Sunday Poster Session
Category: General Endoscopy
P0883 - A Rare yet Potentially Deadly Complication: Splenic Injury Following a Colonoscopy
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Fitsum Adane, MD (she/her/hers)
Montefiore New Rochelle
New Rochelle, NY
Presenting Author(s)
Fitsum Adane, MD, Mark Liss, MD, Ghislaine Noumi, MD, John Langley, MD, MBA, Sulav Pyakurel, MD
Montefiore New Rochelle, New Rochelle, NY
Introduction: Colonoscopy is among the most frequently performed elective procedures in the United States, with approximately 11 to 13 million conducted annually. While generally safe, it carries rare risks, including splenic injury—an infrequent but potentially life-threatening complication with an estimated incidence of 0.002%–0.0034%. This report discusses a rare case of post-colonoscopy splenic laceration successfully managed without surgical intervention and emphasizes the importance of recognizing this uncommon complication.
Case Description/
Methods: We present the case of a 59-year-old woman with a complex medical history, including two remote C-sections, one prior uneventful colonoscopy, pulmonary embolism (on apixaban), sickle cell trait, insulin-dependent diabetes, rheumatoid arthritis on Enbrel, HTN, HLD, and PAD, who presented to our GI suite for a routine colonoscopy. Apixaban had been appropriately held for four days pre-procedure. The colonoscopy was technically uneventful. However, upon awakening from anesthesia, she reported acute left upper quadrant (LUQ) pain radiating to the left shoulder, worsened by deep breaths. At the time, her vital signs were stable, and she was admitted for close monitoring. Despite hemodynamic stability and a benign abdominal exam, her persistent LUQ pain prompted further investigation. A non-contrast CT revealed perisplenic fluid and a subsequent CT angiography confirmed a grade II splenic laceration with a stable hematoma and no active extravasation. Given her stable vital signs and hemoglobin level (Hct 36.3%), a multidisciplinary team opted for conservative management. She remained stable throughout her hospital stay without the need for transfusions and was discharged with activity restrictions and careful anticoagulation guidance.
Discussion: This case underscores the importance of maintaining a high index of suspicion for splenic injury when evaluating post-colonoscopy patients with localized LUQ pain associated with/without left shoulder pain. Although most splenic injuries related to colonoscopy present within 24 to 48 hours post-procedure, late presentations have also been reported. Awareness of this potential complication among physicians, including ED doctors is essential for optimal patient outcomes. Early imaging with CT remains the gold standard for diagnosis. Conservative management is appropriate in hemodynamically stable patients with a confined splenic hematoma, while operative measures are necessary for patients with hemodynamic instability.
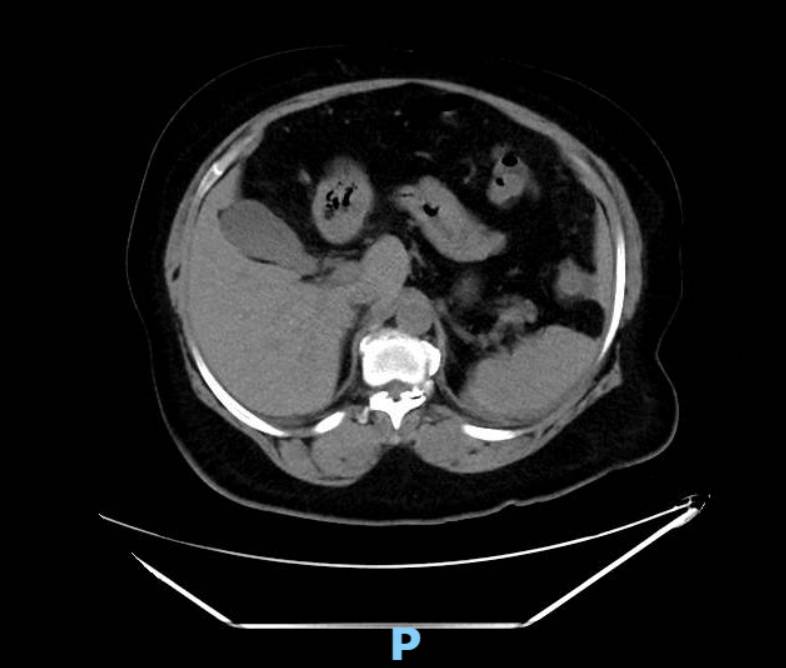
Figure: CTA Chest, Abdomen and Pelvis
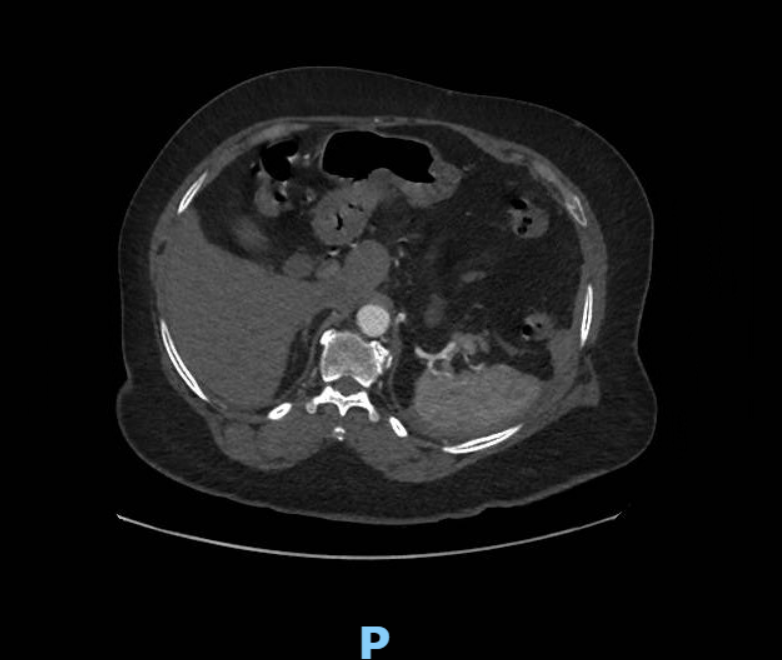
Figure: CT Abdomen and Pelvis without IV Contrast
