Sunday Poster Session
Category: GI Bleeding
P0997 - Hidden in Plain Stoma: Unmasking Parastomal Varices as a Source of Obscure GI Bleeding
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ingrid Rocha, BS (she/her/hers)
Wayne State School of Medicine
Detroit, MI
Presenting Author(s)
Ingrid Rocha, BS1, Suraj Suresh, MD2
1Wayne State School of Medicine, Detroit, MI; 2Henry Ford Health, Detroit, MI
Introduction: Parastomal varices (PSV) are an uncommon complication of portal hypertension, seen in up to 5% of patients with a stoma. Due to their variable appearance and lack of specific symptoms, diagnosis is often delayed, especially in patients with recurrent gastrointestinal (GI) bleeding. Characteristic findings such as stomal discoloration or dilated submucosal veins are infrequently seen. When endoscopy is non-diagnostic, imaging such as contrast venography may be necessary. Management options include local therapy, transjugular intrahepatic portosystemic shunt (TIPS), balloon-occluded retrograde transvenous obliteration (BRTO), and embolization. This case highlights the diagnostic challenge of PSV and the effective use of BRTO as a minimally invasive treatment approach.
Case Description/
Methods: A 59-year-old male with Crohn’s disease status post ileostomy and rectal pouch, MASH cirrhosis, and myelodysplastic syndrome was admitted with several months of recurrent bright red blooding per ostomy. Hemoglobin on presentation was 6.7 g/dL. Prior endoscopy revealed portal hypertensive gastropathy and small bowel arteriovenous malformations treated with argon plasma coagulation. Despite further testing including tagged RBC scan, capsule endoscopy, and push enteroscopy, the bleeding source remained unclear. Ultimately, a more detailed examination allowed for localization of bleeding to the site of the ostomy itself. Bedside cauterization with silver nitrate was ineffective. Interventional radiology was consulted, and venography revealed a portosystemic gradient of 15 mmHg. Coil embolization of a parastomal varix via BRTO was performed, resulting in complete resolution of GI bleeding.
Discussion: This case underscores PSV as a rare but important cause of obscure GI bleeding in patients with portal hypertension and an ostomy. Diagnosis requires high suspicion and appropriate imaging when conventional endoscopy is unrevealing. While local therapies and TIPS have been the mainstay of treatment, this case demonstrates the successful use of BRTO, a minimally invasive alternative with favorable outcomes. Given its efficacy and safety profile, BRTO should be considered in select patients with PSV, particularly when other interventions are contraindicated or have failed.
