Sunday Poster Session
Category: GI Bleeding
P0931 - Hospital Readmission and the Impact of Cardiovascular Medications in Patients Presenting With Diverticular Bleeding
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mohammed Abourahma, MD
Loyola University Medical Center
Willowbrook, IL
Presenting Author(s)
Mohammed Abourahma, MD1, Dinkar Ahuja, MD2, Dejan Micic, MD3
1Loyola University Medical Center, Willowbrook, IL; 2Loyola University Medical Center, Chicago, IL; 3Loyola University Medical Center, Maywood, IL
Introduction: Diverticular bleeding is a leading cause of lower gastrointestinal bleeding (LGIB), often presenting as a brisk hemorrhage that resolves spontaneously. Increasingly, presenting individuals have greater cardiovascular (CV) comorbidities requiring antiplatelet (AP) and anticoagulant (AC) therapies. In addition, hospital readmissions are an increasingly scrutinized measure of healthcare quality. This study aimed to evaluate the 30-day readmission rates among individuals presenting with LGIB.
Methods: We conducted a retrospective cohort study of patients >18 years admitted between 1/2014 and 12/2024 with a primary diagnosis of hematochezia or melena who underwent colonoscopy demonstrating diverticulosis. Exclusion criteria were: diverticulitis, IBD, prior colorectal cancer, radiation proctitis, or cirrhosis. The primary outcome of interest was 30-day all-cause readmission, with a secondary outcome of readmission for LGIB. Categorical data were reported as frequencies and proportions. Comparisons were made using Fisher’s exact test; p < 0.05 was considered significant. Adverse events included recurrent CVA, ACS, or DVT/PE within one year of discontinuing AP or AC. Appropriateness of discontinuation was based on ACG guidelines (Sengupta et al., 2023).
