Sunday Poster Session
Category: GI Bleeding
P0941 - Bleeding Under Pressure: Patterns of GI Hemorrhage in ECMO Patients
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- CA
Chima Amadi, MD, MBA (he/him/his)
Morehouse School of Medicine
Atlanta, GA
Presenting Author(s)
Chima Amadi, MD, MBA1, Chisom Nwaneki, MD2, Joseph A. Atarere, MBChB, MPH3, Abisola Ajayi, MD1, Ayomide F. Sowemimo, MSc, MD1, Olanrewaju Adeniran, MD4, Violet Iyahen, BS1, Eunice Omeludike, MD5, Julia Liu, MD1
1Morehouse School of Medicine, Atlanta, GA; 2Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 3MedStar Georgetown University Hospital, Baltimore, MD; 4West Virginia University Morgantown, Morgantown, WV; 5Piedmont Athens Regional Medical Centre, Athens, GA
Introduction: Extracorporeal membrane oxygenation (ECMO) is a critical, life-saving intervention for patients with severe cardiopulmonary failure. However, ECMO is associated with a range of complications, including gastrointestinal (GI) bleeding, which can contribute to increased morbidity in an already high-risk population. Despite its clinical significance, limited data exist on the timing and pattern of GI bleeding in relation to ECMO initiation. This study aims to evaluate frequency and type of GI bleeding among ECMO patients and its association to timing, length of stay and in-hospital mortality.
Methods: We used retrospective data from the 2016 to 2020 iterations of the Nationwide Inpatient Sample, including patients who underwent ECMO during the course of hospitalization. ECMO initiation was categorized as early (< 24 hours), delayed (24-48 hours) and late ( >48 hours). We collected data on study population characteristics including the frequency of upper and lower GI bleed and described them by timing of ECMO initiation. We also evaluated in-hospital mortality and LOS using adjusted logistic and Poisson regression models respectively.
Results: Of the 1,293 participants, ECMO was initiated within 24 hours of admission in 842 (65.2%). Most were male (63.3%), admitted to large hospitals (79.1%), and critically ill (61.8%). Early initiators were more likely to be in shock (65.0%) than delayed (58.9%) or late (54.7%) groups, but had fewer comorbidities (34.6% vs. 44.4% and 44.0%). GI bleeding was rare but more often upper (1.24%) than lower (0.23%). Late ECMO was linked to longer LOS [IRR 1.53; 95% CI (1.32–1.79)]. Mortality did not differ by timing.
Discussion: In this nationally representative cohort of ECMO patients, gastrointestinal bleeding was relatively rare but predominantly upper in origin. Timing of ECMO initiation—early, delayed, or late—was not significantly associated with the occurrence of GI bleeding, suggesting that bleeding risk may be independent of initiation strategy. However, late ECMO initiation was linked to prolonged hospital stays, reflecting increased resource utilization. These findings highlight the importance of ongoing GI monitoring in ECMO patients and suggest that timing alone may not predict bleeding complications in this high-risk population.
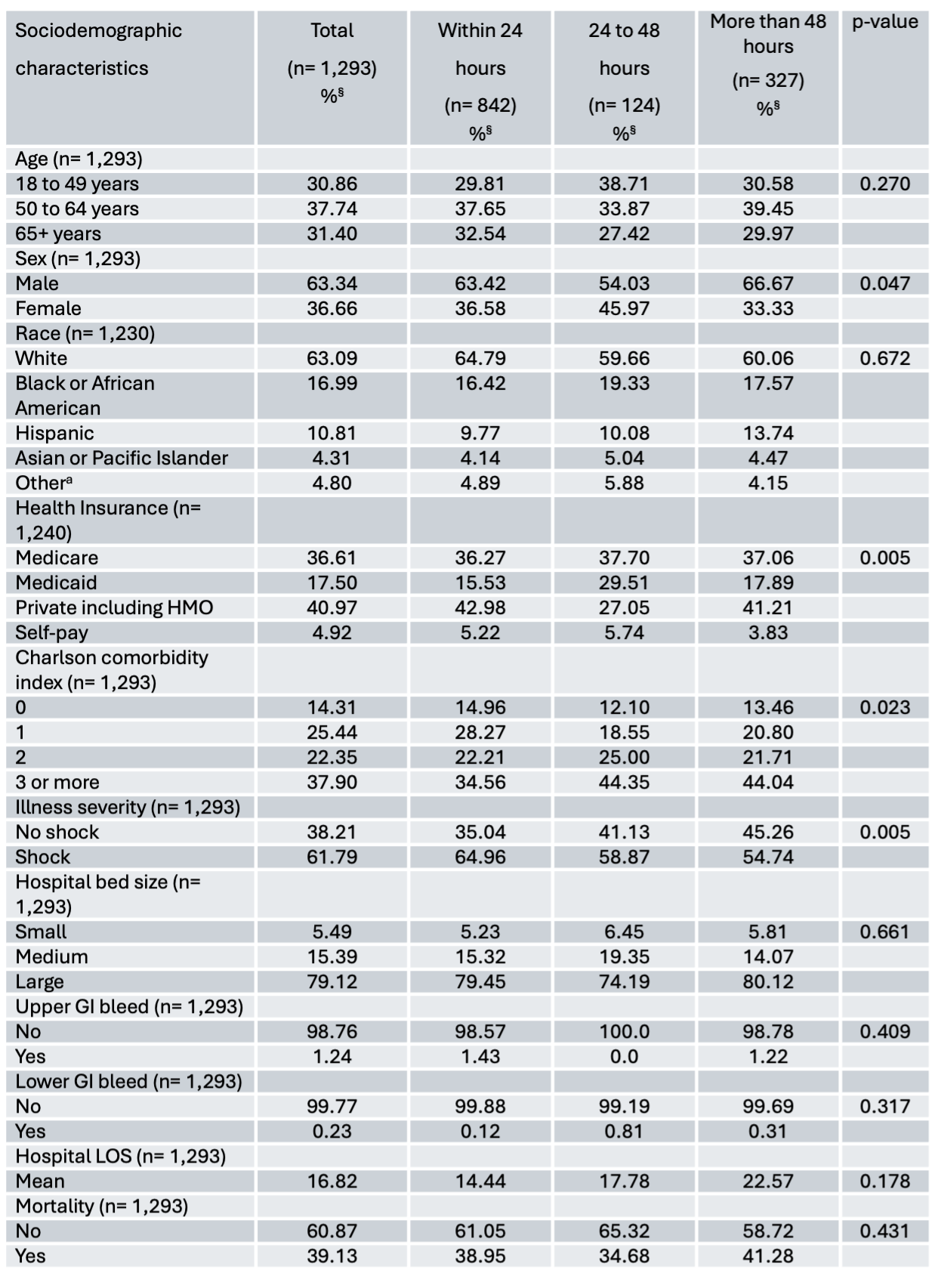
Figure: Table 1: Baseline study population characteristics by timing of ECMO, NIS 2016 to 2020
Disclosures:
Chima Amadi indicated no relevant financial relationships.
Chisom Nwaneki indicated no relevant financial relationships.
