Sunday Poster Session
Category: General Endoscopy
P0884 - Catching the Blood – Splenic and Hepatic Hematoma Following Colonoscopy, A Case Series
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Omar R. Sheikh, MD (he/him/his)
Hackensack Meridian Health - Mountainside Medical Center
Bloomfield, NJ
Presenting Author(s)
Omar R. Sheikh, MD1, Edwin R. Mosquea Gomez, MD2, Muaaz Almerstani, MD3, Minahil A. Khan, MBBS4, Isaac K.. Soliman, MD5
1Hackensack Meridian Health - Mountainside Medical Center, Bloomfield, NJ; 2Hackensack Meridian Health, Bloomfield, NJ; 3HMH mountainside medical center, Clifton, NJ; 4CMH Lahore Medical College, Bloomfield, NJ; 5Hackensack Meridian Health, Montclair, NJ
Introduction: Colonoscopy is generally routine and safe with a complication rate of 2.8/1,000 procedures. When present, these are usually minor bleeding or perforation. We present three cases that were complicated by the developments of hematomas involving the liver or spleen. The estimated incidence of such is reported as 10.63/100,000 (1 in 9400) in-patient colonoscopies, with 10.4% requiring splenectomy.
Case Description/
Methods: A 76-year-old male with a history of chronic kidney disease underwent diagnostic upper and lower endoscopy and had two polyps removed. He presented 24 hours later with generalized abdominal pain, hypotension, and tachycardia. Hemoglobin was 5.1 g/dL. Started on blood transfusions. Computed tomography (CT) of the abdomen showed an enlarged spleen, peri-splenic hematoma, and hemoperitoneum on the left side. Computed tomography angiography (CTA) confirmed high-grade injury with peri-splenic hematoma measuring 13.5 cm, 11 mm Pseudoaneurysm in the splenic hilum, and contrast extravasation anterior to the spleen. Therefore, he was taken for open splenectomy. He required vasopressors and hemodialysis. On post-op day 7, his condition resulted in death.
A 61-year-old female underwent a screening colonoscopy, during which five colonic polyps were removed. In less than 24 hours, she returned with left-sided abdominal pain radiating to her left shoulder, hemodynamically stable, with a hemoglobin of 9.8 g/dL. CT abdomen showed a 1 cm splenic hematoma and a 0.6 cm peri-hepatic hematoma without evidence of perforation. CTA indicated no contrast extravasation to suggest hemorrhage. Managed conservatively with success.
A 50-year-old female underwent a screening colonoscopy with three polyps resected without any immediate complications and was discharged. After a few hours, she returned with left upper quadrant pain that radiated to her shoulder. Hemoglobin was 13.4 g/dL. CT abdomen showed a small peri-splenic hematoma with small hemorrhagic fluid in the pelvis related to grade 1 splenic laceration. Vital signs and hemoglobin were monitored. No surgical intervention was needed.
Discussion: Hematoma formation in the spleen or liver is a severe but rarely observed complication of colonoscopy, and the underlying mechanism is uncertain. Diagnosis should be considered in patients developing abdominal pain following a colonoscopy. The optimal treatment approach is not established, and further studies are required to fully understand pathophysiology and guide preventive measures or standardize treatment.
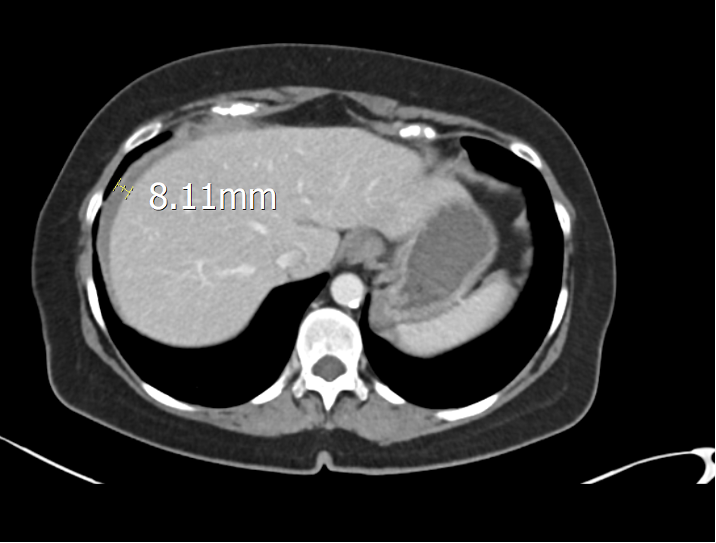
Figure: Computed tomography (abdomen) showing a large peri-splenic hematoma.

Figure: Computed tomography (abdomen) showing a peri-hepatic hematoma.
Disclosures:
Omar Sheikh indicated no relevant financial relationships.
Edwin Mosquea Gomez indicated no relevant financial relationships.
Muaaz Almerstani indicated no relevant financial relationships.
Minahil Khan indicated no relevant financial relationships.
Isaac Soliman indicated no relevant financial relationships.
