Sunday Poster Session
Category: General Endoscopy
P0898 - Mantle Cell Lymphoma Diverted by Diverticulitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- BM
Blakeley Moorman, MD
University of Louisville School of Medicine
Louisville, KY
Presenting Author(s)
Blakeley Moorman, MD, Ethan R. Steele, DO, Forrest Smith, DO, Kristine Krueger, MD
University of Louisville School of Medicine, Louisville, KY
Introduction: Hematochezia in a stable patient raises suspicion for bleeding from the lower gastrointestinal tract and warrants a broad differential diagnosis. We present a case of recurrent hematochezia and lower abdominal pain with imaging consistent with Acute Diverticulitis (AD) with no active extravasation, who was later diagnosed with Mantle Cell Lymphoma (MCL).
Case Description/
Methods: A 76-year-old female with diverticulosis presented with lower abdominal pain and rectal bleeding. CT abdomen and pelvis revealed sigmoid diverticulitis with mild periaortic, abdominopelvic, and groin adenopathy. CT Angiogram (CTA) showed no active extravasation. Outpatient colonoscopy was arranged in six weeks, but the patient was lost to follow-up until symptom recurrence one year later, with imaging showing persistent sigmoid inflammation and progression of lymphadenopathy.
Six weeks after discharge, outpatient colonoscopy found a cecal polyp, altered mucosal texture and vascularity which was further accentuated under Narrow Band Imaging (NBI). Immunohistochemistry staining of the cecal polyp and mucosa revealed stage IV mantle cell lymphoma.
Discussion: Diverticular disease causes 20-50% of lower gastrointestinal bleeds (LGIB). Other causes include hemorrhoids, vascular malformations and neoplasms. Colonoscopy is useful in identifying the source LGIB but is contraindicated in AD due to perforation risk. In patients with hematochezia in the setting of AD, CTA is utilized to locate active bleeding enabling embolization. However, false negatives occur if there is no active bleeding at time of scan. Regardless of CTA results, AGA guidelines recommend colorectal cancer screening via colonoscopy 4-6 weeks after resolution of AD.
Our patient underwent colonoscopy one year after initial episode of hematochezia. At time of colonoscopy, imaging showed progression of nonspecific abdominopelvic lymphadenopathy, supporting her diagnosis of stage IV MCL.
There is recent push toward abandoning post-AD endoscopic evaluation. This case reemphasizes the importance of adhering to current AGA recommendations of colonoscopy at four to six weeks post-AD to rule out malignancy, especially in the setting of alarm symptoms such as changes in stool caliber, iron deficiency anemia, abdominal pain, blood in stool, and weight changes. Additionally, this case highlights the clinical utility of NBI in evaluating subtle mucosal changes otherwise overlooked with conventional white-light endoscopy.
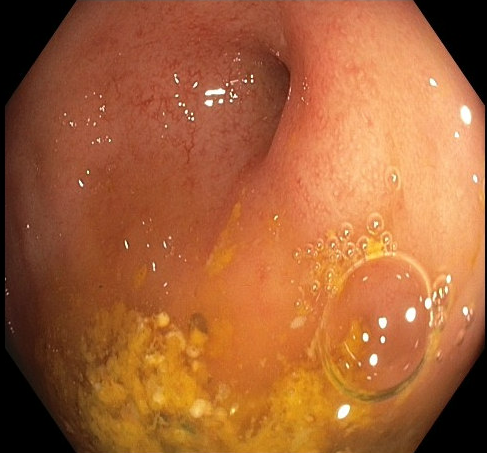
Figure: Abnormal mucosa of appendiceal orifice under white light.
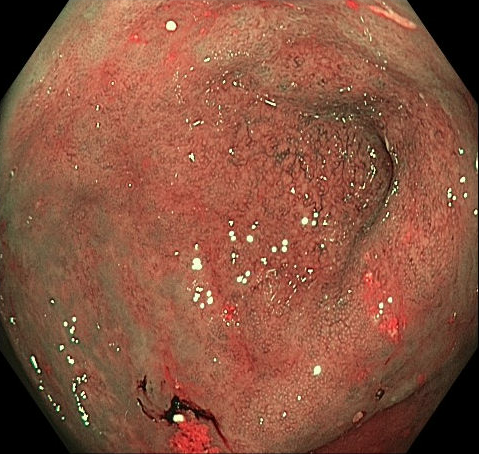
Figure: Abnormal mucosa of appendiceal orifice under Narrow Band Imaging (NBI).
Disclosures:
Blakeley Moorman indicated no relevant financial relationships.
Ethan Steele indicated no relevant financial relationships.
Forrest Smith indicated no relevant financial relationships.
Kristine Krueger indicated no relevant financial relationships.
