Sunday Poster Session
Category: General Endoscopy
P0887 - When Laxity Meets Looping: Endoscopic Challenges in Patients With Hypermobility Spectrum Disorder
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Theja V. Channapragada, DO, MBA, MS (he/him/his)
Penn State Health Milton S. Hershey Medical Center
Hershey, PA
Presenting Author(s)
Theja V. Channapragada, DO, MBA, MS1, Maryanna Schweininger, DO2, Divya Penta, BA3, Srinivas Channapragada, MD4, C.S. Pitchumoni, MD, MACG, MPH4
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2Cooper University Hospital, Camden, NJ; 3Rutgers University, New Brunswick, NJ; 4Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Hypermobility spectrum disorder (HSD) is a connective tissue disorder characterized by joint hypermobility and generalized connective tissue laxity. HSD is the more common type of joint hypermobility disorders and often presents with symptoms that overlap with irritable bowel syndrome (IBS), including bloating, abdominal pain, constipation, and diarrhea. These patients frequently undergo gastrointestinal evaluations often without formal diagnosis of HSD. During routine endoscopic practice, we observed that patients with suspected HSD frequently presented with technically difficult colonoscopies due to tortuous colons with excessive colonic looping. We present a case series highlighting these findings and hypothesize that connective tissue abnormalities in HSD may predispose patients to colonic tortuosity, redundancy, and elongation complicating standard endoscopic techniques.
Case Description/
Methods: Five patients with known or suspected HSD underwent screening or diagnostic colonoscopies. All cases were performed by the same gastroenterologist (SC) who encountered significant procedural challenges due to colonic tortuosity, redundancy and looping. See Table 1.
Discussion: This case series suggests that connective tissue abnormalities in HSD may contribute to colonic structural changes that may complicate standard colonoscopic techniques. We propose that anticipating technical challenges in patients with known or suspected HSD can inform pre-procedural planning, such as allocating additional time for the procedure and/or selecting alternative endoscopic equipment and bowel preparation formulas. Second, recognizing this association may reduce the risk of procedural complications, such as perforation or incomplete examinations. Finally, awareness may lead to earlier identification and diagnosis of HSD in patients with recurrent procedural difficulties, especially when other systemic features are present. Educating physicians about simple screening techniques for HSD, such as the Beighton score, and increasing the awareness of HSD’s association with gastrointestinal structural abnormalities can lead to enhanced patient safety, improved procedural effectiveness, and better diagnostic outcomes in this often-underdiagnosed group.
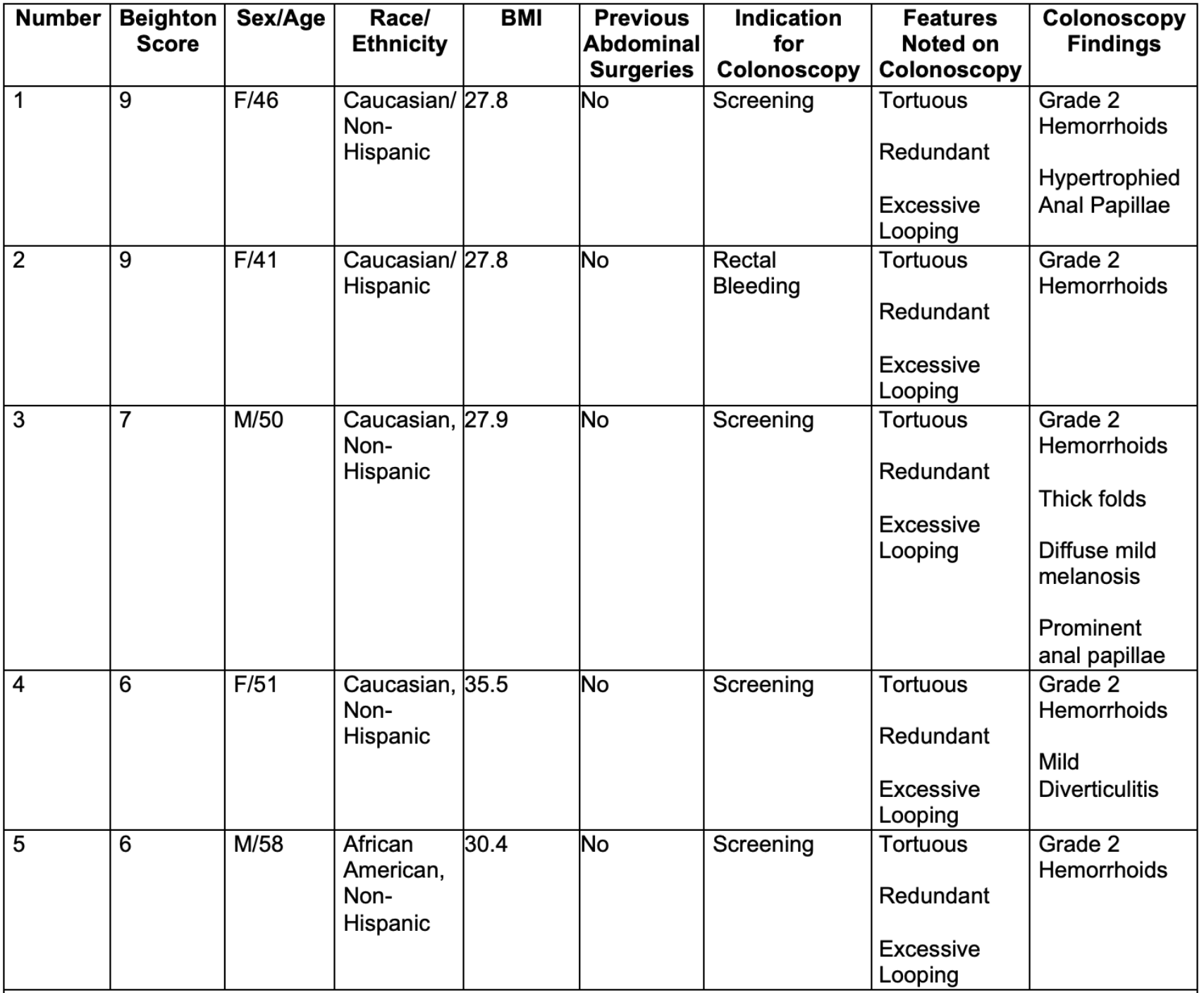
Figure: Table 1: Characteristics and Colonoscopy Findings in Patients of Known or Suspected Hypermobility Spectrum Disorder (HSD). Challenges in colonoscopy were most significant in the left colon, necessitating techniques such as optimal patient positioning, abdominal counter pressure, and scope adjustments due to severe looping, which increased the risk of running out of scope to reach the cecum. While standard colonoscopies usually take approximately 10 to 15 minutes for the operator (SC), these cases took double the time.