Disclosures:
Fitsum Adane indicated no relevant financial relationships.
Mark Liss indicated no relevant financial relationships.
Ghislaine Noumi indicated no relevant financial relationships.
John Langley indicated no relevant financial relationships.
Sulav Pyakurel indicated no relevant financial relationships.
Fitsum Adane, MD, Mark Liss, MD, Ghislaine Noumi, MD, John Langley, MD, MBA, Sulav Pyakurel, MD. P0883 - A Rare yet Potentially Deadly Complication: Splenic Injury Following a Colonoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Montefiore New Rochelle, New Rochelle, NY
Introduction: Colonoscopy is among the most frequently performed elective procedures in the United States, with approximately 11 to 13 million conducted annually. While generally safe, it carries rare risks, including splenic injury—an infrequent but potentially life-threatening complication with an estimated incidence of 0.002%–0.0034%. This report discusses a rare case of post-colonoscopy splenic laceration successfully managed without surgical intervention and emphasizes the importance of recognizing this uncommon complication.
Case Description/
Methods: We present the case of a 59-year-old woman with a complex medical history, including two remote C-sections, one prior uneventful colonoscopy, pulmonary embolism (on apixaban), sickle cell trait, insulin-dependent diabetes, rheumatoid arthritis on Enbrel, HTN, HLD, and PAD, who presented to our GI suite for a routine colonoscopy. Apixaban had been appropriately held for four days pre-procedure. The colonoscopy was technically uneventful. However, upon awakening from anesthesia, she reported acute left upper quadrant (LUQ) pain radiating to the left shoulder, worsened by deep breaths. At the time, her vital signs were stable, and she was admitted for close monitoring. Despite hemodynamic stability and a benign abdominal exam, her persistent LUQ pain prompted further investigation. A non-contrast CT revealed perisplenic fluid and a subsequent CT angiography confirmed a grade II splenic laceration with a stable hematoma and no active extravasation. Given her stable vital signs and hemoglobin level (Hct 36.3%), a multidisciplinary team opted for conservative management. She remained stable throughout her hospital stay without the need for transfusions and was discharged with activity restrictions and careful anticoagulation guidance.
Discussion: This case underscores the importance of maintaining a high index of suspicion for splenic injury when evaluating post-colonoscopy patients with localized LUQ pain associated with/without left shoulder pain. Although most splenic injuries related to colonoscopy present within 24 to 48 hours post-procedure, late presentations have also been reported. Awareness of this potential complication among physicians, including ED doctors is essential for optimal patient outcomes. Early imaging with CT remains the gold standard for diagnosis. Conservative management is appropriate in hemodynamically stable patients with a confined splenic hematoma, while operative measures are necessary for patients with hemodynamic instability.
