Sunday Poster Session
Category: General Endoscopy
P0857 - Re-Examining Computer-Aided Polyp Detection in the Era of a New Quality Benchmark: A Meta-Analysis of ADR, PDR, and SSLDR
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Tasnim Ahmed, MD
Beth Israel Deaconess Medical Center
Boston, MA
Presenting Author(s)
Tasnim Ahmed, MD1, Faisal S. Ali, MD1, Rachel Hicklen, MS2, Tyler M. Berzin, MD1
1Beth Israel Deaconess Medical Center, Boston, MA; 2University of Texas MD Anderson Cancer Center, Houston, TX
Introduction: In 2024, the American College of Gastroenterology (ACG) and the American Society for Gastrointestinal Endoscopy (ASGE) updated quality benchmarks for colonoscopy, highlighting adenoma detection rate (ADR) and introducing sessile serrated lesion detection rate (SSLDR) as a new priority quality indicator. While studies have examined the impact of artificial intelligence (AI)-assisted colonoscopy on ADR and polyp detection rate (PDR), no prior meta-analysis has systematically evaluated SSLDR in this context. We conducted a comprehensive meta-analysis of randomized controlled trials (RCTs) published through March 2025 to evaluate the effects of computer-aided detection (CADe) on ADR, PDR, and SSLDR.
Methods: We conducted a systematic review of Ovid Embase and Ovid MEDLINE to identify RCTs that compared AI-assisted colonoscopies with control. Random-effects meta-analyses were performed to compare the effect of computer assisted detection (CADe) on ADR, PDR, and SSLDR in colonoscopies.
