Sunday Poster Session
Category: General Endoscopy
P0877 - From Gallstones to Necrosis: A Rare Confluence of Choledocholithiasis and Acute Esophageal Necrosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Eunice Aregbesola, MD (she/her/hers)
University of Missouri Health Care
\, MO
Presenting Author(s)
Eunice Aregbesola, MD1, Ibukunoluwa Oshobu, MD, MPH1, Gopala Konduri, MD2, Nourhan Saleh, MD1, Ervin Tahan, 2, Hanna Nale, DO3, Muhammad Yousaf, MD1
1University of Missouri Health Care, Columbia, MO; 2University of Missouri, Columbia, MO; 3University of Missouri School of Medicine, Columbia, MO
Introduction: Acute esophageal necrosis (AEN), or “black esophagus,” characterized by circumferential black discoloration of the esophageal mucosa with a sharp demarcation with normal mucosa. Its pathogenesis is multifactorial, involving hypoperfusion, mucosal injury from gastric acid, and impaired mucosal defense mechanisms. AEN is associated with critical illness and comorbidities such as coronary artery disease, uncontrolled diabetes, malnutrition, and chronic kidney disease. Although frequently seen in the context of severe systemic illness, its association with choledocholithiasis has not been previously reported. We present a unique case of AEN discovered during the evaluation and management of choledocholithiasis.
Case Description/
Methods: A 77-year-old female with a history of GERD presented with abdominal pain, nausea, and poor oral intake for three days. On arrival, she was febrile (38.1°C) but hemodynamically stable. On exam she had jaundice and RUQ tenderness. Labs revealed leukocytosis (WBC 24.3 × 10⁹/L), high total bilirubin 5.22 mg/dL, direct bilirubin 4.0 mg/dL, ALP 146 U/L, AST 315 U/L, and ALT 103 U/L. Ultrasound and CT abdomen confirmed acute cholecystitis. She underwent laparoscopic cholecystectomy with intraoperative cholangiogram, which demonstrated choledocholithiasis. ERCP was performed, and a common bile duct stone was extracted with a balloon sweep. During insertion of side viewing