Sunday Poster Session
Category: General Endoscopy
P0885 - Gastric Bloom: A Rare Case of Flower-Like Lesions in Isolated Gastrointestinal Langerhans Cell Histiocytosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Jameel Alp, MD (he/him/his)
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Jameel Alp, MD1, Timothy Davie, MD2, Samarth Goyal, MD1, Adina Cioc, MD3, Daniela Guerrero Vinsard, MD3
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Langerhans cell histiocytosis (LCH) is a rare clonal proliferation of dendritic cells with variable clinical manifestations. Although LCH is typically observed in children and commonly affects the skin, bones, and pituitary gland, it is rare in adults, with isolated involvement of the gastrointestinal (GI) tract being even more uncommon. We present a case of isolated GI-LCH, incidentally discovered in an asymptomatic patient during an esophagogastroduodenoscopy (EGD), highlighting the critical role of endoscopic and histopathological evaluation in identifying subtle and atypical gastric lesions.
Case Description/
Methods: A 64-year-old otherwise asymptomatic male with a remote history of melanoma and tobacco use disorder was incidentally found to have diffuse esophageal thickening on annual low-dose computerized tomography (CT) of the chest performed for lung cancer screening and was referred to the GI clinic. He reported only occasional heartburn without any other GI symptoms. EGD revealed a normal esophagus, but multiple scattered, small (< 5 mm), flower-like lesions in the gastric body and fundus were found (Fig. 1). Biopsies demonstrated histiocytic infiltration positive for CD1a and S100 on immunohistochemistry (Fig. 2), with confirmation of the BRAF V600E mutation, consistent with LCH. To evaluate disease extent and exclude multisystem involvement, positron emission tomography combined with CT was performed, showing disease confined to the stomach. Given the absence of symptoms and lack of multisystem disease, a surveillance strategy with interval imaging was pursued in collaboration with oncology.
