Sunday Poster Session
Category: GI Bleeding
P0960 - Variant Mechanism in the Development of an Aorto-esophageal Fistula
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Kelly Fan, MD (she/her/hers)
SSM Health Saint Louis University Hospital
St. Louis, MO
Presenting Author(s)
Kelly Fan, MD1, Ameya Deshmukh, DO1, Isra N. Taha, MD1, Adam D. Farmer, MD, PhD2
1SSM Health Saint Louis University Hospital, St. Louis, MO; 2SSM Health Saint Louis University Hospital, Saint Louis, MO
Introduction: Aorto-esophageal fistulas (AEFs) are rare but life-threatening causes of upper GI bleeding, typically associated with prior aortic surgery. We report a novel case of AEF resulting from pressure necrosis caused by an expanding clot in the false lumen of a type B aortic dissection, leading to fistula formation and fatal hemorrhage.
Case Description/
Methods: A 62-year-old woman with antiphospholipid syndrome, lupus, and prior cerebrovascular accidents presented with severe headache and hypertension. Initial coffee-ground aspirate via nasogastric tube resolved spontaneously, and a proton pump inhibitor was initiated. Subsequently, her hemoglobin dropped from 8.0 to 4.2 g/dL. Abdominal computed tomography angiography (CTA) revealed a 5.5-cm thoracoabdominal type B aortic dissection and a large left chest wall hematoma.
Days later, the patient developed 300 mL of hematemesis. EGD identified a pulsatile clot in the distal esophagus, suggestive of AEF (Figure 1). Due to high AEF risk, EGD remained diagnostic. Repeat CTA demonstrated increased thrombosis in the false lumen of the dissection, abutting the distal esophagus, with a contrast blush confirming AEF (Figure 2). Multidisciplinary evaluation deemed the AEF inoperable due to insufficient healthy aorta for stent placement. The condition was considered terminal, and the patient transitioned to end of life care, passing shortly thereafter.
Discussion: AEFs are rare causes of catastrophic GI bleeding, typically linked to thoracic endovascular aortic repair or aortic aneurysm repair, where stents induce pressure necrosis. Patients may exhibit Chiari’s triad: chest pain, sentinel hemorrhage, and a symptom-free interval before fatal exsanguination. This case is unique due to AEF formation from clot expansion in the false lumen of a type B aortic dissection, mimicking postoperative mechanisms without prior surgical intervention. The patient’s connective tissue and hypercoagulable disorders likely exacerbated vascular fragility and thrombosis. This case highlights the need for heightened suspicion of AEF in patients with aortic dissection and GI bleeding, even without surgical history. Imaging and multidisciplinary input are critical for diagnosis, though treatment options may be limited by anatomical constraints.
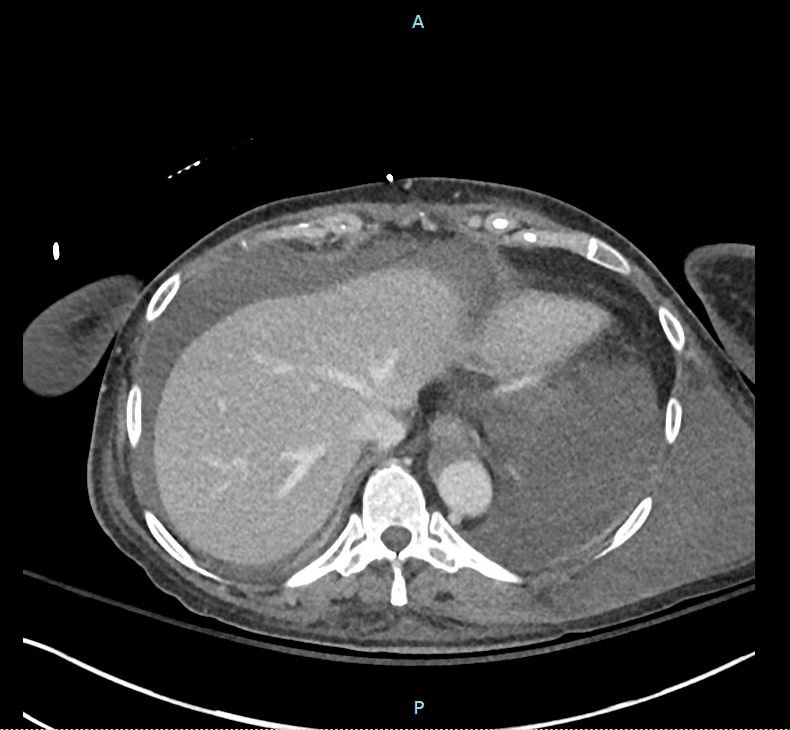
Figure: Figure 1. EGD showing a pulsatile clot in the distal esophagus (~30 cm from incisors), suggestive of AEF.