duodenoscope, diffuse black discoloration of the esophagus with black exudates was noted. This prompted esophageal examination with forward-viewing EGD scope. Given extensive AEN extending up to proximal esophagus, esophageal biopsies were taken. The pathology revealed necro-inflammatory debris and stromal tissue consistent with ulcerative esophagitis, confirming AEN. Patient was managed with high dose of proton pump inhibitors and supportive case. On follow up EGD after 12 weeks EGD showed complete resolution of AEN..
Discussion: This case uniquely highlights the occurrence of AEN in the setting of choledocholithiasis, suggesting that biliary obstruction and its systemic inflammatory response may contribute to esophageal ischemia. The diagnosis of AEN could be missed on side viewing duodenoscope due to limited esophageal visualization. Clinicians should maintain a high index of suspicion for AEN during endoscopic evaluation in acutely ill patients, even when the primary indication is unrelated, such as biliary disease.
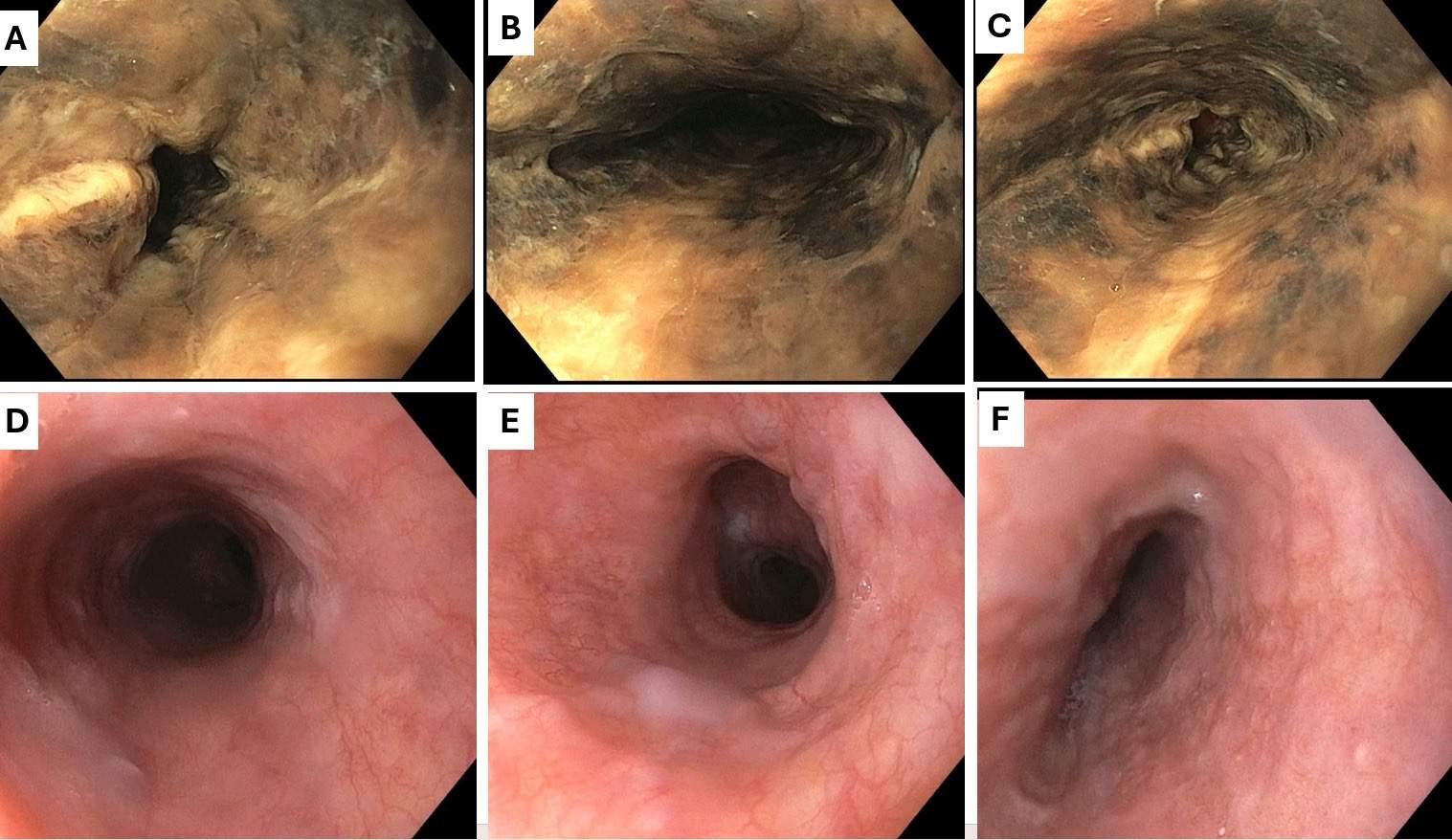
Figure: Fig 1: Initial EGD (panel A, B and C) showing severe acute esophageal necrosis of upper, middle and lower 1/3 of esophagus. Panel D, E and F showed complete resolution of esophageal necrosis of upper, middle and lower 1/3 of esophagus on follow up EGD.
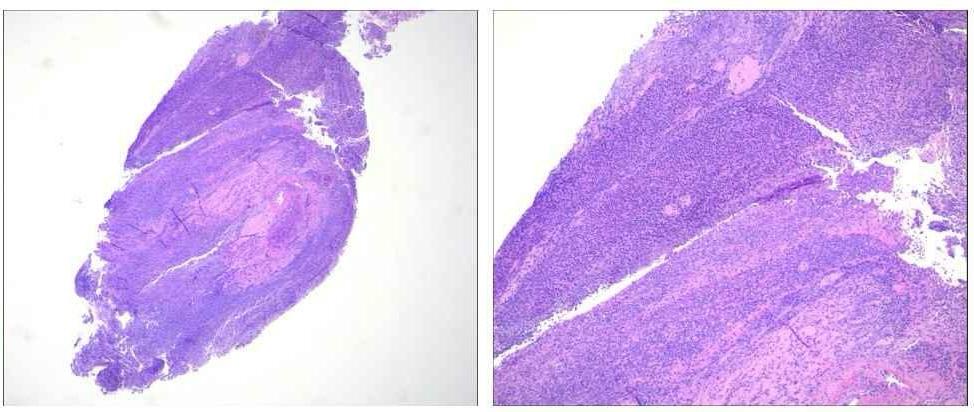
Figure: Fig 2: L-R: H&E stain, 4x: Dense necro-inflammatory debris without residual epithelium.
H&E stain, 10x: Dense acute inflammation extending to submucosa. No residual epithelium present, consistent with ulceration.
Disclosures:
Eunice Aregbesola indicated no relevant financial relationships.
Ibukunoluwa Oshobu indicated no relevant financial relationships.
Gopala Konduri indicated no relevant financial relationships.
Nourhan Saleh indicated no relevant financial relationships.
Ervin Tahan indicated no relevant financial relationships.
Hanna Nale indicated no relevant financial relationships.
Muhammad Yousaf indicated no relevant financial relationships.