Results: Of 182 patients, the median age was 74 years (IQR: 65.0–81.75), and 49.5% were male. Median LOS was 4.5 days (2.78–7.50). Common comorbidities included CVA (13.2%) and CAD (9.9%). Within 30 days, 29 (15.9%) were readmitted for any cause, and 12 (6.6%) for recurrent LGIB. No significant demographic differences were noted with respect to readmission (Table 1). AC discontinuation at discharge occurred in 11 (22%), and AP discontinuation occurred in 16 (17%). Only 50% of AP discontinuations and 18% of AC discontinuations were guideline-concordant. Holding AP or AC on discharge was not associated with a reduction in readmission risk (all-cause or LGIB) (Table 2). Among all-cause readmissions, adverse CV events (i.e., NSTEMI) occurred more often with AP discontinuation (33% vs. 0%, p = 0.19)
Discussion: Our findings demonstrate that holding these CV medications does not reduce the risk of hospital readmission. The majority of medication holds were considered inappropriate and led to numerically higher CV adverse events.
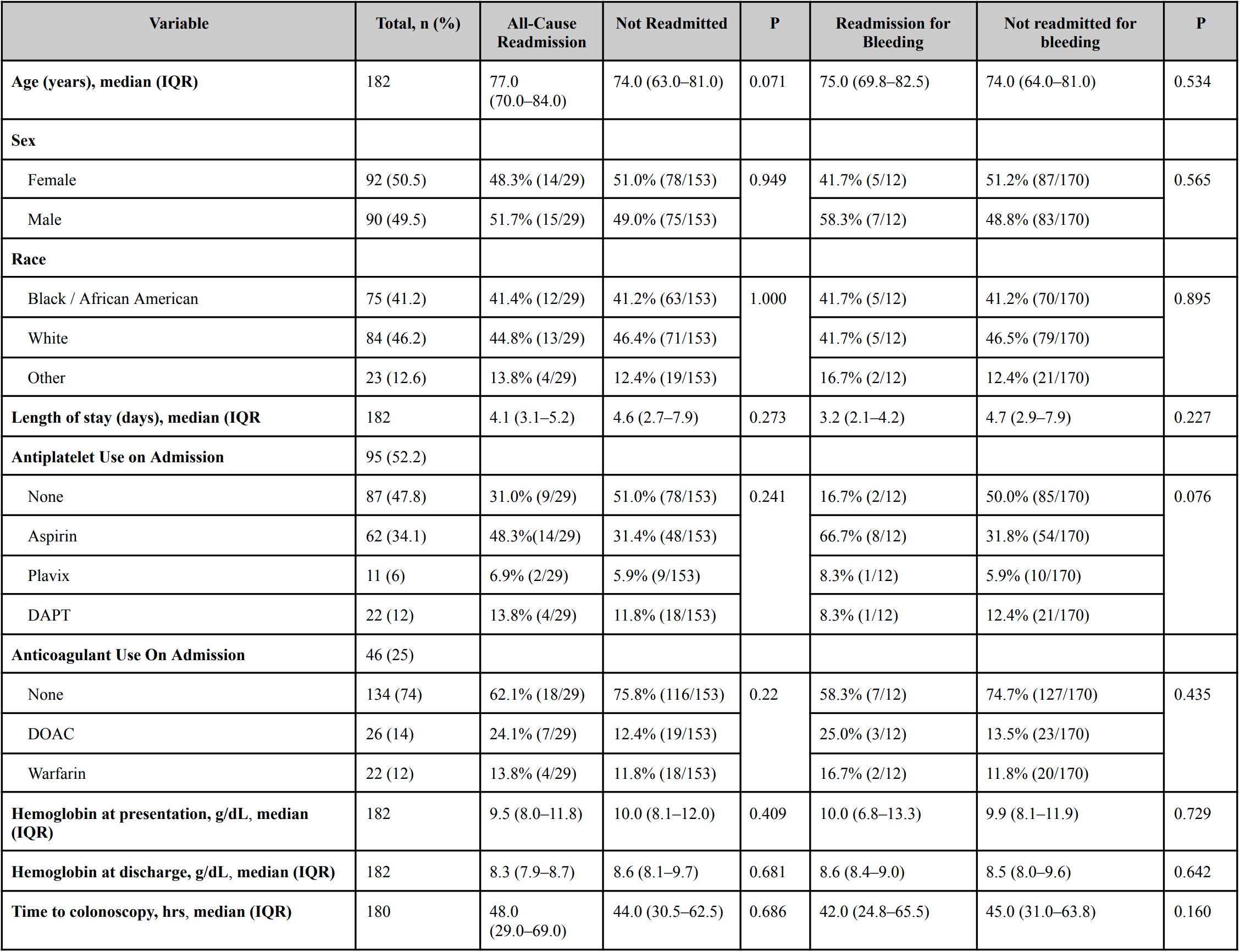
Figure: Baseline and Clinical Characteristics of Patients With Diverticular Bleeding
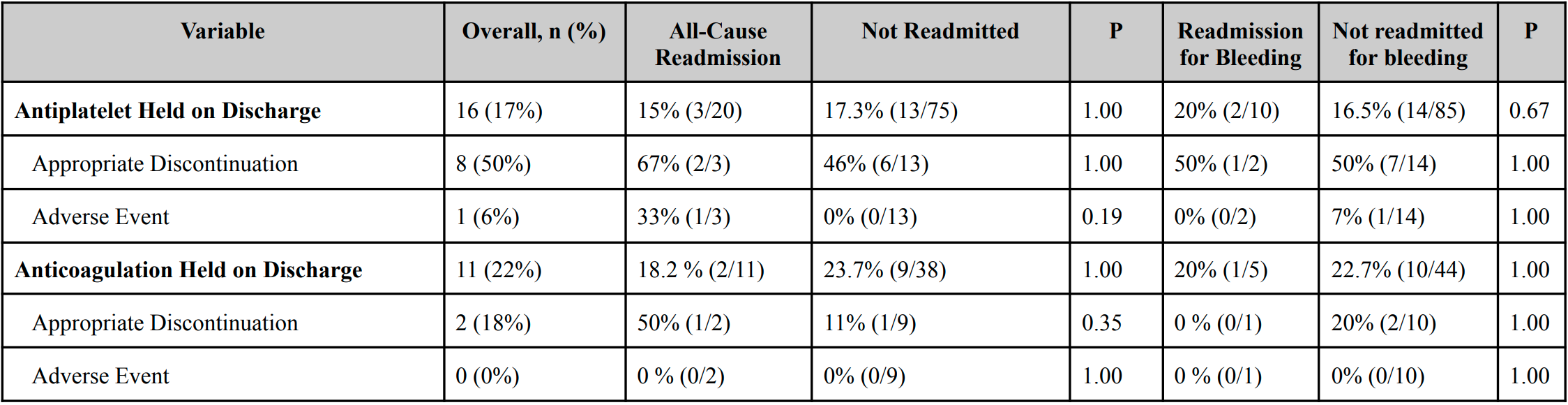
Figure: Impact of Antiplatelet and Anticoagulant Discontinuation on Readmission and Adverse Events
Disclosures:
Mohammed Abourahma indicated no relevant financial relationships.
Dinkar Ahuja indicated no relevant financial relationships.
Dejan Micic indicated no relevant financial relationships.
