presented with 3 days of epigastric pain, melena, and hematemesis that precipitated a syncopal event. She denied smoking, or use of alcohol, anticoagulants, or steroids, but did take ibuprofen occasionally. On presentation, she was hemodynamically stable and her exam revealed a soft abdomen with tenderness across the epigastrium but without peritoneal signs. Labs showed a hemoglobin of 7.7 g/dL from her baseline of 10.5 g/dL. Given concern for an upper gastrointestinal bleed (UGIB), an esophagogastroduodenoscopy (EGD) was performed. It showed severe congestion, erosions, and nodularity of the entire stomach, a 15-mm cratered ulcer with a visible vessel in the incisura treated with epinephrine and cauterization, and a clean based duodenal bulb ulcer. She was treated with a proton pump inhibitor and discharged on hospital day 4, as there was no further bleeding. Gastric biopsies of the incisura revealed dense lymphoid proliferation (polyclonal pattern), chronic active gastritis, and immunoreactivity for spirochetes. Further testing for spirochete associated diseases revealed absence of lyme antibodies, a rapid plasma reagin (RPR) titer of 1:32, and presence of treponema pallidum antibodies, consistent with gastric syphilis. Due to eye pain, changes in visual acuity, and paresthesias, she was treated for presumed neurosyphilis with 14 days of IV penicillin G 24 million units/day. After treatment, repeat EGD to confirm ulcer healing showed patchy gastric discoloration and a healing of the ulcers. Pathology re-demonstrated chronic gastritis with negative spirochete immunostain.
Discussion: Gastric syphilis is a rare cause for an UGIB and the majority of patients do not have a genital ulcer, inguinal lymphadenopathy, or rash on presentation. The endoscopic findings can mimic gastric cancer, lymphoma, or Crohn’s disease, and thus, immunohistochemistry is an invaluable tool for the diagnosis and treatment to minimize progression to late-stage or tertiary syphilis.
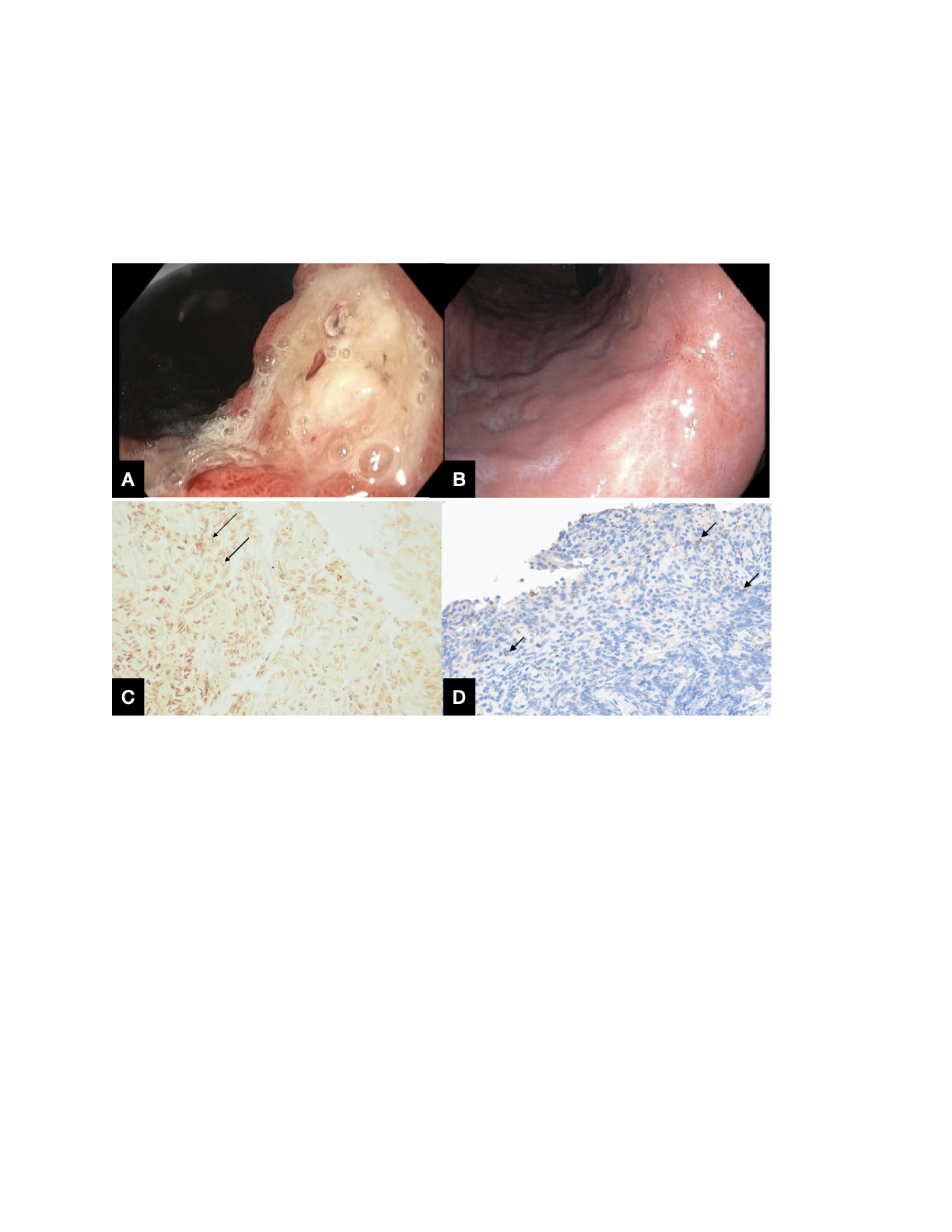
Figure: Figure A demonstrates a 15-mm ulcer with a visible vessel at the gastric incisura. Figure B demonstrates a healed ulcer at the gastric incisura after treatment with IV penicilln. Figure C demonstrates the presence of spirochetes (indicated by arrows) in the incisura using Steiner Stain. Figure D demonstrates presence of spirochetes (indicated by arrows) in the incisura with the Spirochete Immunostain.
Disclosures:
Fredella Lee indicated no relevant financial relationships.
Lillian Zhang indicated no relevant financial relationships.
Eliza Cricco-Lizza indicated no relevant financial relationships.
Michelle Cohen indicated no relevant financial relationships.
Annika Windon indicated no relevant financial relationships.
Evan Grossman indicated no relevant financial relationships.
