Sunday Poster Session
Category: General Endoscopy
P0872 - Feeding Through the Liver: Inadvertent Transhepatic PEG Placement in a Patient With Malignant Esophageal Obstruction
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Pujitha Vallivedu Chennakesavulu, MD, MBBS (she/her/hers)
Quinnipiac University Frank H Netter School of Medicine/ St Vincent medical center
Bridgeport, CT
Presenting Author(s)
Pujitha Vallivedu Chennakesavulu, MD, MBBS1, Sushrut Ingawale, MD, DNB, MBBS2, Akshay Sharma, MBBS3, Archit Garg, MD4, Prabin Sharma, MD5
1Quinnipiac University Frank H Netter School of Medicine/ St Vincent medical center, Bridgeport, CT; 2Quinnipiac University - Frank H Netter MD School of Medicine, Bridgeport, CT; 3Luminis Health Anne Arundel Medical Center, Annapolis, MD; 4Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 5Quinnipiac University - St VIncent Medical Center, Bridgeport, CT
Introduction: Intrahepatic Percutaneous Endoscopic Gastrostomy (PEG) placement is a rare but serious complication with the potential for bleeding and fistulization. We present a case of a mispositioned PEG and explore the rationale and outcomes of conservative management.
Case Description/
Methods: A 65-year-old male with a medical history of esophageal cancer with hepatic metastases presented for oropharyngeal dysphagia. Labs were consistent with anemia, and mild transaminitis. CT abdomen consistent with > 10 bi-lobar hypodense liver lesions with 50 % hepatic tumor parenchyma burden [Image 1]. He was offered an esophageal stent or PEG tube and chose PEG due to potential complications associated with stenting. Repeat esophagogastroduodenoscopy (EGD) successfully traversed the mass. Despite significant tumor burden and hepatomegaly limiting transillumination, a window was identified and PEG was placed. Ten days later, he presented with abdominal pain, erythema, and discomfort at the PEG site. CT abdomen showed the PEG tube passing through a left hepatic metastatic lesion, with the balloon located in the stomach. After multidisciplinary discussion with surgery, gastroenterology, and family, the PEG was retained for enteral nutrition, as there were no signs of decompensation or active bleeding. Chemotherapy was initiated, and following three cycles, the patient demonstrated improved oral intake tolerance. As a result, the PEG was removed, and the gastrocutaneous fistula was successfully closed using cutaneous clips.
Discussion: Gastrostomy and jejunostomy tubes are commonly used to support nutrition in patients with limited oral intake. PEG is generally safe and well-tolerated, with minor complications such as site infection (most common), leakage, dislodgement, or obstruction. However, serious complications such as perforation, peritonitis, bleeding, necrotizing fasciitis, solid organ injury, or buried bumper syndrome can occur. Transhepatic PEG placement is a rare but significant complication, with up to 33% of cases requiring surgical intervention. Placement through a non-mature tract, as in our patient, increases the risk of overt bleeding and gastrohepatic fistula formation. There are no established guidelines for managing this complication. Current literature supports conservative management of leaving the PEG in place when the patient is hemodynamically stable and without signs of acute decompensation. Further research is needed to guide optimal treatment.