Joseph Atarere indicated no relevant financial relationships.
Abisola Ajayi indicated no relevant financial relationships.
Ayomide Sowemimo indicated no relevant financial relationships.
Olanrewaju Adeniran indicated no relevant financial relationships.
Violet Iyahen indicated no relevant financial relationships.
Eunice Omeludike indicated no relevant financial relationships.
Julia Liu indicated no relevant financial relationships.
Chima Amadi, MD, MBA1, Chisom Nwaneki, MD2, Joseph A. Atarere, MBChB, MPH3, Abisola Ajayi, MD1, Ayomide F. Sowemimo, MSc, MD1, Olanrewaju Adeniran, MD4, Violet Iyahen, BS1, Eunice Omeludike, MD5, Julia Liu, MD1. P0941 - Bleeding Under Pressure: Patterns of GI Hemorrhage in ECMO Patients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Morehouse School of Medicine, Atlanta, GA; 2Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 3MedStar Georgetown University Hospital, Baltimore, MD; 4West Virginia University Morgantown, Morgantown, WV; 5Piedmont Athens Regional Medical Centre, Athens, GA
Introduction: Extracorporeal membrane oxygenation (ECMO) is a critical, life-saving intervention for patients with severe cardiopulmonary failure. However, ECMO is associated with a range of complications, including gastrointestinal (GI) bleeding, which can contribute to increased morbidity in an already high-risk population. Despite its clinical significance, limited data exist on the timing and pattern of GI bleeding in relation to ECMO initiation. This study aims to evaluate frequency and type of GI bleeding among ECMO patients and its association to timing, length of stay and in-hospital mortality.
Methods: We used retrospective data from the 2016 to 2020 iterations of the Nationwide Inpatient Sample, including patients who underwent ECMO during the course of hospitalization. ECMO initiation was categorized as early (< 24 hours), delayed (24-48 hours) and late ( >48 hours). We collected data on study population characteristics including the frequency of upper and lower GI bleed and described them by timing of ECMO initiation. We also evaluated in-hospital mortality and LOS using adjusted logistic and Poisson regression models respectively.
Results: Of the 1,293 participants, ECMO was initiated within 24 hours of admission in 842 (65.2%). Most were male (63.3%), admitted to large hospitals (79.1%), and critically ill (61.8%). Early initiators were more likely to be in shock (65.0%) than delayed (58.9%) or late (54.7%) groups, but had fewer comorbidities (34.6% vs. 44.4% and 44.0%). GI bleeding was rare but more often upper (1.24%) than lower (0.23%). Late ECMO was linked to longer LOS [IRR 1.53; 95% CI (1.32–1.79)]. Mortality did not differ by timing.
Discussion: In this nationally representative cohort of ECMO patients, gastrointestinal bleeding was relatively rare but predominantly upper in origin. Timing of ECMO initiation—early, delayed, or late—was not significantly associated with the occurrence of GI bleeding, suggesting that bleeding risk may be independent of initiation strategy. However, late ECMO initiation was linked to prolonged hospital stays, reflecting increased resource utilization. These findings highlight the importance of ongoing GI monitoring in ECMO patients and suggest that timing alone may not predict bleeding complications in this high-risk population.