Fredella Lee, MD, Lillian F. Zhang, MD, PhD, Eliza Cricco-Lizza, MD, Michelle Cohen, MD, Annika Windon, MD, Evan Grossman, MD. P1010 - Upper GI Bleed: A Rare Presentation of Gastric Syphilis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
NewYork-Presbyterian / Weill Cornell Medical Center, New York, NY
Introduction: Syphilis, a sexually transmitted infection caused by Treponema pallidum, is most recognized during its primary stage, with a genital chancre as its presenting symptom. However, secondary syphilis can affect any organ via hematogenous dissemination. We present a rare case of an upper gastrointestinal bleed in the setting of gastric syphilis, an uncommon extracutaneous manifestation of syphilis that occurs < 1% in patients.
Case Description/
Methods: A 37-year-old female, with fibromyalgia, asthma, and history of Lyme disease in 2013, presented with 3 days of epigastric pain, melena, and hematemesis that precipitated a syncopal event. She denied smoking, or use of alcohol, anticoagulants, or steroids, but did take ibuprofen occasionally. On presentation, she was hemodynamically stable and her exam revealed a soft abdomen with tenderness across the epigastrium but without peritoneal signs. Labs showed a hemoglobin of 7.7 g/dL from her baseline of 10.5 g/dL. Given concern for an upper gastrointestinal bleed (UGIB), an esophagogastroduodenoscopy (EGD) was performed. It showed severe congestion, erosions, and nodularity of the entire stomach, a 15-mm cratered ulcer with a visible vessel in the incisura treated with epinephrine and cauterization, and a clean based duodenal bulb ulcer. She was treated with a proton pump inhibitor and discharged on hospital day 4, as there was no further bleeding. Gastric biopsies of the incisura revealed dense lymphoid proliferation (polyclonal pattern), chronic active gastritis, and immunoreactivity for spirochetes. Further testing for spirochete associated diseases revealed absence of lyme antibodies, a rapid plasma reagin (RPR) titer of 1:32, and presence of treponema pallidum antibodies, consistent with gastric syphilis. Due to eye pain, changes in visual acuity, and paresthesias, she was treated for presumed neurosyphilis with 14 days of IV penicillin G 24 million units/day. After treatment, repeat EGD to confirm ulcer healing showed patchy gastric discoloration and a healing of the ulcers. Pathology re-demonstrated chronic gastritis with negative spirochete immunostain.
Discussion: Gastric syphilis is a rare cause for an UGIB and the majority of patients do not have a genital ulcer, inguinal lymphadenopathy, or rash on presentation. The endoscopic findings can mimic gastric cancer, lymphoma, or Crohn’s disease, and thus, immunohistochemistry is an invaluable tool for the diagnosis and treatment to minimize progression to late-stage or tertiary syphilis.