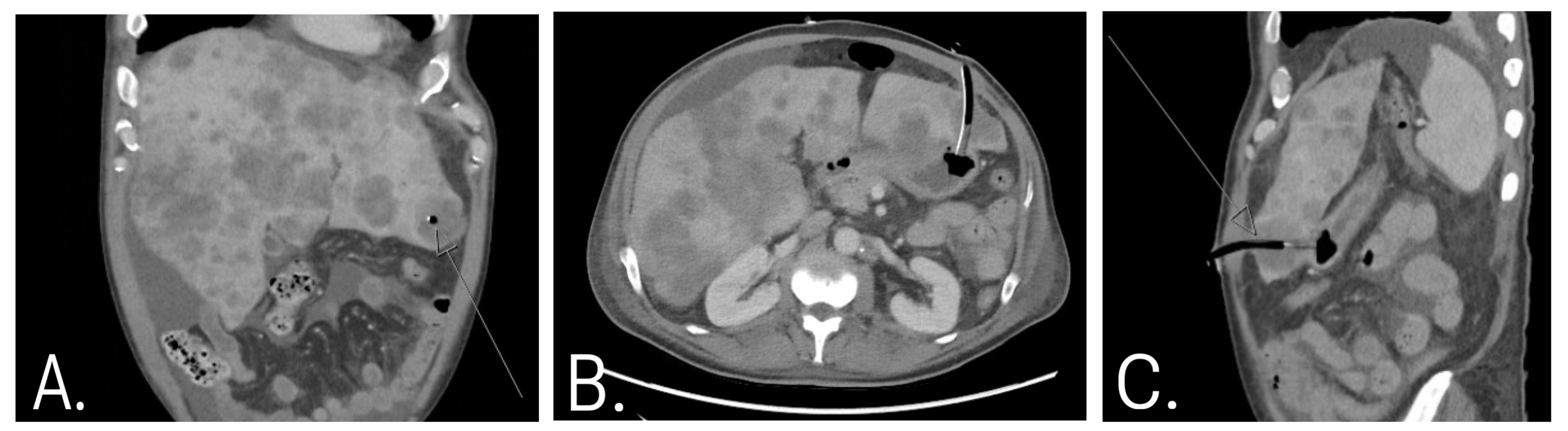
Figure: Image 1: Endoscopic and procedural findings during PEG placement in a patient with esophageal cancer.
A. Friable, ulcerated esophageal mass consistent with malignancy.
B. Endoscopic view of gastric indentation marking the PEG insertion site.
C. Intragastric PEG placement confirmed by visualization of the internal bolster.
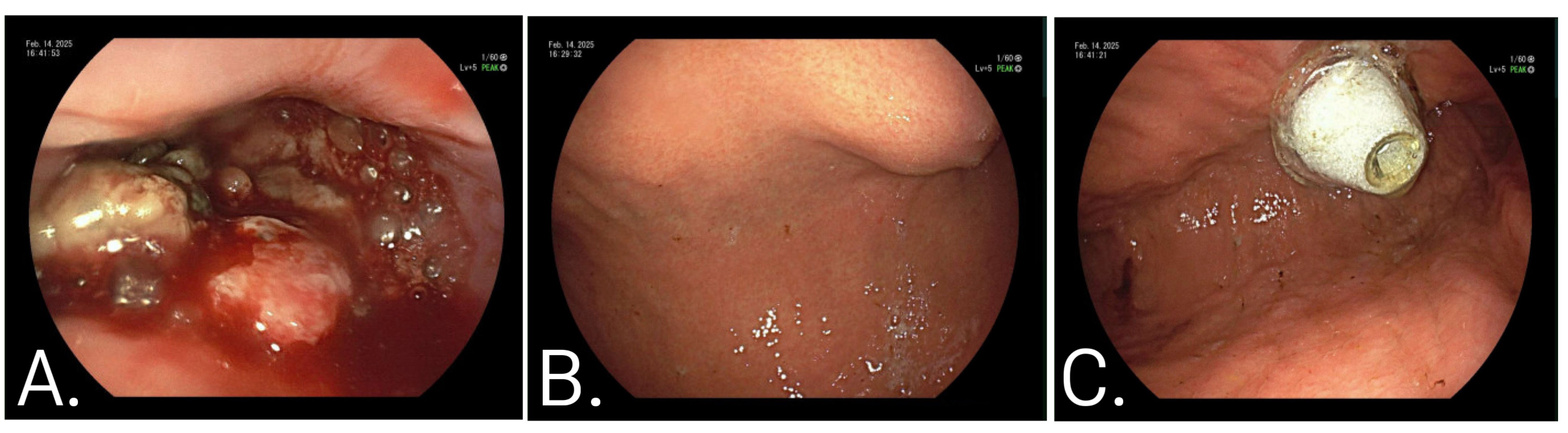
Figure: Image 2: CT abdomen demonstrating intrahepatic PEG tube placement:
A. Coronal view shows the PEG tube traversing the left hepatic lobe.
B. Axial view confirms transhepatic course with the balloon within the gastric lumen.
C. Sagittal view highlights the tube’s intrahepatic path terminating in the stomach.
Disclosures:
Pujitha Vallivedu Chennakesavulu indicated no relevant financial relationships.
Sushrut Ingawale indicated no relevant financial relationships.
Akshay Sharma indicated no relevant financial relationships.
Archit Garg indicated no relevant financial relationships.
Prabin Sharma indicated no relevant financial relationships.