Discussion: Adult LCH is rare, with an estimated annual incidence of 1-2 cases per million. Isolated GI involvement is especially uncommon, with only a few cases reported in the literature. Diagnosis requires histopathologic and immunohistochemical confirmation, often supported by molecular testing for BRAF mutations. This case emphasizes the importance of vigilance and comprehensive diagnostic evaluation with sampling of gastric lesions, even when subtle or atypical, and highlights the need for tailored, patient-centered management through a multidisciplinary approach.
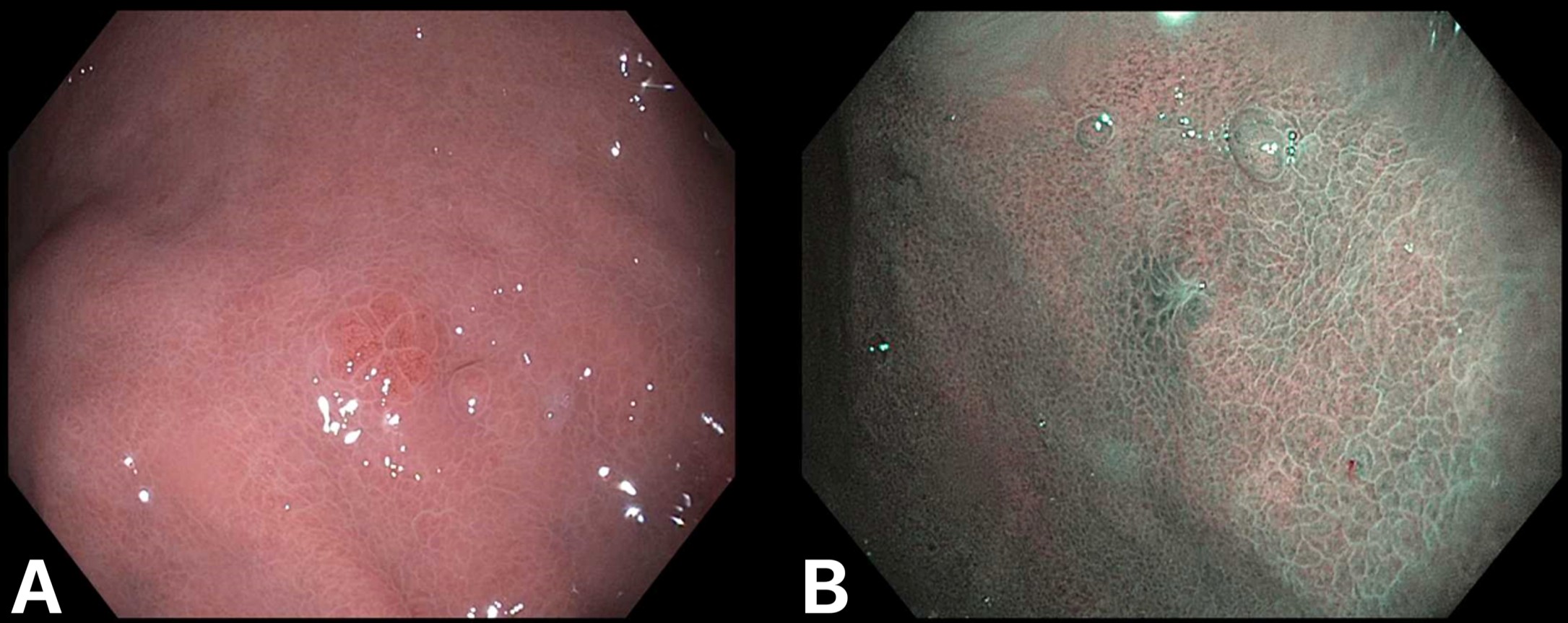
Figure: Figure 1. Endoscopic appearance of gastrointestinal Langerhans cell histiocytosis. (A) Subtle flower-shaped lesion in the gastric body seen with white light. (B) Similar lesion seen with narrow band imaging.
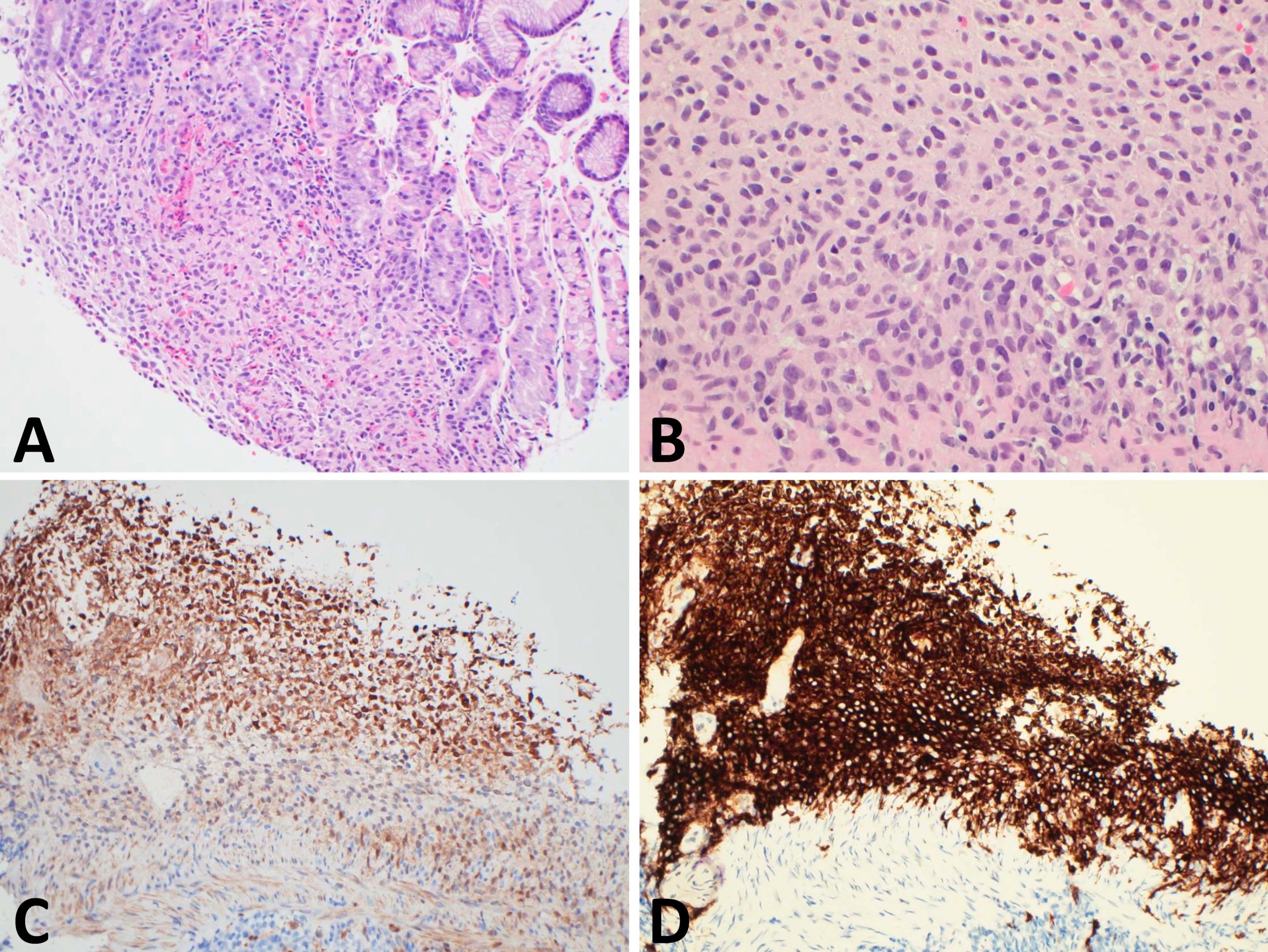
Figure: Figure 2. Histopathologic and immunohistochemical features of gastrointestinal Langerhans cell histiocytosis (LCH). (A) Hematoxylin and eosin (H&E) stain shows expansion of the lamina propria by a dense infiltrate of histiocytes accompanied by eosinophils and small mature lymphocytes (original magnification x200). (B) At higher magnification, histiocytes demonstrate oval to irregular nuclei with occasional nuclear grooves, characteristic of Langerhans cells (H&E, x400). (C) Immunohistochemical staining for S100 protein highlights the lesional cells, confirming histiocytic lineage (x200). (D) Strong membranous staining for CD1a further supports the diagnosis of LCH (x200).
Disclosures:
Jameel Alp indicated no relevant financial relationships.
Timothy Davie indicated no relevant financial relationships.
Samarth Goyal indicated no relevant financial relationships.
Adina Cioc indicated no relevant financial relationships.
Daniela Guerrero Vinsard indicated no relevant financial relationships.
Jameel Alp, MD1, Timothy Davie, MD2, Samarth Goyal, MD1, Adina Cioc, MD3, Daniela Guerrero Vinsard, MD3. P0885 - Gastric Bloom: A Rare Case of Flower-Like Lesions in Isolated Gastrointestinal Langerhans Cell Histiocytosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN; 3University of Minnesota and Minneapolis VA Health Care System, Minneapolis, MN
