Sunday Poster Session
Category: GI Bleeding
P1006 - Dual Arteries, Dual Threat: Managing Refractory Duodenal Ulcer Bleeding Secondary to a Duplicated Gastroduodenal Artery
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Maitri Shah, MD (she/her/hers)
University of Michigan Health - Sparrow
East Lansing, MI
Presenting Author(s)
Maitri Shah, MD1, Amey Joshi, MD1, Adarsh Kumar. Jha, MD1, Shreeya kumar. Adhikari, MD1, Divij K. Jha, MD1, Rutwik Pradeep. Sharma, MD2, Abhishek Satishchandran, MD, PhD3
1University of Michigan Health - Sparrow, Lansing, MI; 2University of Michigan-Sparrow Hospital, Lansing, MI; 3University of Michigan, Lansing, MI
Introduction: Fatal upper gastrointestinal bleeding (UGIB) from duodenal ulcers typically requires both endoscopic and interventional treatment. The gastroduodenal artery (GDA) is the most commonly involved vessel in posterior duodenal ulcer bleeding. Duplication of the GDA is an uncommon vascular anomaly present in ~1.1% of the population. Bleeding may persist despite standard treatments if such anomalies go undetected. We describe a unique case of refractory duodenal ulcer bleeding successfully treated by dual micro-coil embolization of a duplicated GDA.
Case Description/
Methods: A 63-year-old female with post-stroke epilepsy presented with fatigue, dizziness, and abdominal pain. She was admitted for pyometra and underwent hysteroscopy and D&C, after which she developed hemorrhagic shock due to hematochezia. EGD revealed LA Grade D esophagitis and old blood in the stomach and duodenum. A 2–3 cm ulcer with visible vessels was seen in the second portion, and a 1.5 cm ulcer with a partially visible vessel was noted in the bulb. Hemostasis with epinephrine and bipolar cautery was unsuccessful due to location. Given concern for GDA-territory bleeding, interventional radiology (IR) performed emergent mesenteric angiography, revealing a duplicated GDA. Both branches were embolized using four Tornado micro-coils, resulting in hemodynamic stabilization and cessation of bleeding. The patient later developed duodenal perforation requiring laparotomy and antrectomy and ultimately succumbed to septic complications.
Discussion: The GDA, a branch of the common hepatic artery, runs posterior to the duodenum and commonly contributes to life-threatening bleeds from posterior duodenal ulcers. Endoscopic therapy typically includes injection (e.g., epinephrine), thermal (e.g. bipolar), and mechanical (clips). Success depends on ulcer visibility and access, which can be limited by location/clot burden. In cases where endoscopy fails, angiographic embolization is needed. Standard GDA embolization involves coiling proximal and distal to the bleed. However, in rare variants like a duplicated GDA, failure to identify and embolize all branches may lead to persistent bleeding. This case highlights the need for high clinical suspicion, angiographic mapping, and interdisciplinary approach in managing refractory bleed. Duplicate GDA, though rare, must be considered in recurrent duodenal ulcer bleed. Early IR involvement is key. Hemostasis relies on identifying and embolizing all feeding vessels, including rare variants.
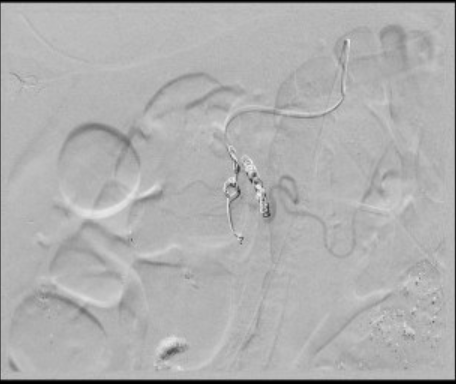
Figure: Lateral and medial branch of gastroduodenal artery
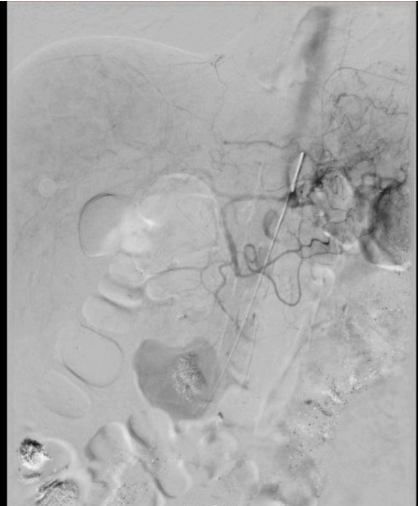
Figure: Lateral GDA with smaller micro-coil, Medial GDA with larger micro-coil
Disclosures:
Maitri Shah indicated no relevant financial relationships.
Amey Joshi indicated no relevant financial relationships.
Adarsh Jha indicated no relevant financial relationships.
Shreeya Adhikari indicated no relevant financial relationships.
Divij Jha indicated no relevant financial relationships.
Rutwik Sharma indicated no relevant financial relationships.
Abhishek Satishchandran indicated no relevant financial relationships.