Pujitha Vallivedu Chennakesavulu, MD, MBBS1, Sushrut Ingawale, MD, DNB, MBBS2, Akshay Sharma, MBBS3, Archit Garg, MD4, Prabin Sharma, MD5. P0872 - Feeding Through the Liver: Inadvertent Transhepatic PEG Placement in a Patient With Malignant Esophageal Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Quinnipiac University Frank H Netter School of Medicine/ St Vincent medical center, Bridgeport, CT; 2Quinnipiac University - Frank H Netter MD School of Medicine, Bridgeport, CT; 3Luminis Health Anne Arundel Medical Center, Annapolis, MD; 4Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 5Quinnipiac University - St VIncent Medical Center, Bridgeport, CT
Introduction: Intrahepatic Percutaneous Endoscopic Gastrostomy (PEG) placement is a rare but serious complication with the potential for bleeding and fistulization. We present a case of a mispositioned PEG and explore the rationale and outcomes of conservative management.
Case Description/
Methods: A 65-year-old male with a medical history of esophageal cancer with hepatic metastases presented for oropharyngeal dysphagia. Labs were consistent with anemia, and mild transaminitis. CT abdomen consistent with > 10 bi-lobar hypodense liver lesions with 50 % hepatic tumor parenchyma burden [Image 1]. He was offered an esophageal stent or PEG tube and chose PEG due to potential complications associated with stenting. Repeat esophagogastroduodenoscopy (EGD) successfully traversed the mass. Despite significant tumor burden and hepatomegaly limiting transillumination, a window was identified and PEG was placed. Ten days later, he presented with abdominal pain, erythema, and discomfort at the PEG site. CT abdomen showed the PEG tube passing through a left hepatic metastatic lesion, with the balloon located in the stomach. After multidisciplinary discussion with surgery, gastroenterology, and family, the PEG was retained for enteral nutrition, as there were no signs of decompensation or active bleeding. Chemotherapy was initiated, and following three cycles, the patient demonstrated improved oral intake tolerance. As a result, the PEG was removed, and the gastrocutaneous fistula was successfully closed using cutaneous clips.
Discussion: Gastrostomy and jejunostomy tubes are commonly used to support nutrition in patients with limited oral intake. PEG is generally safe and well-tolerated, with minor complications such as site infection (most common), leakage, dislodgement, or obstruction. However, serious complications such as perforation, peritonitis, bleeding, necrotizing fasciitis, solid organ injury, or buried bumper syndrome can occur. Transhepatic PEG placement is a rare but significant complication, with up to 33% of cases requiring surgical intervention. Placement through a non-mature tract, as in our patient, increases the risk of overt bleeding and gastrohepatic fistula formation. There are no established guidelines for managing this complication. Current literature supports conservative management of leaving the PEG in place when the patient is hemodynamically stable and without signs of acute decompensation. Further research is needed to guide optimal treatment.
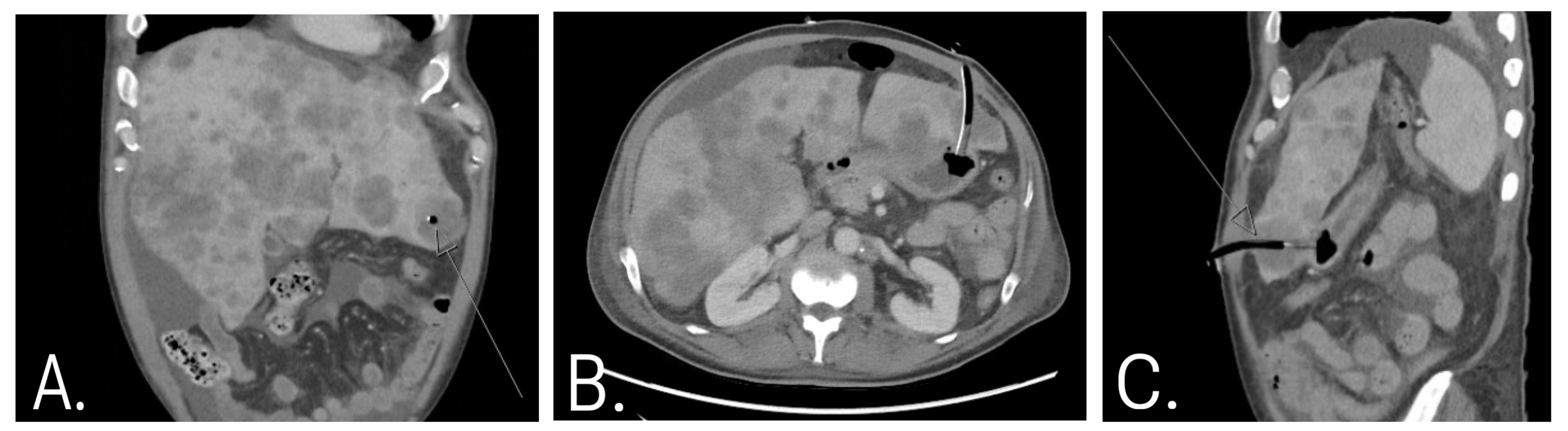
Figure: Image 1: Endoscopic and procedural findings during PEG placement in a patient with esophageal cancer.