Introduction: Langerhans cell histiocytosis (LCH) is a rare clonal proliferation of dendritic cells with variable clinical manifestations. Although LCH is typically observed in children and commonly affects the skin, bones, and pituitary gland, it is rare in adults, with isolated involvement of the gastrointestinal (GI) tract being even more uncommon. We present a case of isolated GI-LCH, incidentally discovered in an asymptomatic patient during an esophagogastroduodenoscopy (EGD), highlighting the critical role of endoscopic and histopathological evaluation in identifying subtle and atypical gastric lesions.
Case Description/
Methods: A 64-year-old otherwise asymptomatic male with a remote history of melanoma and tobacco use disorder was incidentally found to have diffuse esophageal thickening on annual low-dose computerized tomography (CT) of the chest performed for lung cancer screening and was referred to the GI clinic. He reported only occasional heartburn without any other GI symptoms. EGD revealed a normal esophagus, but multiple scattered, small (< 5 mm), flower-like lesions in the gastric body and fundus were found (Fig. 1). Biopsies demonstrated histiocytic infiltration positive for CD1a and S100 on immunohistochemistry (Fig. 2), with confirmation of the BRAF V600E mutation, consistent with LCH. To evaluate disease extent and exclude multisystem involvement, positron emission tomography combined with CT was performed, showing disease confined to the stomach. Given the absence of symptoms and lack of multisystem disease, a surveillance strategy with interval imaging was pursued in collaboration with oncology.
Discussion: Adult LCH is rare, with an estimated annual incidence of 1-2 cases per million. Isolated GI involvement is especially uncommon, with only a few cases reported in the literature. Diagnosis requires histopathologic and immunohistochemical confirmation, often supported by molecular testing for BRAF mutations. This case emphasizes the importance of vigilance and comprehensive diagnostic evaluation with sampling of gastric lesions, even when subtle or atypical, and highlights the need for tailored, patient-centered management through a multidisciplinary approach.