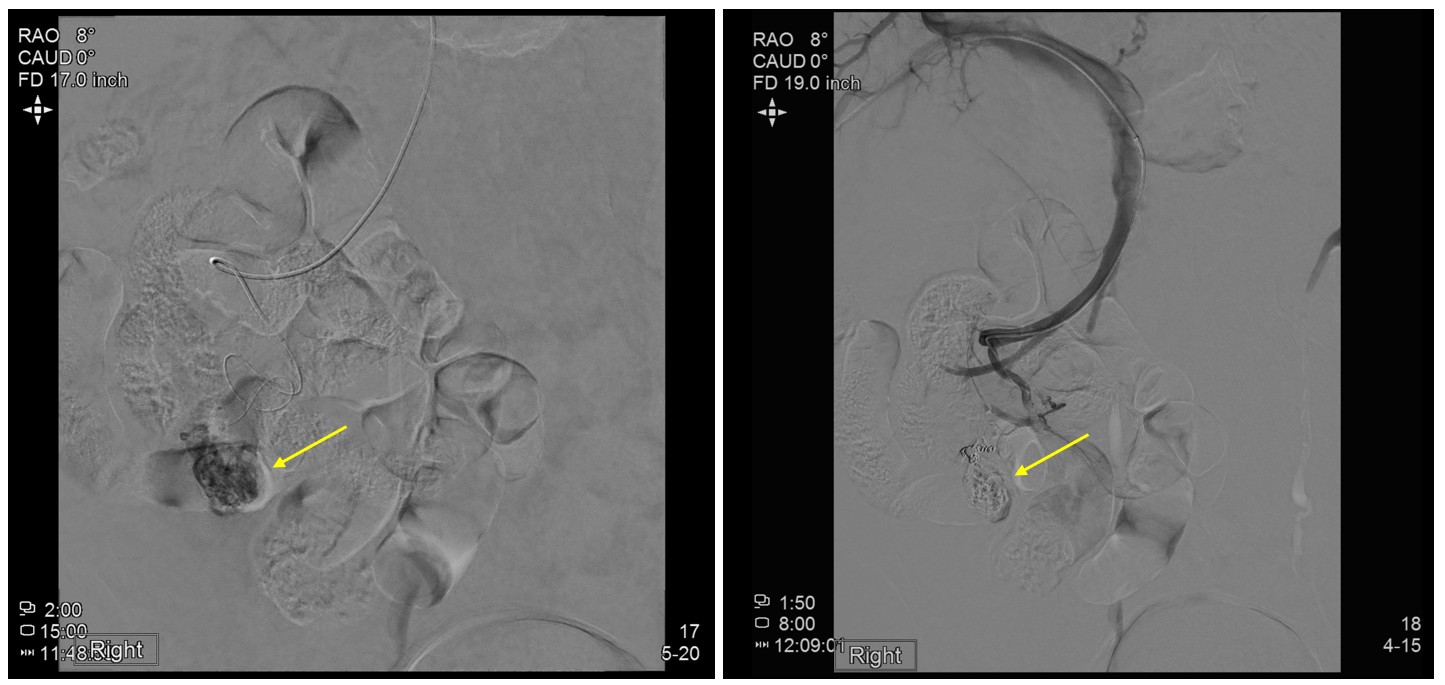
Figure: Figure 1: Digital subtraction angiography demonstrates parastomal varices near the ostomy site prior to embolization (left), with successful occlusion of the dilated vessels following treatment with Sotradecol/lipiodol foam and coil embolization (right).
Disclosures:
Ingrid Rocha indicated no relevant financial relationships.
Suraj Suresh indicated no relevant financial relationships.
Ingrid Rocha, BS1, Suraj Suresh, MD2. P0997 - Hidden in Plain Stoma: Unmasking Parastomal Varices as a Source of Obscure GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Wayne State School of Medicine, Detroit, MI; 2Henry Ford Health, Detroit, MI
Introduction: Parastomal varices (PSV) are an uncommon complication of portal hypertension, seen in up to 5% of patients with a stoma. Due to their variable appearance and lack of specific symptoms, diagnosis is often delayed, especially in patients with recurrent gastrointestinal (GI) bleeding. Characteristic findings such as stomal discoloration or dilated submucosal veins are infrequently seen. When endoscopy is non-diagnostic, imaging such as contrast venography may be necessary. Management options include local therapy, transjugular intrahepatic portosystemic shunt (TIPS), balloon-occluded retrograde transvenous obliteration (BRTO), and embolization. This case highlights the diagnostic challenge of PSV and the effective use of BRTO as a minimally invasive treatment approach.
Case Description/
Methods: A 59-year-old male with Crohn’s disease status post ileostomy and rectal pouch, MASH cirrhosis, and myelodysplastic syndrome was admitted with several months of recurrent bright red blooding per ostomy. Hemoglobin on presentation was 6.7 g/dL. Prior endoscopy revealed portal hypertensive gastropathy and small bowel arteriovenous malformations treated with argon plasma coagulation. Despite further testing including tagged RBC scan, capsule endoscopy, and push enteroscopy, the bleeding source remained unclear. Ultimately, a more detailed examination allowed for localization of bleeding to the site of the ostomy itself. Bedside cauterization with silver nitrate was ineffective. Interventional radiology was consulted, and venography revealed a portosystemic gradient of 15 mmHg. Coil embolization of a parastomal varix via BRTO was performed, resulting in complete resolution of GI bleeding.