Maitri Shah, MD1, Amey Joshi, MD1, Adarsh Kumar. Jha, MD1, Shreeya kumar. Adhikari, MD1, Divij K. Jha, MD1, Rutwik Pradeep. Sharma, MD2, Abhishek Satishchandran, MD, PhD3. P1006 - Dual Arteries, Dual Threat: Managing Refractory Duodenal Ulcer Bleeding Secondary to a Duplicated Gastroduodenal Artery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Michigan Health - Sparrow, Lansing, MI; 2University of Michigan-Sparrow Hospital, Lansing, MI; 3University of Michigan, Lansing, MI
Introduction: Fatal upper gastrointestinal bleeding (UGIB) from duodenal ulcers typically requires both endoscopic and interventional treatment. The gastroduodenal artery (GDA) is the most commonly involved vessel in posterior duodenal ulcer bleeding. Duplication of the GDA is an uncommon vascular anomaly present in ~1.1% of the population. Bleeding may persist despite standard treatments if such anomalies go undetected. We describe a unique case of refractory duodenal ulcer bleeding successfully treated by dual micro-coil embolization of a duplicated GDA.
Case Description/
Methods: A 63-year-old female with post-stroke epilepsy presented with fatigue, dizziness, and abdominal pain. She was admitted for pyometra and underwent hysteroscopy and D&C, after which she developed hemorrhagic shock due to hematochezia. EGD revealed LA Grade D esophagitis and old blood in the stomach and duodenum. A 2–3 cm ulcer with visible vessels was seen in the second portion, and a 1.5 cm ulcer with a partially visible vessel was noted in the bulb. Hemostasis with epinephrine and bipolar cautery was unsuccessful due to location. Given concern for GDA-territory bleeding, interventional radiology (IR) performed emergent mesenteric angiography, revealing a duplicated GDA. Both branches were embolized using four Tornado micro-coils, resulting in hemodynamic stabilization and cessation of bleeding. The patient later developed duodenal perforation requiring laparotomy and antrectomy and ultimately succumbed to septic complications.
Discussion: The GDA, a branch of the common hepatic artery, runs posterior to the duodenum and commonly contributes to life-threatening bleeds from posterior duodenal ulcers. Endoscopic therapy typically includes injection (e.g., epinephrine), thermal (e.g. bipolar), and mechanical (clips). Success depends on ulcer visibility and access, which can be limited by location/clot burden. In cases where endoscopy fails, angiographic embolization is needed. Standard GDA embolization involves coiling proximal and distal to the bleed. However, in rare variants like a duplicated GDA, failure to identify and embolize all branches may lead to persistent bleeding. This case highlights the need for high clinical suspicion, angiographic mapping, and interdisciplinary approach in managing refractory bleed. Duplicate GDA, though rare, must be considered in recurrent duodenal ulcer bleed. Early IR involvement is key. Hemostasis relies on identifying and embolizing all feeding vessels, including rare variants.
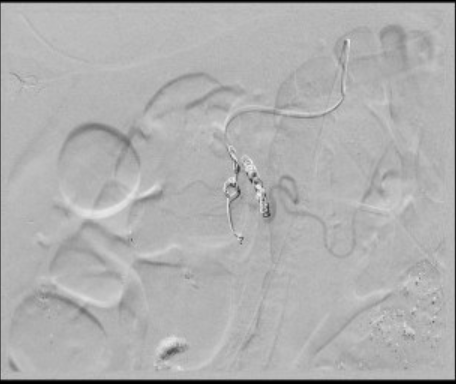
Figure: Lateral and medial branch of gastroduodenal artery
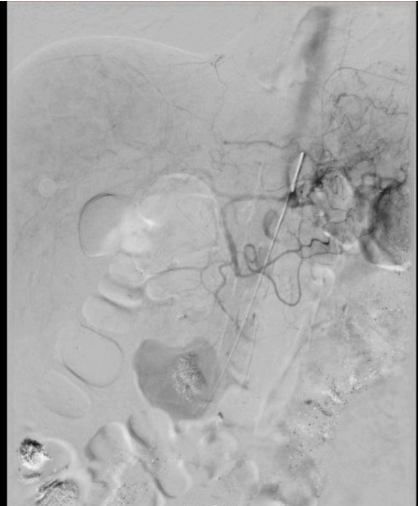
Figure: Lateral GDA with smaller micro-coil, Medial GDA with larger micro-coil
Disclosures:
Maitri Shah indicated no relevant financial relationships.
Amey Joshi indicated no relevant financial relationships.
Adarsh Jha indicated no relevant financial relationships.
Shreeya Adhikari indicated no relevant financial relationships.
Divij Jha indicated no relevant financial relationships.
Rutwik Sharma indicated no relevant financial relationships.
Abhishek Satishchandran indicated no relevant financial relationships.
Maitri Shah, MD1, Amey Joshi, MD1, Adarsh Kumar. Jha, MD1, Shreeya kumar. Adhikari, MD1, Divij K. Jha, MD1, Rutwik Pradeep. Sharma, MD2, Abhishek Satishchandran, MD, PhD3. P1006 - Dual Arteries, Dual Threat: Managing Refractory Duodenal Ulcer Bleeding Secondary to a Duplicated Gastroduodenal Artery, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
