Sunday Poster Session
Category: GI Bleeding
P0993 - Beyond the Usual Suspects: When Intermittent Melena Heralds a Life-Threatening Dieulafoy Lesion
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- FM
Farirai Melania Marwizi, MD (she/her/hers)
Episcopal Health Services
Queens, NY
Presenting Author(s)
Farirai Melania Marwizi, MD1, Olanrewaju Adeniran, MD2, Abidemi Akinrinmade, MBBS3, Ifeoma P. Kwentoh, MD4, Shekwonya Damaris. Sakoma, MD5, Adela Damm, MD6
1Episcopal Health Services, Queens, NY; 2West Virginia University Morgantown, Morgantown, WV; 3University of Pittsburgh Medical Center, Monroeville, PA; 4New York Institute of Technology College of Osteopathic Medicine, Kent, CT; 5Jersey City Medical Center, Jersey City, NJ; 6University of Medicine and Pharmacy 'Victor Babes', Timisoara, Hermitage, TN
Introduction: Dieulafoy lesions (DLs) are a rare cause of gastrointestinal (GI) bleeding due to erosion of an aberrant submucosal artery extending to the mucosa. We present a case of an adult with no apparent risk factors who developed life threatening, refractory GI bleeding due to a Dieulafoy lesion.
Case Description/
Methods: 38-year old male presented to the emergency department (ED) for syncope with bright red blood per rectum (BRBPR) during a bowel movement (BM). He had dismissed 2 months of intermittent melena. He presented with shortness of breath, palpitations and asthenia. He was an active smoker with unremarkable family history. In the ED, he had 2 more episodes of BRBPR.
Initial labs showed hemoglobin (Hgb) of 5.5 g/dL with high reticulocyte count. He received IV pantoprazole and 2 units of packed red red blood cells (PRBCs). GI recommended a non-emergent colonoscopy with optimal bowel prep. CT angiography and tagged red blood cell scan did not reveal active GI bleeding. After 4 units of PRBCs, Hgb improved to 7.4 g/dL.
On hospital day 3, another bloody BM decreased Hgb to 6.7 g/dL and he got another unit of blood. EGD revealed shallow erosion in duodenal bulb (chronic gastritis). Colonoscopy showed a Dieulafoy lesion with spurting in the ascending colon (Fig.1). 3 endoclips were applied (Fig.2), resolving the bleeding.
A day later, he syncopized again with a bloody BM. Surgery declined intervention. He was sent to ICU for further transfusion before transfer to a tertiary center for IR management due to refractory GI bleed.
Discussion: DLs, though rare, can cause life-threatening GI bleeding. They affect the stomach in 95% of cases. Our case features a rare ascending colon location and refractory hemorrhage despite standard therapy. We emphasize the need for patient education, as delayed presentations (e.g., 2 months of melena) cause an unfavorable course. This is especially applicable to men from lower socioeconomic backgrounds whose health seeking behavior trends more towards avoidance than pursuit.
Endoscopy, the gold standard for both diagnosis and treatment of DL, demonstrates high sensitivity with optimal bowel prep and expert technique. Our case shows limitations of non-endoscopic methods like CTA and tagged RBC scans, which yielded false negatives. Despite employing endoclips - considered a safe and effective treatment - our patient re-bled, highlighting the complex and unpredictable nature of DLs. Refractory cases may require escalation to interventional radiology or surgery.