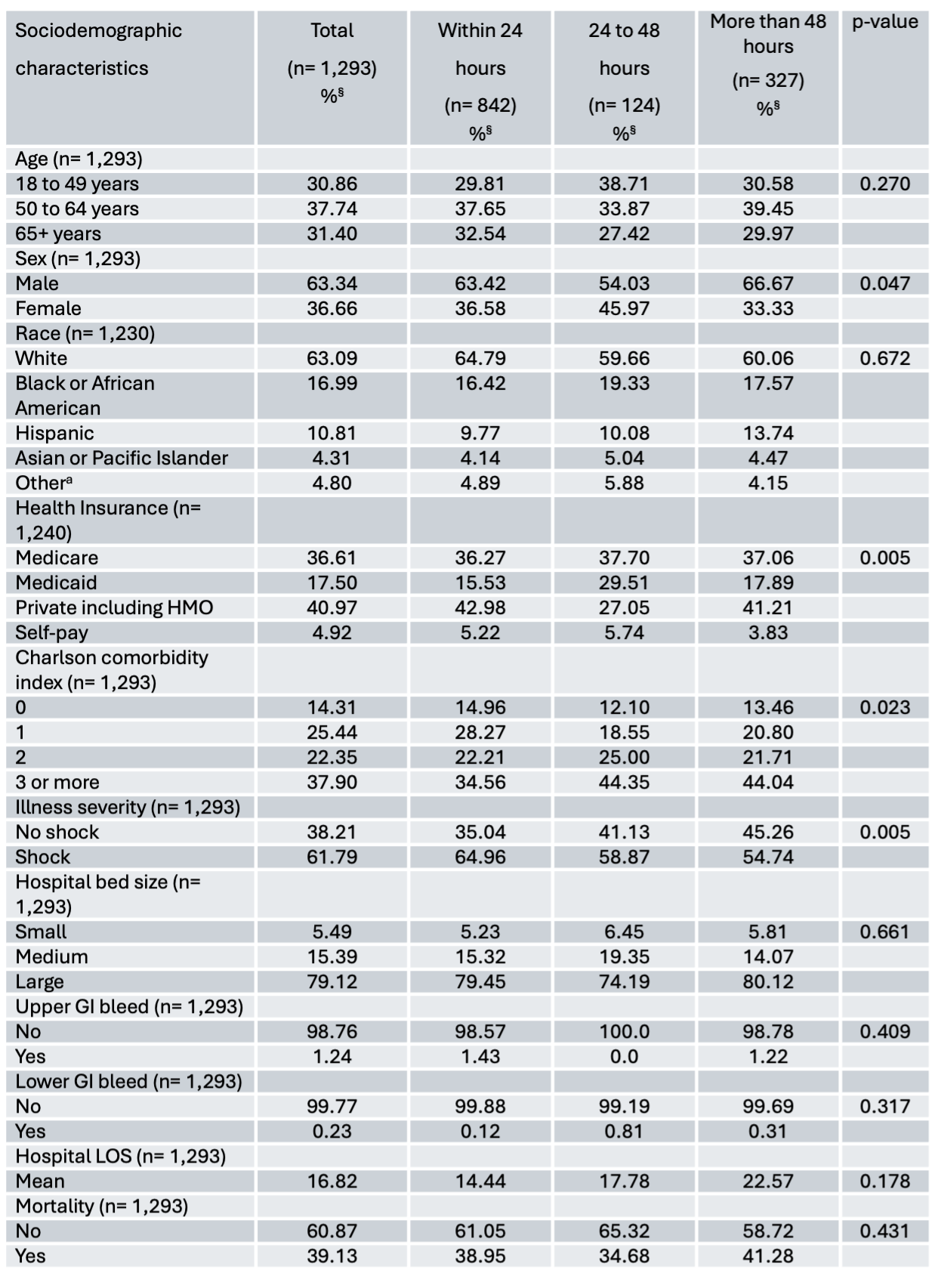
Figure: Table 1: Baseline study population characteristics by timing of ECMO, NIS 2016 to 2020
Disclosures:
Chima Amadi indicated no relevant financial relationships.
Chisom Nwaneki indicated no relevant financial relationships.
Joseph Atarere indicated no relevant financial relationships.
Abisola Ajayi indicated no relevant financial relationships.
Ayomide Sowemimo indicated no relevant financial relationships.
Olanrewaju Adeniran indicated no relevant financial relationships.
Violet Iyahen indicated no relevant financial relationships.
Eunice Omeludike indicated no relevant financial relationships.
Julia Liu indicated no relevant financial relationships.
Chima Amadi, MD, MBA1, Chisom Nwaneki, MD2, Joseph A. Atarere, MBChB, MPH3, Abisola Ajayi, MD1, Ayomide F. Sowemimo, MSc, MD1, Olanrewaju Adeniran, MD4, Violet Iyahen, BS1, Eunice Omeludike, MD5, Julia Liu, MD1. P0941 - Bleeding Under Pressure: Patterns of GI Hemorrhage in ECMO Patients, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