Mohammed Abourahma, MD1, Dinkar Ahuja, MD2, Dejan Micic, MD3. P0931 - Hospital Readmission and the Impact of Cardiovascular Medications in Patients Presenting With Diverticular Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Loyola University Medical Center, Willowbrook, IL; 2Loyola University Medical Center, Chicago, IL; 3Loyola University Medical Center, Maywood, IL
Introduction: Diverticular bleeding is a leading cause of lower gastrointestinal bleeding (LGIB), often presenting as a brisk hemorrhage that resolves spontaneously. Increasingly, presenting individuals have greater cardiovascular (CV) comorbidities requiring antiplatelet (AP) and anticoagulant (AC) therapies. In addition, hospital readmissions are an increasingly scrutinized measure of healthcare quality. This study aimed to evaluate the 30-day readmission rates among individuals presenting with LGIB.
Methods: We conducted a retrospective cohort study of patients >18 years admitted between 1/2014 and 12/2024 with a primary diagnosis of hematochezia or melena who underwent colonoscopy demonstrating diverticulosis. Exclusion criteria were: diverticulitis, IBD, prior colorectal cancer, radiation proctitis, or cirrhosis. The primary outcome of interest was 30-day all-cause readmission, with a secondary outcome of readmission for LGIB. Categorical data were reported as frequencies and proportions. Comparisons were made using Fisher’s exact test; p < 0.05 was considered significant. Adverse events included recurrent CVA, ACS, or DVT/PE within one year of discontinuing AP or AC. Appropriateness of discontinuation was based on ACG guidelines (Sengupta et al., 2023).