Eunice Aregbesola, MD1, Ibukunoluwa Oshobu, MD, MPH1, Gopala Konduri, MD2, Nourhan Saleh, MD1, Ervin Tahan, 2, Hanna Nale, DO3, Muhammad Yousaf, MD1. P0877 - From Gallstones to Necrosis: A Rare Confluence of Choledocholithiasis and Acute Esophageal Necrosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Missouri Health Care, Columbia, MO; 2University of Missouri, Columbia, MO; 3University of Missouri School of Medicine, Columbia, MO
Introduction: Acute esophageal necrosis (AEN), or “black esophagus,” characterized by circumferential black discoloration of the esophageal mucosa with a sharp demarcation with normal mucosa. Its pathogenesis is multifactorial, involving hypoperfusion, mucosal injury from gastric acid, and impaired mucosal defense mechanisms. AEN is associated with critical illness and comorbidities such as coronary artery disease, uncontrolled diabetes, malnutrition, and chronic kidney disease. Although frequently seen in the context of severe systemic illness, its association with choledocholithiasis has not been previously reported. We present a unique case of AEN discovered during the evaluation and management of choledocholithiasis.
Case Description/
Methods: A 77-year-old female with a history of GERD presented with abdominal pain, nausea, and poor oral intake for three days. On arrival, she was febrile (38.1°C) but hemodynamically stable. On exam she had jaundice and RUQ tenderness. Labs revealed leukocytosis (WBC 24.3 × 10⁹/L), high total bilirubin 5.22 mg/dL, direct bilirubin 4.0 mg/dL, ALP 146 U/L, AST 315 U/L, and ALT 103 U/L. Ultrasound and CT abdomen confirmed acute cholecystitis. She underwent laparoscopic cholecystectomy with intraoperative cholangiogram, which demonstrated choledocholithiasis. ERCP was performed, and a common bile duct stone was extracted with a balloon sweep. During insertion of side viewing duodenoscope, diffuse black discoloration of the esophagus with black exudates was noted. This prompted esophageal examination with forward-viewing EGD scope. Given extensive AEN extending up to proximal esophagus, esophageal biopsies were taken. The pathology revealed necro-inflammatory debris and stromal tissue consistent with ulcerative esophagitis, confirming AEN. Patient was managed with high dose of proton pump inhibitors and supportive case. On follow up EGD after 12 weeks EGD showed complete resolution of AEN..