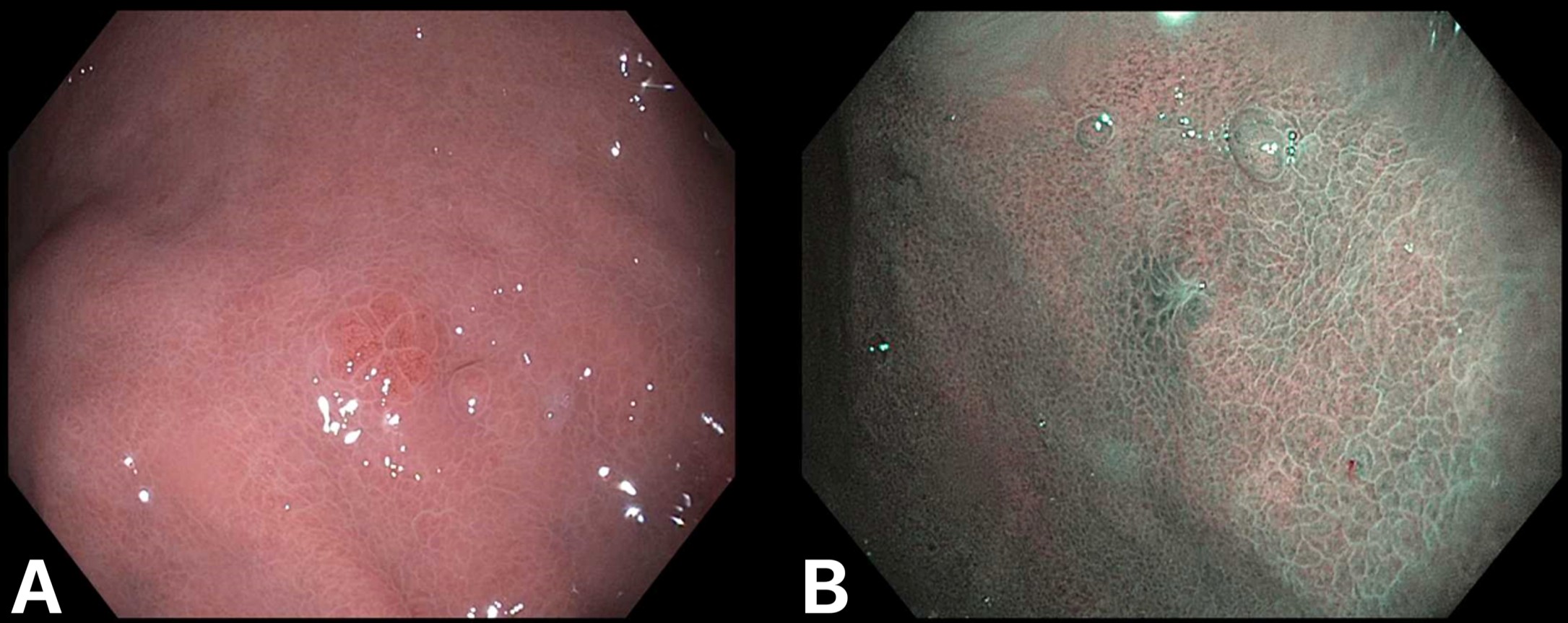
Figure: Figure 1. Endoscopic appearance of gastrointestinal Langerhans cell histiocytosis. (A) Subtle flower-shaped lesion in the gastric body seen with white light. (B) Similar lesion seen with narrow band imaging.