A. Friable, ulcerated esophageal mass consistent with malignancy.
B. Endoscopic view of gastric indentation marking the PEG insertion site.
C. Intragastric PEG placement confirmed by visualization of the internal bolster.
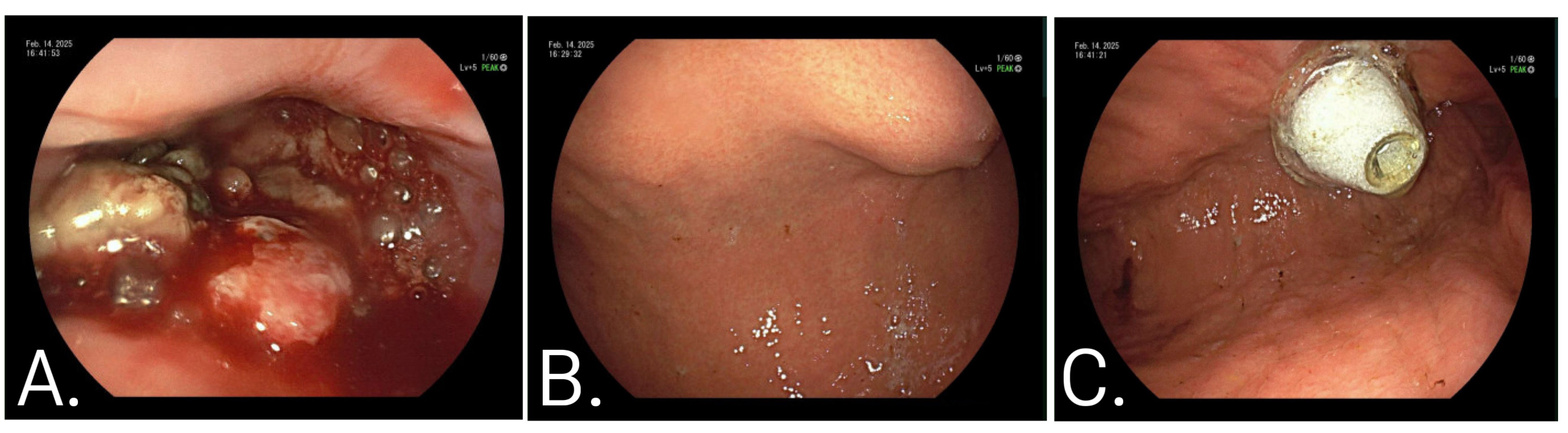
Figure: Image 2: CT abdomen demonstrating intrahepatic PEG tube placement:
A. Coronal view shows the PEG tube traversing the left hepatic lobe.
B. Axial view confirms transhepatic course with the balloon within the gastric lumen.
C. Sagittal view highlights the tube’s intrahepatic path terminating in the stomach.
Disclosures:
Pujitha Vallivedu Chennakesavulu indicated no relevant financial relationships.
Sushrut Ingawale indicated no relevant financial relationships.
Akshay Sharma indicated no relevant financial relationships.
Archit Garg indicated no relevant financial relationships.
Prabin Sharma indicated no relevant financial relationships.
Pujitha Vallivedu Chennakesavulu, MD, MBBS1, Sushrut Ingawale, MD, DNB, MBBS2, Akshay Sharma, MBBS3, Archit Garg, MD4, Prabin Sharma, MD5. P0872 - Feeding Through the Liver: Inadvertent Transhepatic PEG Placement in a Patient With Malignant Esophageal Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