Discussion: This case underscores PSV as a rare but important cause of obscure GI bleeding in patients with portal hypertension and an ostomy. Diagnosis requires high suspicion and appropriate imaging when conventional endoscopy is unrevealing. While local therapies and TIPS have been the mainstay of treatment, this case demonstrates the successful use of BRTO, a minimally invasive alternative with favorable outcomes. Given its efficacy and safety profile, BRTO should be considered in select patients with PSV, particularly when other interventions are contraindicated or have failed.
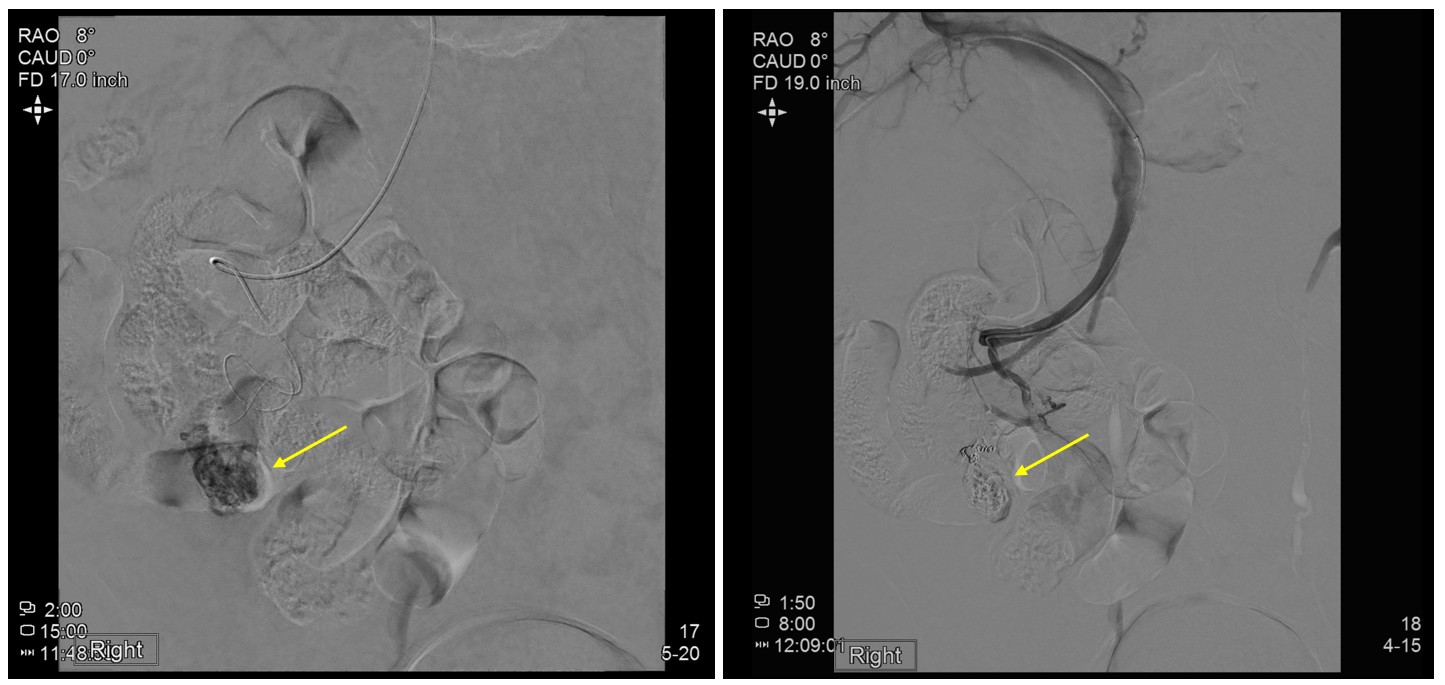
Figure: Figure 1: Digital subtraction angiography demonstrates parastomal varices near the ostomy site prior to embolization (left), with successful occlusion of the dilated vessels following treatment with Sotradecol/lipiodol foam and coil embolization (right).
Disclosures:
Ingrid Rocha indicated no relevant financial relationships.
Suraj Suresh indicated no relevant financial relationships.
Ingrid Rocha, BS1, Suraj Suresh, MD2. P0997 - Hidden in Plain Stoma: Unmasking Parastomal Varices as a Source of Obscure GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