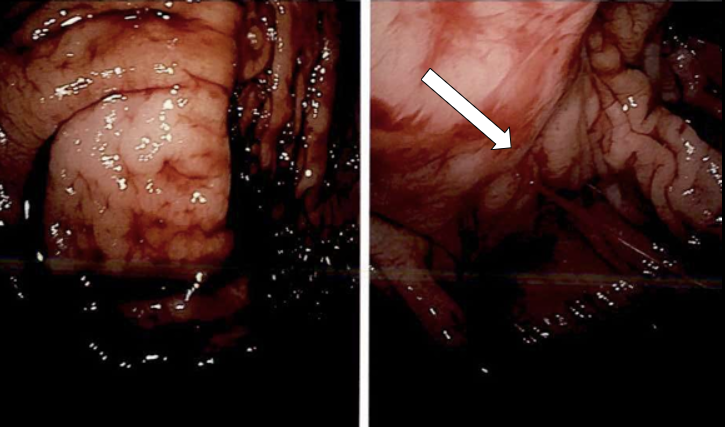
Figure: Fig. 1
Credit: Dr. Twersky
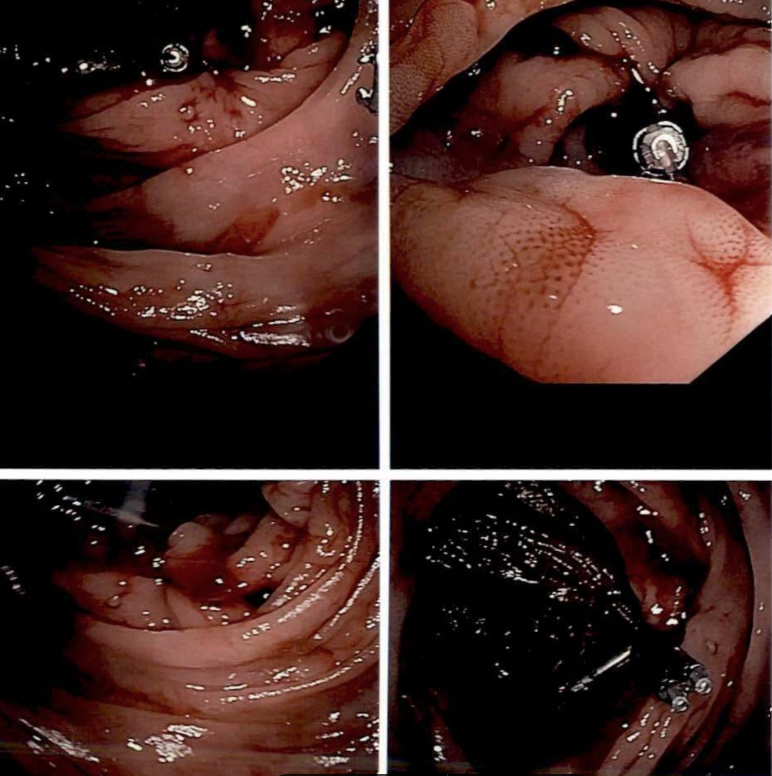
Figure: Fig. 2
Disclosures:
Farirai Melania Marwizi indicated no relevant financial relationships.
Olanrewaju Adeniran indicated no relevant financial relationships.
Abidemi Akinrinmade indicated no relevant financial relationships.
Ifeoma Kwentoh indicated no relevant financial relationships.
Shekwonya Sakoma indicated no relevant financial relationships.
Adela Damm indicated no relevant financial relationships.
Farirai Melania Marwizi, MD1, Olanrewaju Adeniran, MD2, Abidemi Akinrinmade, MBBS3, Ifeoma P. Kwentoh, MD4, Shekwonya Damaris. Sakoma, MD5, Adela Damm, MD6. P0993 - Beyond the Usual Suspects: When Intermittent Melena Heralds a Life-Threatening Dieulafoy Lesion, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Episcopal Health Services, Queens, NY; 2West Virginia University Morgantown, Morgantown, WV; 3University of Pittsburgh Medical Center, Monroeville, PA; 4New York Institute of Technology College of Osteopathic Medicine, Kent, CT; 5Jersey City Medical Center, Jersey City, NJ; 6University of Medicine and Pharmacy 'Victor Babes', Timisoara, Hermitage, TN
Introduction: Dieulafoy lesions (DLs) are a rare cause of gastrointestinal (GI) bleeding due to erosion of an aberrant submucosal artery extending to the mucosa. We present a case of an adult with no apparent risk factors who developed life threatening, refractory GI bleeding due to a Dieulafoy lesion.
Case Description/
Methods: 38-year old male presented to the emergency department (ED) for syncope with bright red blood per rectum (BRBPR) during a bowel movement (BM). He had dismissed 2 months of intermittent melena. He presented with shortness of breath, palpitations and asthenia. He was an active smoker with unremarkable family history. In the ED, he had 2 more episodes of BRBPR.
Initial labs showed hemoglobin (Hgb) of 5.5 g/dL with high reticulocyte count. He received IV pantoprazole and 2 units of packed red red blood cells (PRBCs). GI recommended a non-emergent colonoscopy with optimal bowel prep. CT angiography and tagged red blood cell scan did not reveal active GI bleeding. After 4 units of PRBCs, Hgb improved to 7.4 g/dL.
On hospital day 3, another bloody BM decreased Hgb to 6.7 g/dL and he got another unit of blood. EGD revealed shallow erosion in duodenal bulb (chronic gastritis). Colonoscopy showed a Dieulafoy lesion with spurting in the ascending colon (Fig.1). 3 endoclips were applied (Fig.2), resolving the bleeding.
A day later, he syncopized again with a bloody BM. Surgery declined intervention. He was sent to ICU for further transfusion before transfer to a tertiary center for IR management due to refractory GI bleed.