Disclosures:
Theja Channapragada indicated no relevant financial relationships.
Maryanna Schweininger indicated no relevant financial relationships.
Divya Penta indicated no relevant financial relationships.
Srinivas Channapragada indicated no relevant financial relationships.
C.S. Pitchumoni indicated no relevant financial relationships.
Theja V. Channapragada, DO, MBA, MS1, Maryanna Schweininger, DO2, Divya Penta, BA3, Srinivas Channapragada, MD4, C.S. Pitchumoni, MD, MACG, MPH4. P0887 - When Laxity Meets Looping: Endoscopic Challenges in Patients With Hypermobility Spectrum Disorder, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2Cooper University Hospital, Camden, NJ; 3Rutgers University, New Brunswick, NJ; 4Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Hypermobility spectrum disorder (HSD) is a connective tissue disorder characterized by joint hypermobility and generalized connective tissue laxity. HSD is the more common type of joint hypermobility disorders and often presents with symptoms that overlap with irritable bowel syndrome (IBS), including bloating, abdominal pain, constipation, and diarrhea. These patients frequently undergo gastrointestinal evaluations often without formal diagnosis of HSD. During routine endoscopic practice, we observed that patients with suspected HSD frequently presented with technically difficult colonoscopies due to tortuous colons with excessive colonic looping. We present a case series highlighting these findings and hypothesize that connective tissue abnormalities in HSD may predispose patients to colonic tortuosity, redundancy, and elongation complicating standard endoscopic techniques.
Case Description/
Methods: Five patients with known or suspected HSD underwent screening or diagnostic colonoscopies. All cases were performed by the same gastroenterologist (SC) who encountered significant procedural challenges due to colonic tortuosity, redundancy and looping. See Table 1.
Discussion: This case series suggests that connective tissue abnormalities in HSD may contribute to colonic structural changes that may complicate standard colonoscopic techniques. We propose that anticipating technical challenges in patients with known or suspected HSD can inform pre-procedural planning, such as allocating additional time for the procedure and/or selecting alternative endoscopic equipment and bowel preparation formulas. Second, recognizing this association may reduce the risk of procedural complications, such as perforation or incomplete examinations. Finally, awareness may lead to earlier identification and diagnosis of HSD in patients with recurrent procedural difficulties, especially when other systemic features are present. Educating physicians about simple screening techniques for HSD, such as the Beighton score, and increasing the awareness of HSD’s association with gastrointestinal structural abnormalities can lead to enhanced patient safety, improved procedural effectiveness, and better diagnostic outcomes in this often-underdiagnosed group.
