Sunday Poster Session
Category: GI Bleeding
P0990 - Dieulafoy Lesion in a Post–Deceased Donor Liver Transplant Patient: A Rare Cause of Upper GI Bleeding
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Raza Muhammad, DO (he/him/his)
University of Chicago/Northshore
Evanston, IL
Presenting Author(s)
Raza Muhammad, DO1, Ushan A. Ranasinghe, MBBS2, Joseph Ahn, MD3, Edward C. Villa, MD4
1University of Chicago/Northshore, Evanston, IL; 2University of Chicago, NorthShore Health Systems, Chicago, IL; 3Endeavor Health, Niles, IL; 4University of Chicago, Northshore University Healthsystem, Chicago, IL
Introduction: Dieulafoy lesions, characterized by a large-caliber submucosal artery eroding the mucosa in the absence of ulceration, are an uncommon but serious cause of upper gastrointestinal bleeding. We report a rare case of a bleeding Dieulafoy lesion in a post–liver transplant patient, representing one of only two such cases documented in the literature.
Case Description/
Methods: A 74-year-old male with a history of chronic HBV infection and hepatocellular carcinoma s/p deceased donor liver transplant (2021) with post-transplant course complicated by ischemic cholangiopathy, recurrent portal hypertension presented with a hemoglobin of 5.8 (baseline 8-9) on routine labs without overt signs of bleeding. Other remarkable labs included platelets 230, BUN 30, Cr 1.8 (baseline), Tbili 2.7, DBili 1.8, and albumin 2.6. Aminotransferase levels, hemolysis, and coagulation labs were unremarkable. He endorsed fatigue and dark brown stools one week prior to arrival. On exam, he was tachycardic, with otherwise normal vital signs and negative DRE. He had bilateral lower extremity edema, abdominal distention with fluid wave, and mild pallor on exam. The patient was transfused 2 units of pRBCs and started on an octreotide infusion and pantoprazole. Push enteroscopy was remarkable for LA Grade D reflux and erosive esophagitis, and a bleeding Dieulafoy lesion with active hemorrhage at the gastric cardia. Hemostasis was successfully achieved with hemostatic clips and thermocautery.
Discussion: Dieulafoy lesions are often missed in the absence of active bleeding, given their subtle mucosal appearance, which can present as a raised nipple, visible vessel, or just normal appearing mucosa with no ulceration. Though pathogenesis is incompletely understood, portal hypertension and mucosal ischemia have been implicated. In our post–liver transplant patient with cellular rejection and portal HTN, altered hemodynamics may have contributed to angiogenesis as well as remodeling of the existing vasculature. Further studies are required to investigate the relationship of these lesions in this patient population.
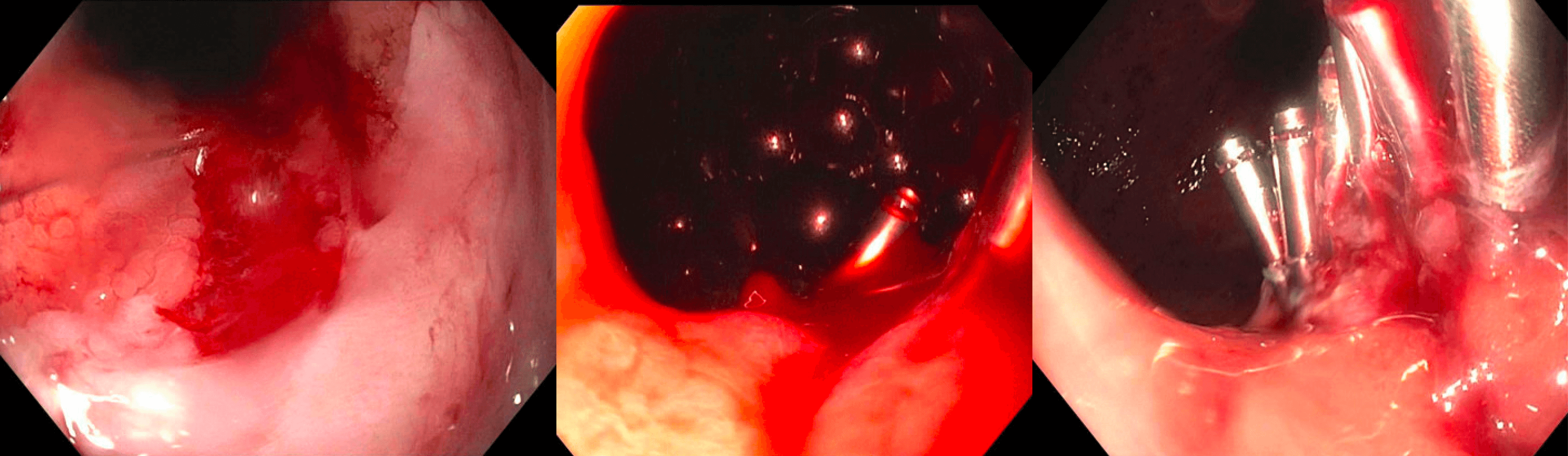
Figure: Bleeding Dieulafoy lesion with active hemorrhage at the gastric cardia
Disclosures:
Raza Muhammad indicated no relevant financial relationships.
Ushan Ranasinghe indicated no relevant financial relationships.
Joseph Ahn: Madrigal – Advisory Committee/Board Member.
Edward Villa: Olympus Corporation – Consultant.