Discussion: This case uniquely highlights the occurrence of AEN in the setting of choledocholithiasis, suggesting that biliary obstruction and its systemic inflammatory response may contribute to esophageal ischemia. The diagnosis of AEN could be missed on side viewing duodenoscope due to limited esophageal visualization. Clinicians should maintain a high index of suspicion for AEN during endoscopic evaluation in acutely ill patients, even when the primary indication is unrelated, such as biliary disease.
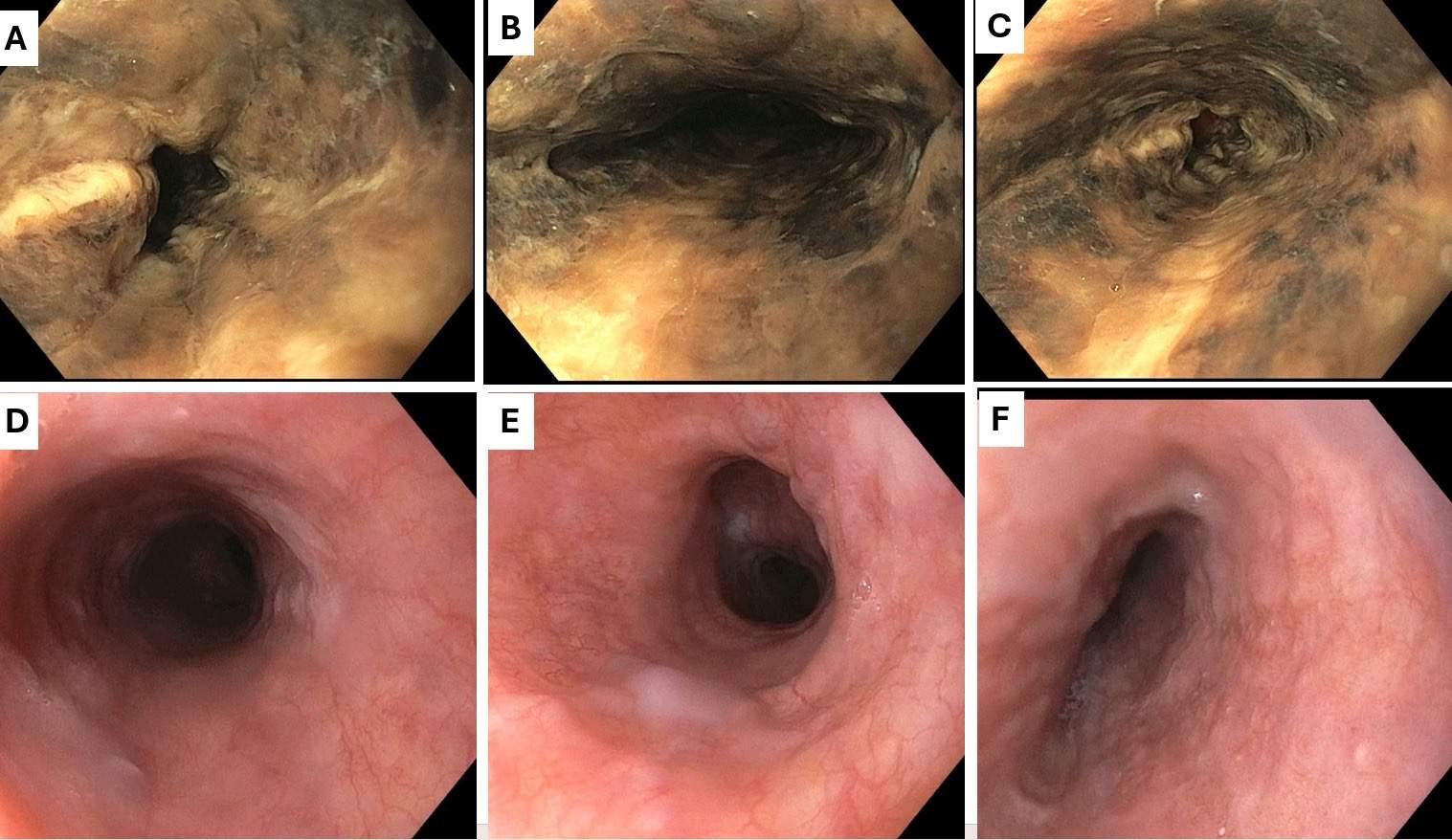
Figure: Fig 1: Initial EGD (panel A, B and C) showing severe acute esophageal necrosis of upper, middle and lower 1/3 of esophagus. Panel D, E and F showed complete resolution of esophageal necrosis of upper, middle and lower 1/3 of esophagus on follow up EGD.
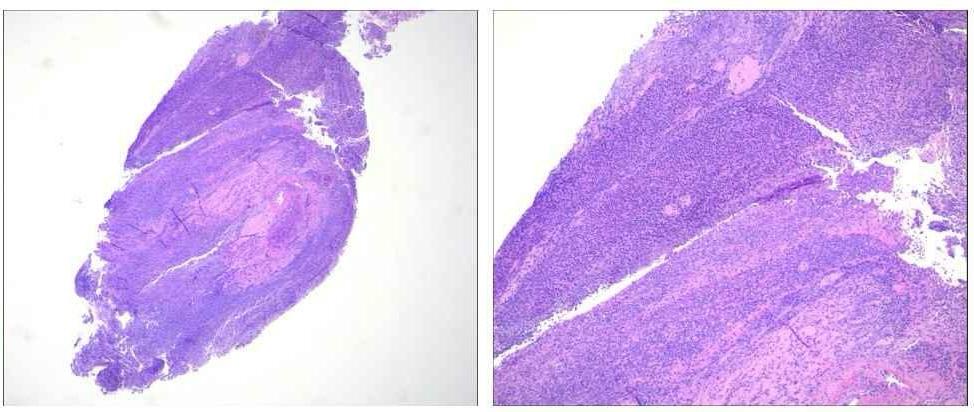
Figure: Fig 2: L-R: H&E stain, 4x: Dense necro-inflammatory debris without residual epithelium.
H&E stain, 10x: Dense acute inflammation extending to submucosa. No residual epithelium present, consistent with ulceration.
Disclosures:
Eunice Aregbesola indicated no relevant financial relationships.
Ibukunoluwa Oshobu indicated no relevant financial relationships.
Gopala Konduri indicated no relevant financial relationships.
Nourhan Saleh indicated no relevant financial relationships.
Ervin Tahan indicated no relevant financial relationships.
Hanna Nale indicated no relevant financial relationships.
Muhammad Yousaf indicated no relevant financial relationships.
Eunice Aregbesola, MD1, Ibukunoluwa Oshobu, MD, MPH1, Gopala Konduri, MD2, Nourhan Saleh, MD1, Ervin Tahan, 2, Hanna Nale, DO3, Muhammad Yousaf, MD1. P0877 - From Gallstones to Necrosis: A Rare Confluence of Choledocholithiasis and Acute Esophageal Necrosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