Blakeley Moorman, MD, Ethan R. Steele, DO, Forrest Smith, DO, Kristine Krueger, MD. P0898 - Mantle Cell Lymphoma Diverted by Diverticulitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Louisville School of Medicine, Louisville, KY
Introduction: Hematochezia in a stable patient raises suspicion for bleeding from the lower gastrointestinal tract and warrants a broad differential diagnosis. We present a case of recurrent hematochezia and lower abdominal pain with imaging consistent with Acute Diverticulitis (AD) with no active extravasation, who was later diagnosed with Mantle Cell Lymphoma (MCL).
Case Description/
Methods: A 76-year-old female with diverticulosis presented with lower abdominal pain and rectal bleeding. CT abdomen and pelvis revealed sigmoid diverticulitis with mild periaortic, abdominopelvic, and groin adenopathy. CT Angiogram (CTA) showed no active extravasation. Outpatient colonoscopy was arranged in six weeks, but the patient was lost to follow-up until symptom recurrence one year later, with imaging showing persistent sigmoid inflammation and progression of lymphadenopathy.
Six weeks after discharge, outpatient colonoscopy found a cecal polyp, altered mucosal texture and vascularity which was further accentuated under Narrow Band Imaging (NBI). Immunohistochemistry staining of the cecal polyp and mucosa revealed stage IV mantle cell lymphoma.
Discussion: Diverticular disease causes 20-50% of lower gastrointestinal bleeds (LGIB). Other causes include hemorrhoids, vascular malformations and neoplasms. Colonoscopy is useful in identifying the source LGIB but is contraindicated in AD due to perforation risk. In patients with hematochezia in the setting of AD, CTA is utilized to locate active bleeding enabling embolization. However, false negatives occur if there is no active bleeding at time of scan. Regardless of CTA results, AGA guidelines recommend colorectal cancer screening via colonoscopy 4-6 weeks after resolution of AD.
Our patient underwent colonoscopy one year after initial episode of hematochezia. At time of colonoscopy, imaging showed progression of nonspecific abdominopelvic lymphadenopathy, supporting her diagnosis of stage IV MCL.
There is recent push toward abandoning post-AD endoscopic evaluation. This case reemphasizes the importance of adhering to current AGA recommendations of colonoscopy at four to six weeks post-AD to rule out malignancy, especially in the setting of alarm symptoms such as changes in stool caliber, iron deficiency anemia, abdominal pain, blood in stool, and weight changes. Additionally, this case highlights the clinical utility of NBI in evaluating subtle mucosal changes otherwise overlooked with conventional white-light endoscopy.
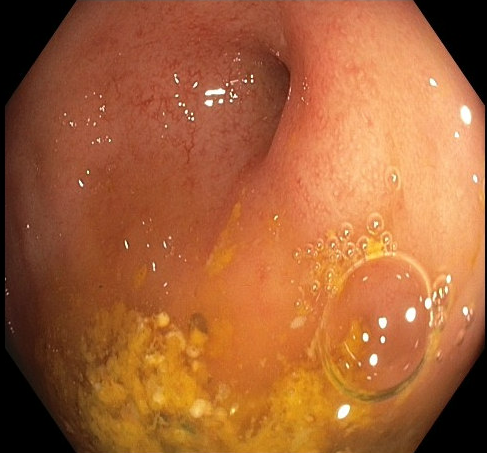
Figure: Abnormal mucosa of appendiceal orifice under white light.
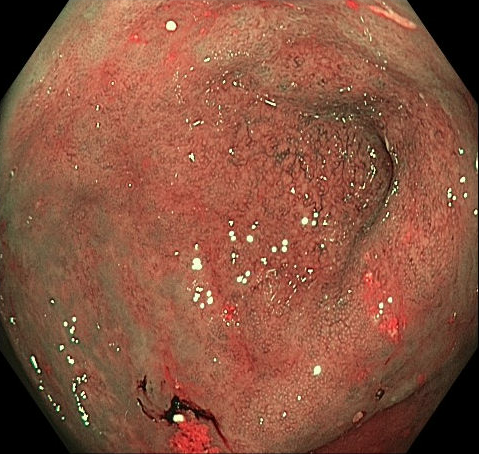
Figure: Abnormal mucosa of appendiceal orifice under Narrow Band Imaging (NBI).
Disclosures:
Blakeley Moorman indicated no relevant financial relationships.
Ethan Steele indicated no relevant financial relationships.
Forrest Smith indicated no relevant financial relationships.
Kristine Krueger indicated no relevant financial relationships.
Blakeley Moorman, MD, Ethan R. Steele, DO, Forrest Smith, DO, Kristine Krueger, MD. P0898 - Mantle Cell Lymphoma Diverted by Diverticulitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