Results: Of 182 patients, the median age was 74 years (IQR: 65.0–81.75), and 49.5% were male. Median LOS was 4.5 days (2.78–7.50). Common comorbidities included CVA (13.2%) and CAD (9.9%). Within 30 days, 29 (15.9%) were readmitted for any cause, and 12 (6.6%) for recurrent LGIB. No significant demographic differences were noted with respect to readmission (Table 1). AC discontinuation at discharge occurred in 11 (22%), and AP discontinuation occurred in 16 (17%). Only 50% of AP discontinuations and 18% of AC discontinuations were guideline-concordant. Holding AP or AC on discharge was not associated with a reduction in readmission risk (all-cause or LGIB) (Table 2). Among all-cause readmissions, adverse CV events (i.e., NSTEMI) occurred more often with AP discontinuation (33% vs. 0%, p = 0.19)
Discussion: Our findings demonstrate that holding these CV medications does not reduce the risk of hospital readmission. The majority of medication holds were considered inappropriate and led to numerically higher CV adverse events.
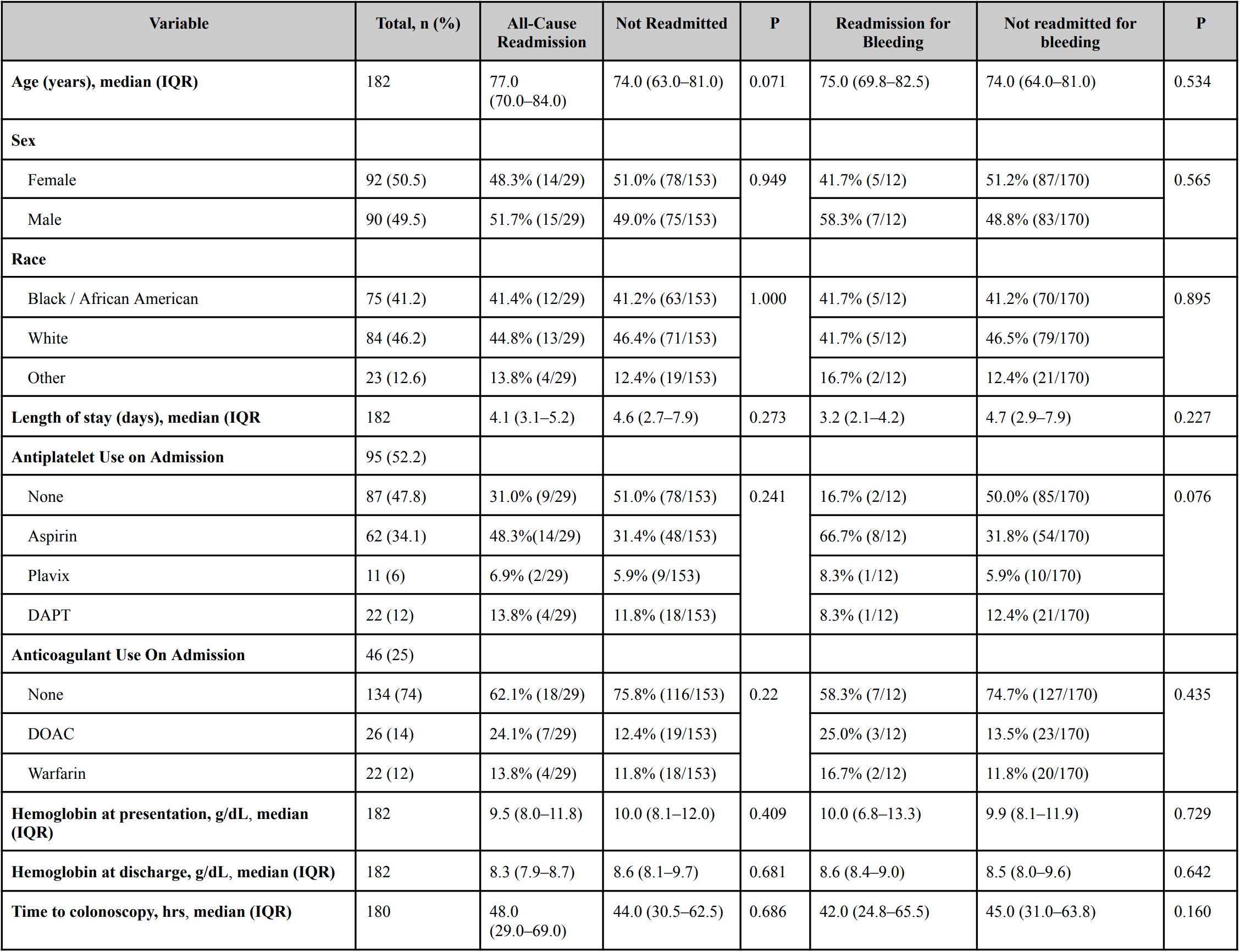
Figure: Baseline and Clinical Characteristics of Patients With Diverticular Bleeding
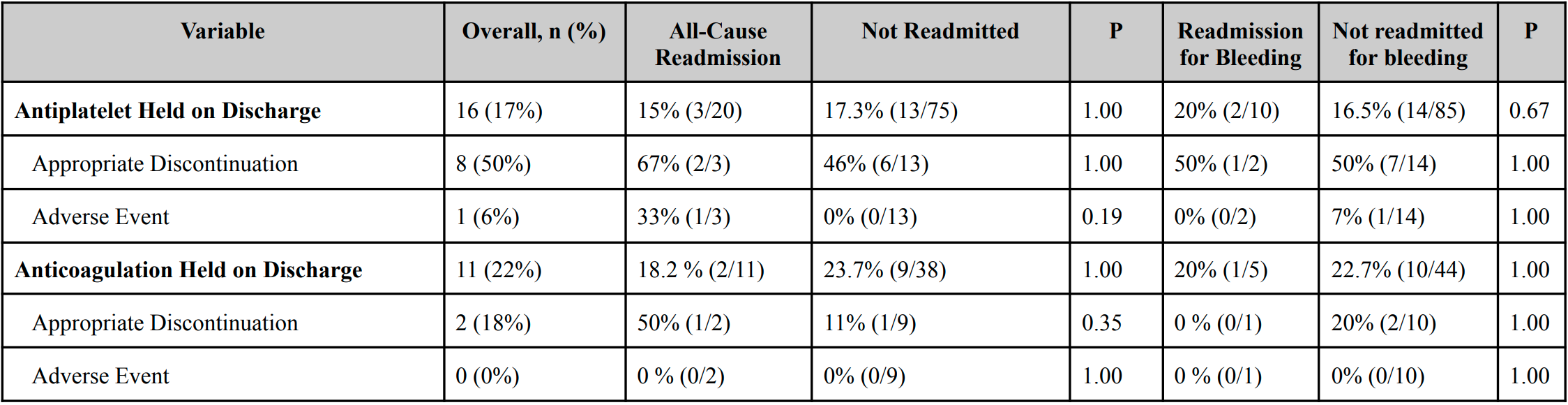
Figure: Impact of Antiplatelet and Anticoagulant Discontinuation on Readmission and Adverse Events
Disclosures:
Mohammed Abourahma indicated no relevant financial relationships.
Dinkar Ahuja indicated no relevant financial relationships.
Dejan Micic indicated no relevant financial relationships.
Mohammed Abourahma, MD1, Dinkar Ahuja, MD2, Dejan Micic, MD3. P0931 - Hospital Readmission and the Impact of Cardiovascular Medications in Patients Presenting With Diverticular Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
