Sunday Poster Session
Category: GI Bleeding
P0953 - Bleeding Beyond Reach: A Jejunal Dieulafoy’s Lesion Requiring Advanced Endoscopic Rescue
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- MW
Mahader N. Wossene, MD (he/him/his)
MacNeal Hospital Loyola Medicine
Berwyn, IL
Presenting Author(s)
Mahader N. Wossene, MD1, Genet Hagos. Weldemichael, MD1, Vaishnavi K. Modi, MD2, Anum Nawaz, MBBS, MD2, Soulaf Abou Khachfe, MD2, Amit Srivastava, MD3
1MacNeal Hospital Loyola Medicine, Berwyn, IL; 2MacNeal Hospital Loyola Medicine, Oak Park, IL; 3MacNeal Hospital Loyola Medicine, Burr ridge, IL
Introduction: Dieulafoy's lesion (DL) is a rare but potentially life-threatening cause of gastrointestinal bleeding (GIB), accounting for less than 2% of cases. While commonly localized in the proximal stomach, jejunal DLs are quire rare, and a diagnostic challenge given their location and intermittent bleeding. We report a case of jejunal DL successfully managed with advanced endoscopic therapy.
Case Description/
Methods: A 39-year- old male with no significant medical history presented with sudden epigastric pain, melena and dark emesis. He denied any medication use except NSAIDS taken four days prior. CT abdomen/pelvis and CT angiography showed no active bleeding. Admission hemoglobin was 10.8 g/dL but declined to 7 g/dL with tachycardia and hypotension. He was admitted to the ICU and received 9 units of packed PRBCs under massive transfusion protocol.
Esophagogastroduodenoscopy showed fresh blood in the duodenum but no source. Push enteroscopy using a pediatric colonoscope revealed a 3 mm spurting lesion with a visible vessel in the jejunum, consistent with DL. Hemostasis was achieved using six hemoclips, epinephrine injections, bipolar cautery and hemospray. No further bleeding was observed on repeat endoscopy and imaging, interventional radiology deferred embolization due to ischemic risk.
The patient's hemoglobin stabilized without further transfusion. He resumed oral intake and was discharged on high-dose pantoprazole with taper and sucralfate.
Discussion: DL accounts for 1% to 2% of acute GIB mostly in the stomach (72%), duodenum (15%), esophagus (8%), but rarely in jejunum. Diagnosis requires high clinical suspicion and specialized endoscopy. A 2022 systematic review reported 98 small bowel DL since 1978; 48% jejunal with a mean age of 45.5 and male predominance (62.5%), aligning with our case.
Jejunal DLs often elude standard imaging. Push enteroscopy using a pediatric colonoscope, which allows reaching 45–60 cm past the ligament of Treitz, was key for localization in this case. While mechanical therapies are effective, combination endoscopic therapy yields better results. Multimodal treatment (Clips, epinephrine, cautery and hemospray) achieved hemostasis in this case. Rebleeding after embolization is higher for small bowel lesions due to limited collaterals and extensive vascular territory. The decision to forego interventional radiology highlights the efficacy and safety of endoscopic therapy when expertly applied for obscure GIB. this case contributes to the limited literature on jejunal DLs.
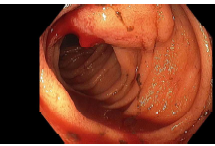
Figure: a 3mm spurting ulcer with a visible vessel was found in the jejunum
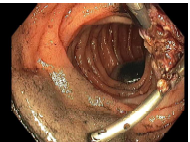
Figure: bipolar cautery and hemostatic clip placement on the spurting jejunal ulcer
Disclosures:
Mahader Wossene indicated no relevant financial relationships.
Genet Weldemichael indicated no relevant financial relationships.
Vaishnavi Modi indicated no relevant financial relationships.
Anum Nawaz indicated no relevant financial relationships.
Soulaf Abou Khachfe indicated no relevant financial relationships.
Amit Srivastava indicated no relevant financial relationships.