Omar R. Sheikh, MD1, Edwin R. Mosquea Gomez, MD2, Muaaz Almerstani, MD3, Minahil A. Khan, MBBS4, Isaac K.. Soliman, MD5. P0884 - Catching the Blood – Splenic and Hepatic Hematoma Following Colonoscopy, A Case Series, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Hackensack Meridian Health - Mountainside Medical Center, Bloomfield, NJ; 2Hackensack Meridian Health, Bloomfield, NJ; 3HMH mountainside medical center, Clifton, NJ; 4CMH Lahore Medical College, Bloomfield, NJ; 5Hackensack Meridian Health, Montclair, NJ
Introduction: Colonoscopy is generally routine and safe with a complication rate of 2.8/1,000 procedures. When present, these are usually minor bleeding or perforation. We present three cases that were complicated by the developments of hematomas involving the liver or spleen. The estimated incidence of such is reported as 10.63/100,000 (1 in 9400) in-patient colonoscopies, with 10.4% requiring splenectomy.
Case Description/
Methods: A 76-year-old male with a history of chronic kidney disease underwent diagnostic upper and lower endoscopy and had two polyps removed. He presented 24 hours later with generalized abdominal pain, hypotension, and tachycardia. Hemoglobin was 5.1 g/dL. Started on blood transfusions. Computed tomography (CT) of the abdomen showed an enlarged spleen, peri-splenic hematoma, and hemoperitoneum on the left side. Computed tomography angiography (CTA) confirmed high-grade injury with peri-splenic hematoma measuring 13.5 cm, 11 mm Pseudoaneurysm in the splenic hilum, and contrast extravasation anterior to the spleen. Therefore, he was taken for open splenectomy. He required vasopressors and hemodialysis. On post-op day 7, his condition resulted in death.
A 61-year-old female underwent a screening colonoscopy, during which five colonic polyps were removed. In less than 24 hours, she returned with left-sided abdominal pain radiating to her left shoulder, hemodynamically stable, with a hemoglobin of 9.8 g/dL. CT abdomen showed a 1 cm splenic hematoma and a 0.6 cm peri-hepatic hematoma without evidence of perforation. CTA indicated no contrast extravasation to suggest hemorrhage. Managed conservatively with success.
A 50-year-old female underwent a screening colonoscopy with three polyps resected without any immediate complications and was discharged. After a few hours, she returned with left upper quadrant pain that radiated to her shoulder. Hemoglobin was 13.4 g/dL. CT abdomen showed a small peri-splenic hematoma with small hemorrhagic fluid in the pelvis related to grade 1 splenic laceration. Vital signs and hemoglobin were monitored. No surgical intervention was needed.
Discussion: Hematoma formation in the spleen or liver is a severe but rarely observed complication of colonoscopy, and the underlying mechanism is uncertain. Diagnosis should be considered in patients developing abdominal pain following a colonoscopy. The optimal treatment approach is not established, and further studies are required to fully understand pathophysiology and guide preventive measures or standardize treatment.
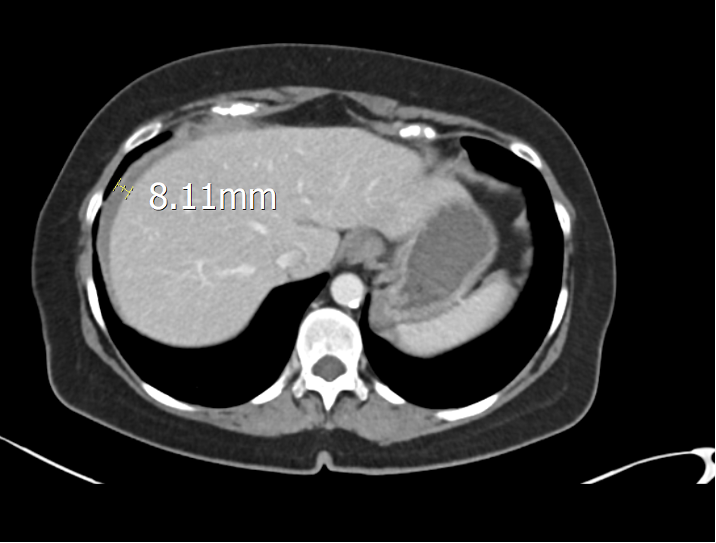
Figure: Computed tomography (abdomen) showing a large peri-splenic hematoma.

Figure: Computed tomography (abdomen) showing a peri-hepatic hematoma.
Disclosures:
Omar Sheikh indicated no relevant financial relationships.
Edwin Mosquea Gomez indicated no relevant financial relationships.
Muaaz Almerstani indicated no relevant financial relationships.
Minahil Khan indicated no relevant financial relationships.
Isaac Soliman indicated no relevant financial relationships.
Omar R. Sheikh, MD1, Edwin R. Mosquea Gomez, MD2, Muaaz Almerstani, MD3, Minahil A. Khan, MBBS4, Isaac K.. Soliman, MD5. P0884 - Catching the Blood – Splenic and Hepatic Hematoma Following Colonoscopy, A Case Series, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