Discussion: DLs, though rare, can cause life-threatening GI bleeding. They affect the stomach in 95% of cases. Our case features a rare ascending colon location and refractory hemorrhage despite standard therapy. We emphasize the need for patient education, as delayed presentations (e.g., 2 months of melena) cause an unfavorable course. This is especially applicable to men from lower socioeconomic backgrounds whose health seeking behavior trends more towards avoidance than pursuit.
Endoscopy, the gold standard for both diagnosis and treatment of DL, demonstrates high sensitivity with optimal bowel prep and expert technique. Our case shows limitations of non-endoscopic methods like CTA and tagged RBC scans, which yielded false negatives. Despite employing endoclips - considered a safe and effective treatment - our patient re-bled, highlighting the complex and unpredictable nature of DLs. Refractory cases may require escalation to interventional radiology or surgery.
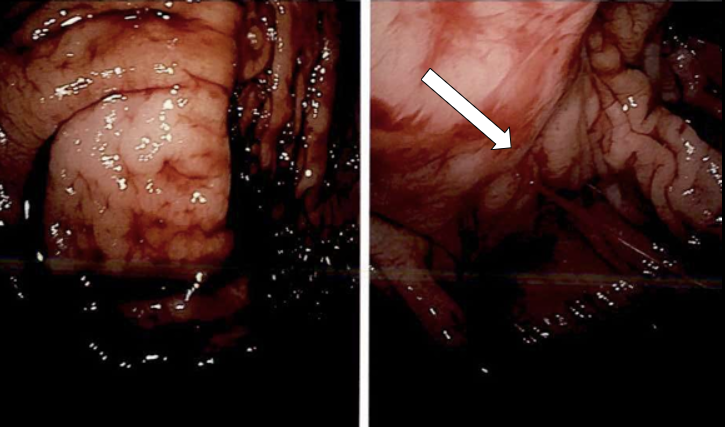
Figure: Fig. 1
Credit: Dr. Twersky
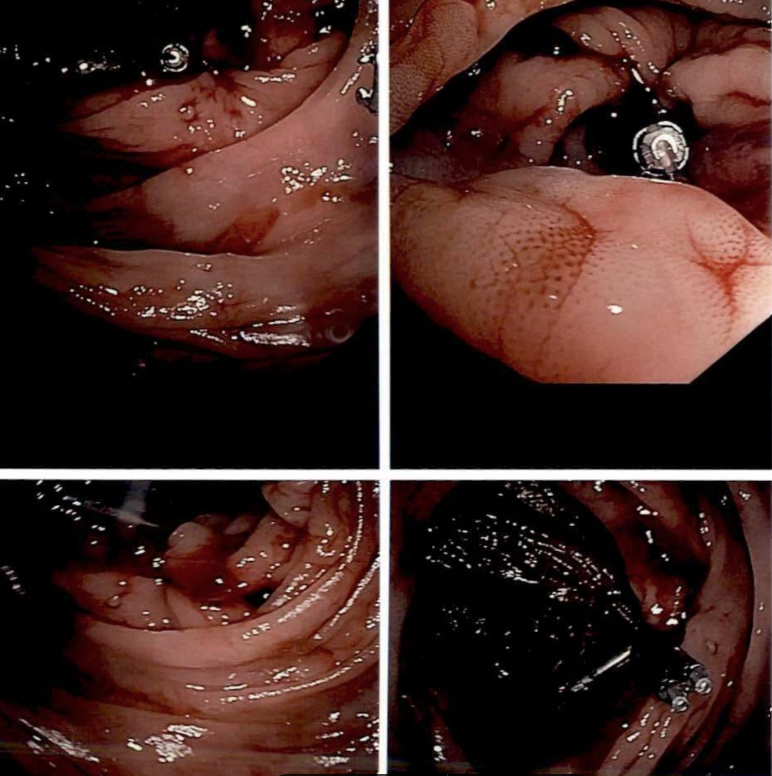
Figure: Fig. 2
Disclosures:
Farirai Melania Marwizi indicated no relevant financial relationships.
Olanrewaju Adeniran indicated no relevant financial relationships.
Abidemi Akinrinmade indicated no relevant financial relationships.
Ifeoma Kwentoh indicated no relevant financial relationships.
Shekwonya Sakoma indicated no relevant financial relationships.
Adela Damm indicated no relevant financial relationships.
Farirai Melania Marwizi, MD1, Olanrewaju Adeniran, MD2, Abidemi Akinrinmade, MBBS3, Ifeoma P. Kwentoh, MD4, Shekwonya Damaris. Sakoma, MD5, Adela Damm, MD6. P0993 - Beyond the Usual Suspects: When Intermittent Melena Heralds a Life-Threatening Dieulafoy Lesion, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