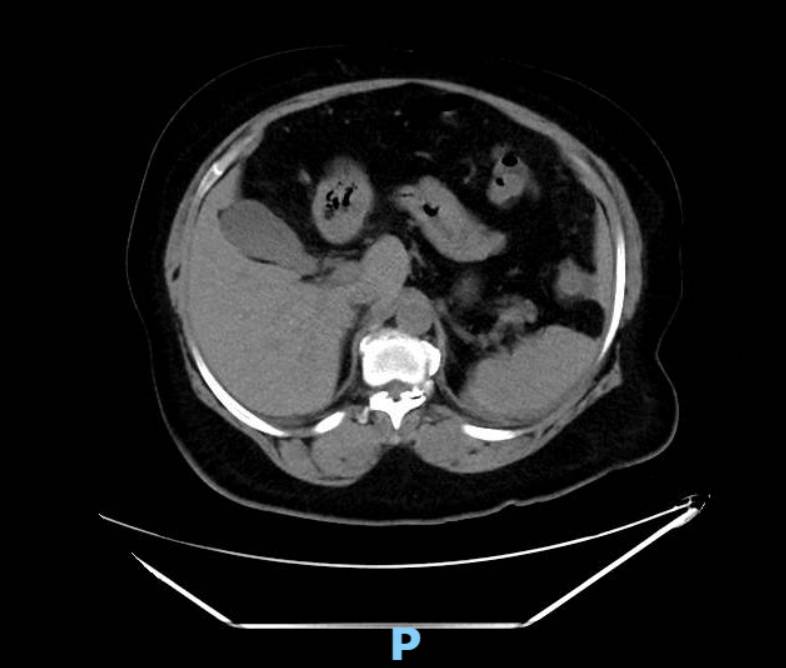
Figure: CTA Chest, Abdomen and Pelvis
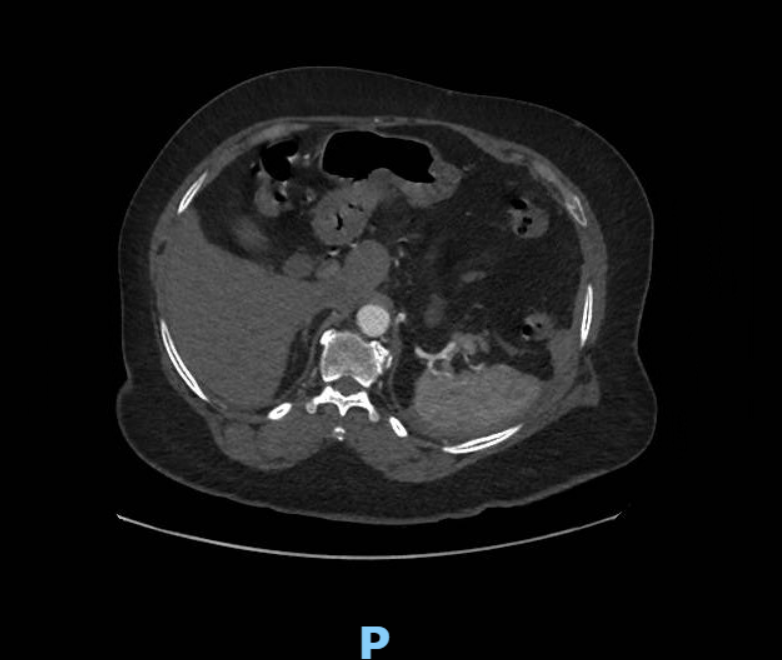
Figure: CT Abdomen and Pelvis without IV Contrast
Disclosures:
Fitsum Adane indicated no relevant financial relationships.
Mark Liss indicated no relevant financial relationships.
Ghislaine Noumi indicated no relevant financial relationships.
John Langley indicated no relevant financial relationships.
Sulav Pyakurel indicated no relevant financial relationships.
Fitsum Adane, MD, Mark Liss, MD, Ghislaine Noumi, MD, John Langley, MD, MBA, Sulav Pyakurel, MD. P0883 - A Rare yet Potentially Deadly Complication: Splenic Injury Following a Colonoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