Mahader N. Wossene, MD1, Genet Hagos. Weldemichael, MD1, Vaishnavi K. Modi, MD2, Anum Nawaz, MBBS, MD2, Soulaf Abou Khachfe, MD2, Amit Srivastava, MD3. P0953 - Bleeding Beyond Reach: A Jejunal Dieulafoy’s Lesion Requiring Advanced Endoscopic Rescue, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1MacNeal Hospital Loyola Medicine, Berwyn, IL; 2MacNeal Hospital Loyola Medicine, Oak Park, IL; 3MacNeal Hospital Loyola Medicine, Burr ridge, IL
Introduction: Dieulafoy's lesion (DL) is a rare but potentially life-threatening cause of gastrointestinal bleeding (GIB), accounting for less than 2% of cases. While commonly localized in the proximal stomach, jejunal DLs are quire rare, and a diagnostic challenge given their location and intermittent bleeding. We report a case of jejunal DL successfully managed with advanced endoscopic therapy.
Case Description/
Methods: A 39-year- old male with no significant medical history presented with sudden epigastric pain, melena and dark emesis. He denied any medication use except NSAIDS taken four days prior. CT abdomen/pelvis and CT angiography showed no active bleeding. Admission hemoglobin was 10.8 g/dL but declined to 7 g/dL with tachycardia and hypotension. He was admitted to the ICU and received 9 units of packed PRBCs under massive transfusion protocol.
Esophagogastroduodenoscopy showed fresh blood in the duodenum but no source. Push enteroscopy using a pediatric colonoscope revealed a 3 mm spurting lesion with a visible vessel in the jejunum, consistent with DL. Hemostasis was achieved using six hemoclips, epinephrine injections, bipolar cautery and hemospray. No further bleeding was observed on repeat endoscopy and imaging, interventional radiology deferred embolization due to ischemic risk.
The patient's hemoglobin stabilized without further transfusion. He resumed oral intake and was discharged on high-dose pantoprazole with taper and sucralfate.
Discussion: DL accounts for 1% to 2% of acute GIB mostly in the stomach (72%), duodenum (15%), esophagus (8%), but rarely in jejunum. Diagnosis requires high clinical suspicion and specialized endoscopy. A 2022 systematic review reported 98 small bowel DL since 1978; 48% jejunal with a mean age of 45.5 and male predominance (62.5%), aligning with our case.
Jejunal DLs often elude standard imaging. Push enteroscopy using a pediatric colonoscope, which allows reaching 45–60 cm past the ligament of Treitz, was key for localization in this case. While mechanical therapies are effective, combination endoscopic therapy yields better results. Multimodal treatment (Clips, epinephrine, cautery and hemospray) achieved hemostasis in this case. Rebleeding after embolization is higher for small bowel lesions due to limited collaterals and extensive vascular territory. The decision to forego interventional radiology highlights the efficacy and safety of endoscopic therapy when expertly applied for obscure GIB. this case contributes to the limited literature on jejunal DLs.
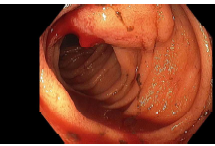
Figure: a 3mm spurting ulcer with a visible vessel was found in the jejunum
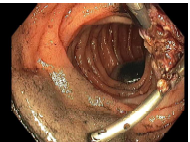
Figure: bipolar cautery and hemostatic clip placement on the spurting jejunal ulcer
Disclosures:
Mahader Wossene indicated no relevant financial relationships.
Genet Weldemichael indicated no relevant financial relationships.
Vaishnavi Modi indicated no relevant financial relationships.
Anum Nawaz indicated no relevant financial relationships.
Soulaf Abou Khachfe indicated no relevant financial relationships.
Amit Srivastava indicated no relevant financial relationships.
Mahader N. Wossene, MD1, Genet Hagos. Weldemichael, MD1, Vaishnavi K. Modi, MD2, Anum Nawaz, MBBS, MD2, Soulaf Abou Khachfe, MD2, Amit Srivastava, MD3. P0953 - Bleeding Beyond Reach: A Jejunal Dieulafoy’s Lesion Requiring Advanced Endoscopic Rescue, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