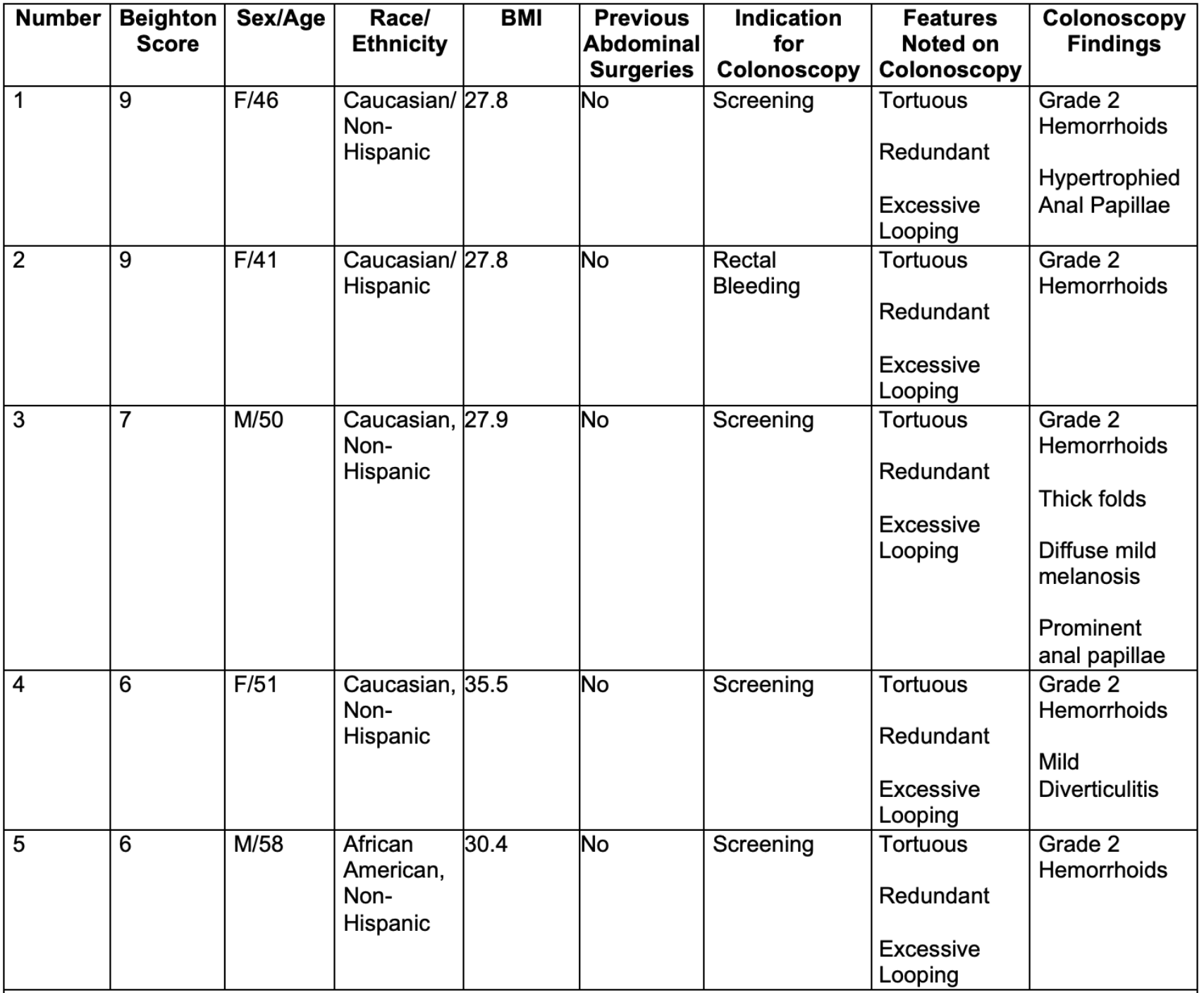
Figure: Table 1: Characteristics and Colonoscopy Findings in Patients of Known or Suspected Hypermobility Spectrum Disorder (HSD). Challenges in colonoscopy were most significant in the left colon, necessitating techniques such as optimal patient positioning, abdominal counter pressure, and scope adjustments due to severe looping, which increased the risk of running out of scope to reach the cecum. While standard colonoscopies usually take approximately 10 to 15 minutes for the operator (SC), these cases took double the time.
Disclosures:
Theja Channapragada indicated no relevant financial relationships.
Maryanna Schweininger indicated no relevant financial relationships.
Divya Penta indicated no relevant financial relationships.
Srinivas Channapragada indicated no relevant financial relationships.
C.S. Pitchumoni indicated no relevant financial relationships.
Theja V. Channapragada, DO, MBA, MS1, Maryanna Schweininger, DO2, Divya Penta, BA3, Srinivas Channapragada, MD4, C.S. Pitchumoni, MD, MACG, MPH4. P0887 - When Laxity Meets Looping: Endoscopic Challenges in Patients With Hypermobility Spectrum Disorder, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