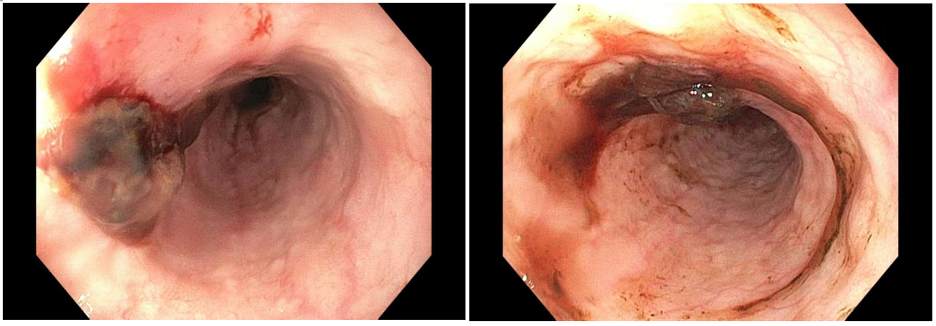
Figure: Figure 2. CTA demonstrating increased clot burden in the false lumen of a type B aortic dissection, abutting the distal esophagus with a contrast blush confirming AEF.
Disclosures:
Kelly Fan indicated no relevant financial relationships.
Ameya Deshmukh indicated no relevant financial relationships.
Isra Taha indicated no relevant financial relationships.
Adam D. Farmer indicated no relevant financial relationships.
Kelly Fan, MD1, Ameya Deshmukh, DO1, Isra N. Taha, MD1, Adam D. Farmer, MD, PhD2. P0960 - Variant Mechanism in the Development of an Aorto-esophageal Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SSM Health Saint Louis University Hospital, St. Louis, MO; 2SSM Health Saint Louis University Hospital, Saint Louis, MO
Introduction: Aorto-esophageal fistulas (AEFs) are rare but life-threatening causes of upper GI bleeding, typically associated with prior aortic surgery. We report a novel case of AEF resulting from pressure necrosis caused by an expanding clot in the false lumen of a type B aortic dissection, leading to fistula formation and fatal hemorrhage.
Case Description/
Methods: A 62-year-old woman with antiphospholipid syndrome, lupus, and prior cerebrovascular accidents presented with severe headache and hypertension. Initial coffee-ground aspirate via nasogastric tube resolved spontaneously, and a proton pump inhibitor was initiated. Subsequently, her hemoglobin dropped from 8.0 to 4.2 g/dL. Abdominal computed tomography angiography (CTA) revealed a 5.5-cm thoracoabdominal type B aortic dissection and a large left chest wall hematoma.
Days later, the patient developed 300 mL of hematemesis. EGD identified a pulsatile clot in the distal esophagus, suggestive of AEF (Figure 1). Due to high AEF risk, EGD remained diagnostic. Repeat CTA demonstrated increased thrombosis in the false lumen of the dissection, abutting the distal esophagus, with a contrast blush confirming AEF (Figure 2). Multidisciplinary evaluation deemed the AEF inoperable due to insufficient healthy aorta for stent placement. The condition was considered terminal, and the patient transitioned to end of life care, passing shortly thereafter.