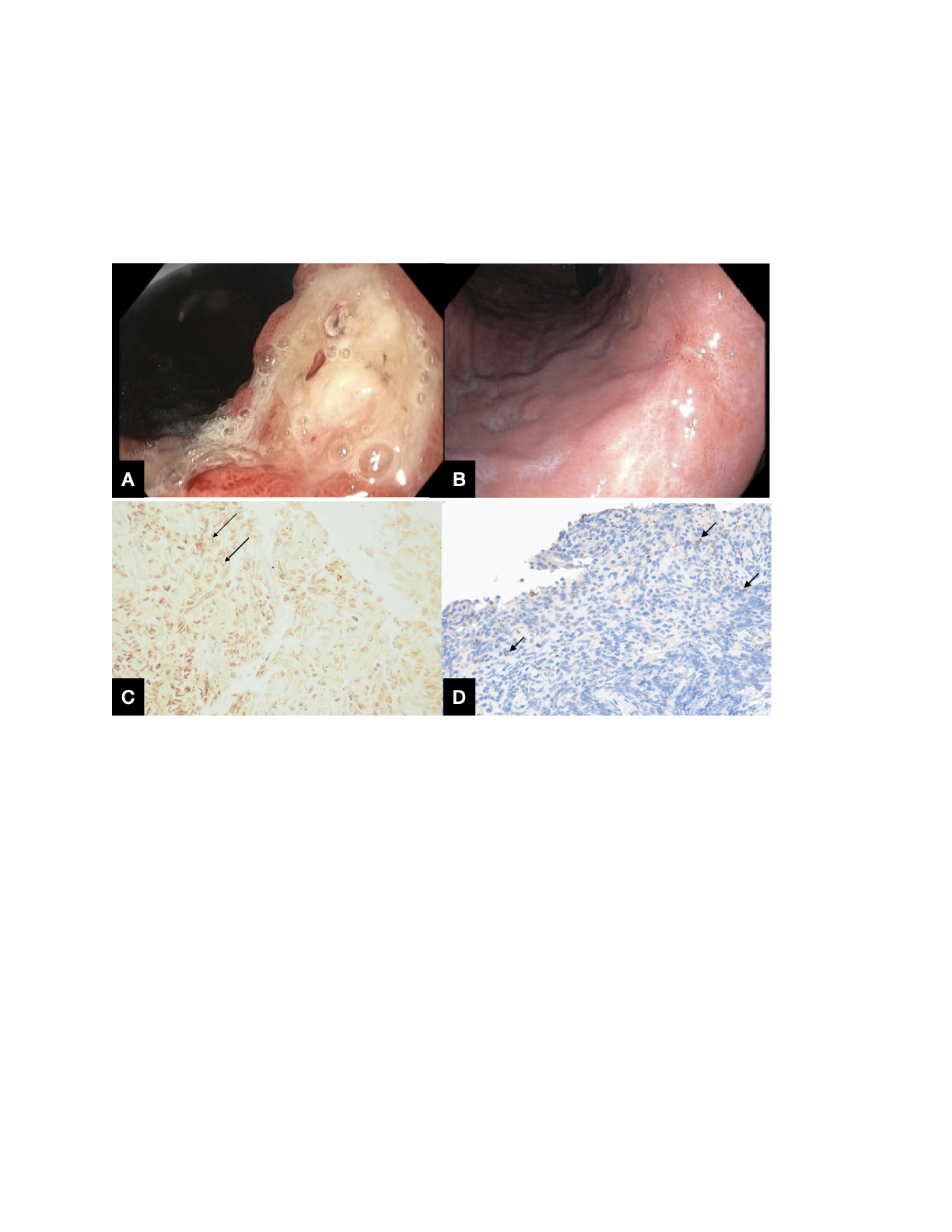
Figure: Figure A demonstrates a 15-mm ulcer with a visible vessel at the gastric incisura. Figure B demonstrates a healed ulcer at the gastric incisura after treatment with IV penicilln. Figure C demonstrates the presence of spirochetes (indicated by arrows) in the incisura using Steiner Stain. Figure D demonstrates presence of spirochetes (indicated by arrows) in the incisura with the Spirochete Immunostain.
Disclosures:
Fredella Lee indicated no relevant financial relationships.
Lillian Zhang indicated no relevant financial relationships.
Eliza Cricco-Lizza indicated no relevant financial relationships.
Michelle Cohen indicated no relevant financial relationships.
Annika Windon indicated no relevant financial relationships.
Evan Grossman indicated no relevant financial relationships.
Fredella Lee, MD, Lillian F. Zhang, MD, PhD, Eliza Cricco-Lizza, MD, Michelle Cohen, MD, Annika Windon, MD, Evan Grossman, MD. P1010 - Upper GI Bleed: A Rare Presentation of Gastric Syphilis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