Raza Muhammad, DO1, Ushan A. Ranasinghe, MBBS2, Joseph Ahn, MD3, Edward C. Villa, MD4. P0990 - Dieulafoy Lesion in a Post–Deceased Donor Liver Transplant Patient: A Rare Cause of Upper GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Chicago/Northshore, Evanston, IL; 2University of Chicago, NorthShore Health Systems, Chicago, IL; 3Endeavor Health, Niles, IL; 4University of Chicago, Northshore University Healthsystem, Chicago, IL
Introduction: Dieulafoy lesions, characterized by a large-caliber submucosal artery eroding the mucosa in the absence of ulceration, are an uncommon but serious cause of upper gastrointestinal bleeding. We report a rare case of a bleeding Dieulafoy lesion in a post–liver transplant patient, representing one of only two such cases documented in the literature.
Case Description/
Methods: A 74-year-old male with a history of chronic HBV infection and hepatocellular carcinoma s/p deceased donor liver transplant (2021) with post-transplant course complicated by ischemic cholangiopathy, recurrent portal hypertension presented with a hemoglobin of 5.8 (baseline 8-9) on routine labs without overt signs of bleeding. Other remarkable labs included platelets 230, BUN 30, Cr 1.8 (baseline), Tbili 2.7, DBili 1.8, and albumin 2.6. Aminotransferase levels, hemolysis, and coagulation labs were unremarkable. He endorsed fatigue and dark brown stools one week prior to arrival. On exam, he was tachycardic, with otherwise normal vital signs and negative DRE. He had bilateral lower extremity edema, abdominal distention with fluid wave, and mild pallor on exam. The patient was transfused 2 units of pRBCs and started on an octreotide infusion and pantoprazole. Push enteroscopy was remarkable for LA Grade D reflux and erosive esophagitis, and a bleeding Dieulafoy lesion with active hemorrhage at the gastric cardia. Hemostasis was successfully achieved with hemostatic clips and thermocautery.
Discussion: Dieulafoy lesions are often missed in the absence of active bleeding, given their subtle mucosal appearance, which can present as a raised nipple, visible vessel, or just normal appearing mucosa with no ulceration. Though pathogenesis is incompletely understood, portal hypertension and mucosal ischemia have been implicated. In our post–liver transplant patient with cellular rejection and portal HTN, altered hemodynamics may have contributed to angiogenesis as well as remodeling of the existing vasculature. Further studies are required to investigate the relationship of these lesions in this patient population.
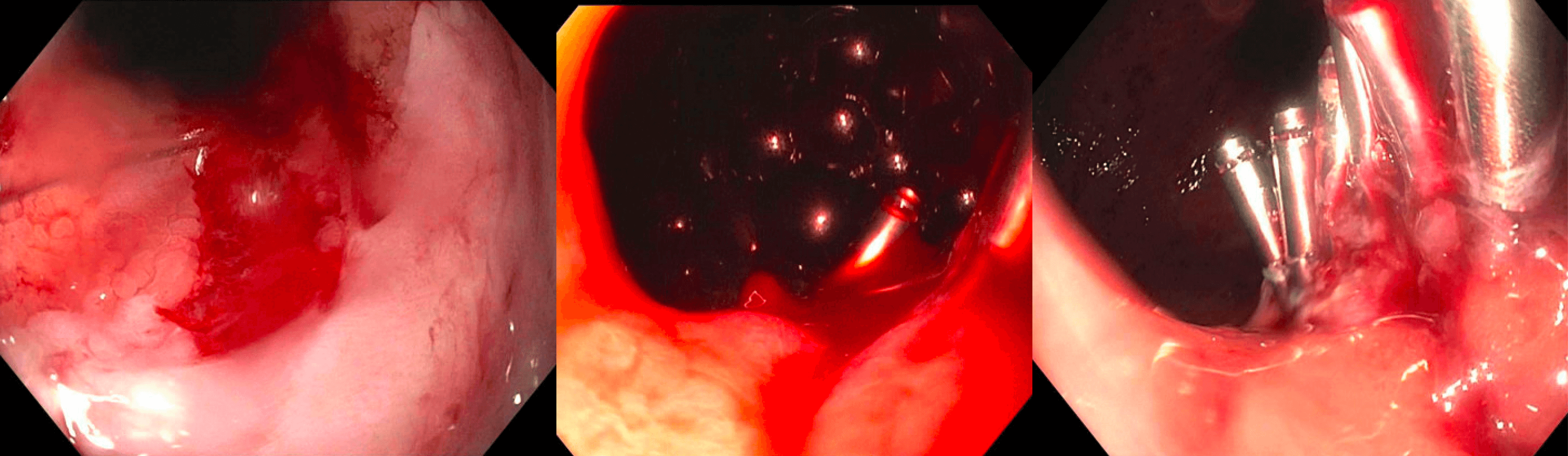
Figure: Bleeding Dieulafoy lesion with active hemorrhage at the gastric cardia
Disclosures:
Raza Muhammad indicated no relevant financial relationships.
Ushan Ranasinghe indicated no relevant financial relationships.
Joseph Ahn: Madrigal – Advisory Committee/Board Member.
Edward Villa: Olympus Corporation – Consultant.
Raza Muhammad, DO1, Ushan A. Ranasinghe, MBBS2, Joseph Ahn, MD3, Edward C. Villa, MD4. P0990 - Dieulafoy Lesion in a Post–Deceased Donor Liver Transplant Patient: A Rare Cause of Upper GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