Discussion: AEFs are rare causes of catastrophic GI bleeding, typically linked to thoracic endovascular aortic repair or aortic aneurysm repair, where stents induce pressure necrosis. Patients may exhibit Chiari’s triad: chest pain, sentinel hemorrhage, and a symptom-free interval before fatal exsanguination. This case is unique due to AEF formation from clot expansion in the false lumen of a type B aortic dissection, mimicking postoperative mechanisms without prior surgical intervention. The patient’s connective tissue and hypercoagulable disorders likely exacerbated vascular fragility and thrombosis. This case highlights the need for heightened suspicion of AEF in patients with aortic dissection and GI bleeding, even without surgical history. Imaging and multidisciplinary input are critical for diagnosis, though treatment options may be limited by anatomical constraints.
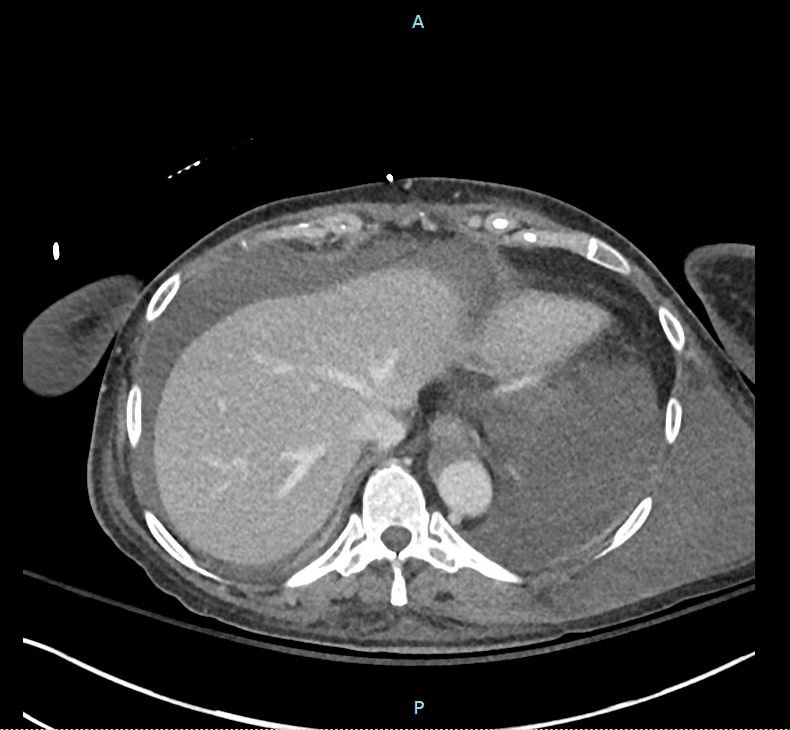
Figure: Figure 1. EGD showing a pulsatile clot in the distal esophagus (~30 cm from incisors), suggestive of AEF.
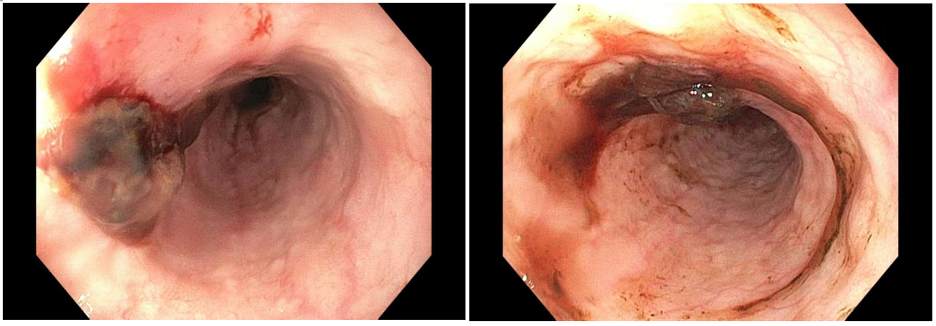
Figure: Figure 2. CTA demonstrating increased clot burden in the false lumen of a type B aortic dissection, abutting the distal esophagus with a contrast blush confirming AEF.
Disclosures:
Kelly Fan indicated no relevant financial relationships.
Ameya Deshmukh indicated no relevant financial relationships.
Isra Taha indicated no relevant financial relationships.
Adam D. Farmer indicated no relevant financial relationships.
Kelly Fan, MD1, Ameya Deshmukh, DO1, Isra N. Taha, MD1, Adam D. Farmer, MD, PhD2. P0960 - Variant Mechanism in the Development of an Aorto-esophageal Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