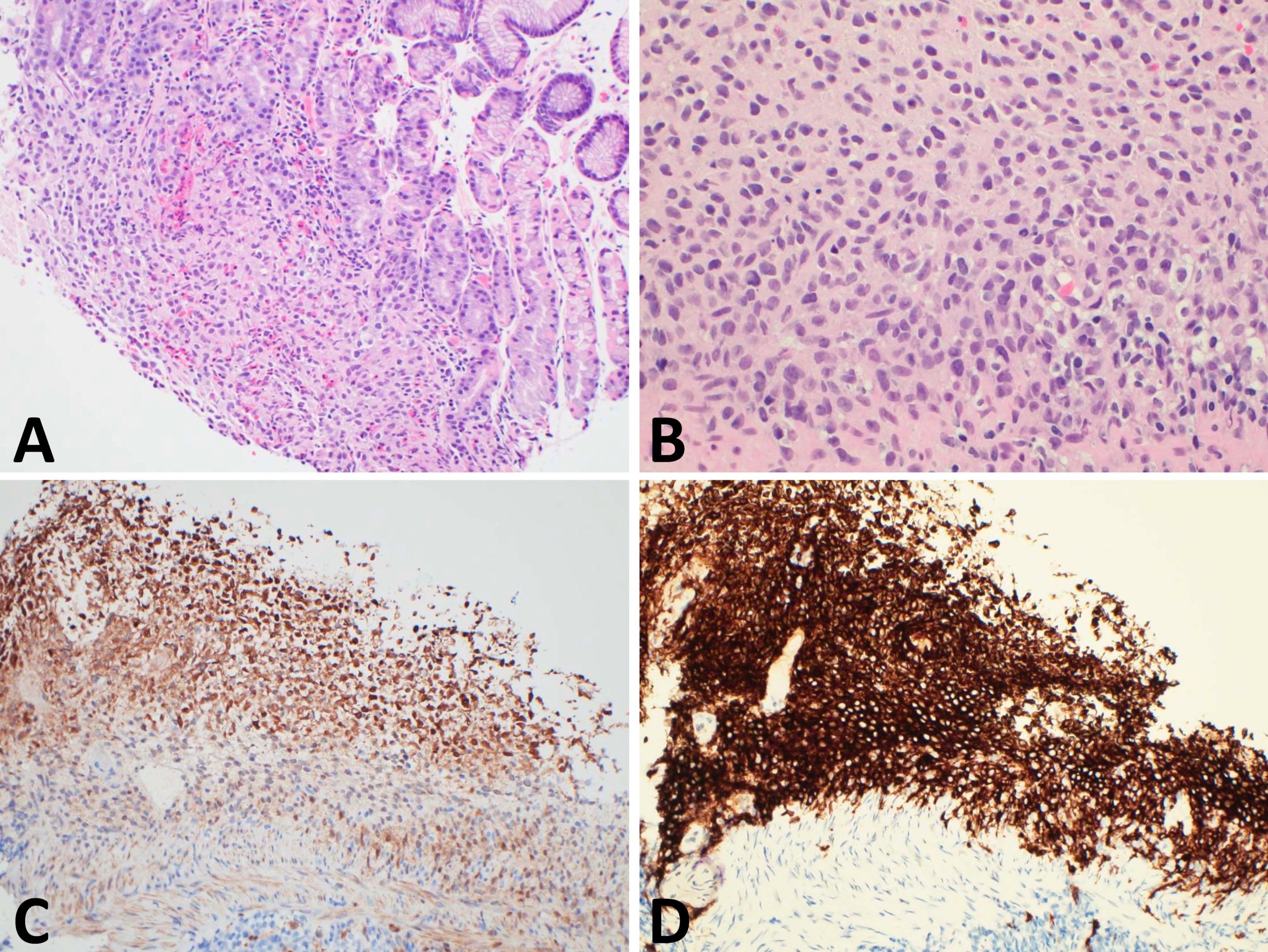
Figure: Figure 2. Histopathologic and immunohistochemical features of gastrointestinal Langerhans cell histiocytosis (LCH). (A) Hematoxylin and eosin (H&E) stain shows expansion of the lamina propria by a dense infiltrate of histiocytes accompanied by eosinophils and small mature lymphocytes (original magnification x200). (B) At higher magnification, histiocytes demonstrate oval to irregular nuclei with occasional nuclear grooves, characteristic of Langerhans cells (H&E, x400). (C) Immunohistochemical staining for S100 protein highlights the lesional cells, confirming histiocytic lineage (x200). (D) Strong membranous staining for CD1a further supports the diagnosis of LCH (x200).
Disclosures:
Jameel Alp indicated no relevant financial relationships.
Timothy Davie indicated no relevant financial relationships.
Samarth Goyal indicated no relevant financial relationships.
Adina Cioc indicated no relevant financial relationships.
Daniela Guerrero Vinsard indicated no relevant financial relationships.
Jameel Alp, MD1, Timothy Davie, MD2, Samarth Goyal, MD1, Adina Cioc, MD3, Daniela Guerrero Vinsard, MD3. P0885 - Gastric Bloom: A Rare Case of Flower-Like Lesions in Isolated Gastrointestinal Langerhans Cell Histiocytosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