Results: A total of 50 systematic reviews were included in our analysis and met inclusion criteria. 45 were used for ADR meta-analysis, 36 for PDR meta-analysis, and 25 for SSLDR meta-analysis. Overall, ADR, PDR, and SSLDR were all significantly higher with CADe than without. ADR was 21% higher in AI-assisted colonoscopies (44.68%) than those without (37.65%) (risk ratio [RR] 1.21, 95% confidence interval [CI] 1.16-1.26 I2 55.66%) (Figure 1). In the studies that included SSLDR data, SSDLDR was also significantly higher in CADe colonoscopies (8.66%) than those without (7.49%) (RR 1.17 95 % CI 1.04-1.32 I2 21.15%) (Figure 2). The risk difference for SSLDR was 0.01 between intervention and control arms (95% CI 0.000-.0135 I2 35.61%) (Figure 2). Finally, PDR, often used as a surrogate marker for ADR in studies, was 19% higher in AI-assisted colonoscopies (56.89%) than control (49.32%) (RR 1.19 95% CI 1.14-1.23 I2 70.64%) (Figure 1).
Discussion: CADe using artificial intelligence improves the quality of colonoscopies, using indicators determined by the newest ACG and AGSE guidelines. While both ADR (performance target > 35%) and SSLDR (performance target > 6%) were improved with CADe, the risk difference in SSLDR was minimal at 0.01. Given the degree of heterogeneity, it is important to standardize methods for future trials and may warrant further subgroup analyses. As CADe systems advance, they should be explicitly trained and validated for SSLDR to support newer colonoscopy quality benchmark expectations.
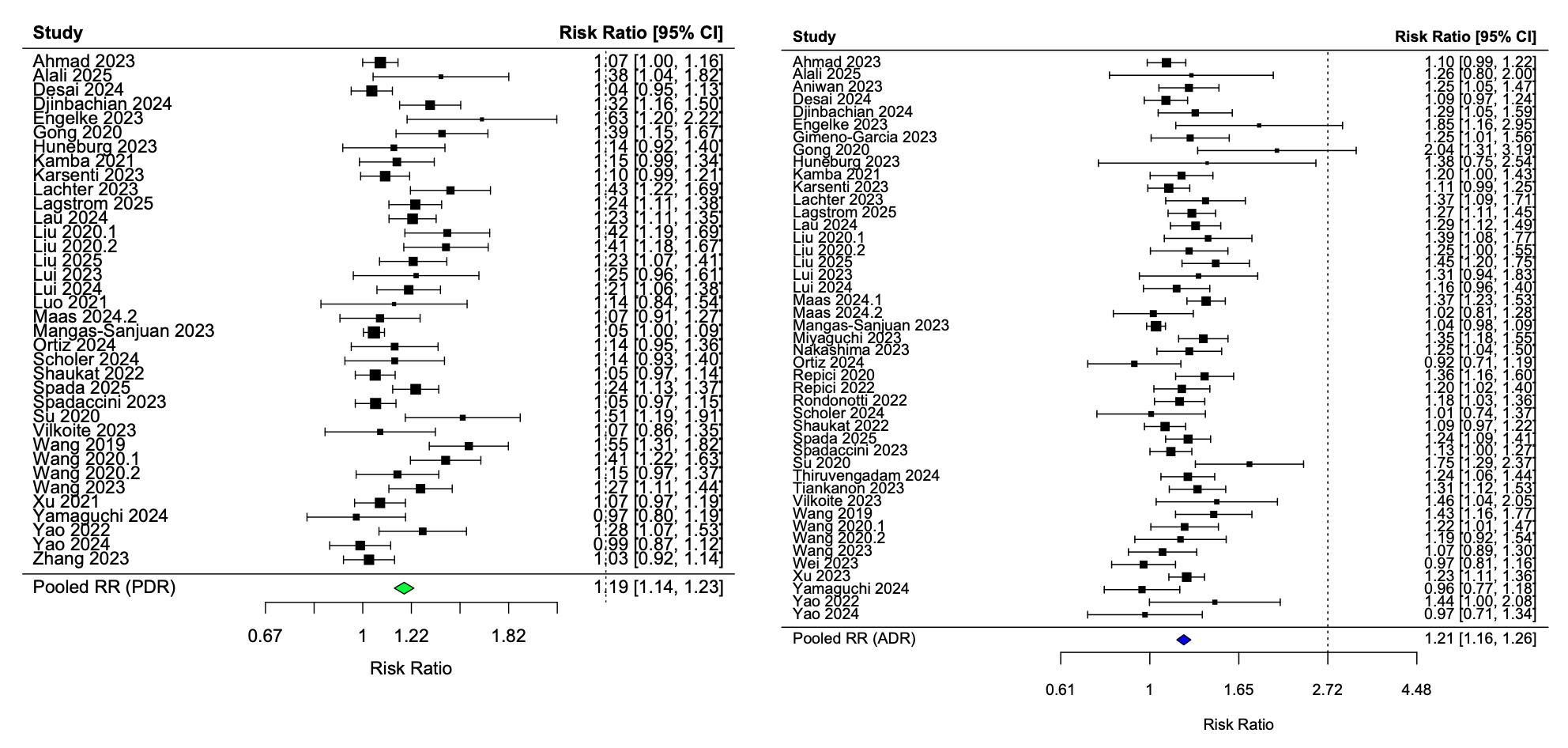
Figure: Figure 1: Risk ratio (RR) forest plots comparing ADR and PDR in colonoscopy with CADe vs colonoscopy without CADe
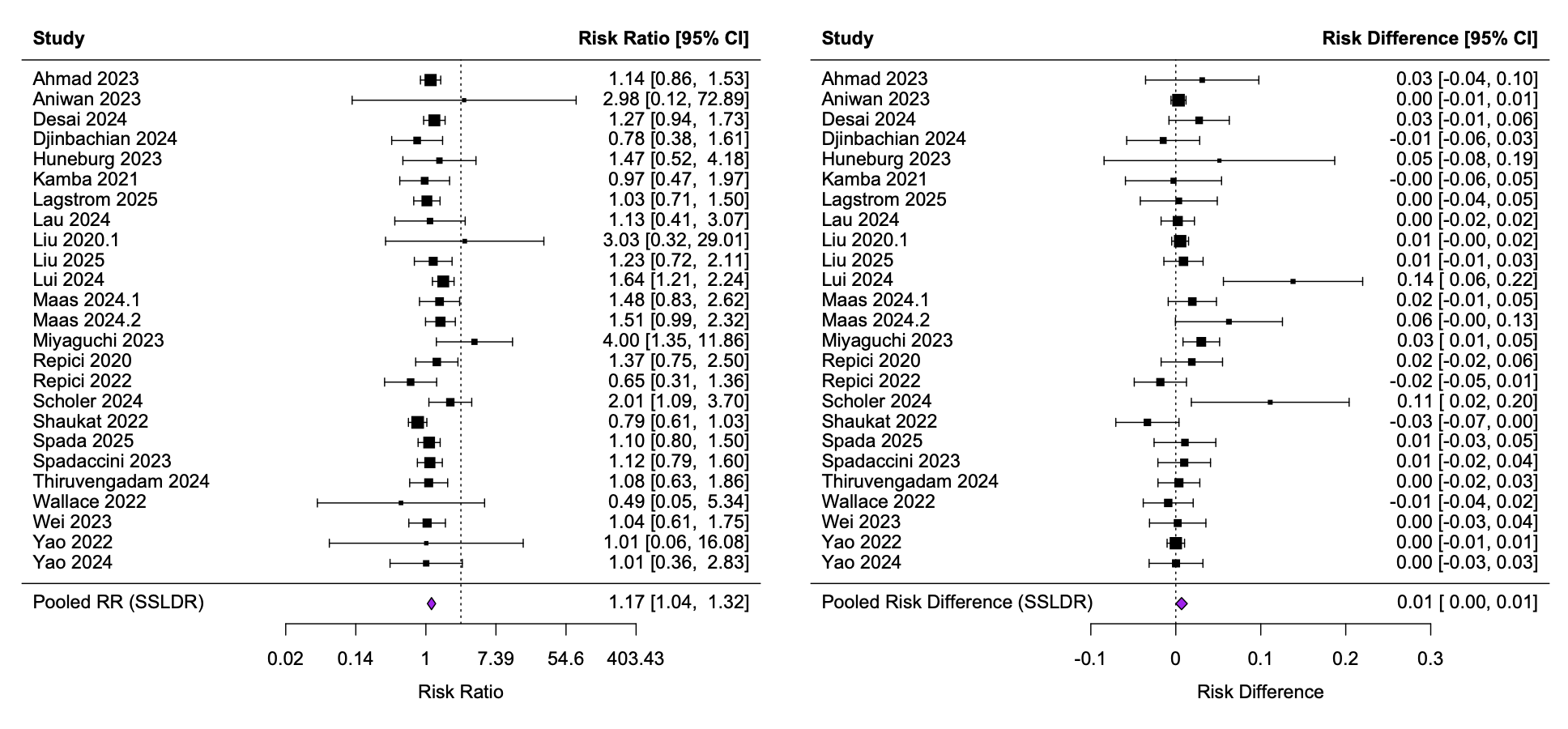
Figure: Figure 2: Risk ratio (RR) and risk difference (RD) forest plots comparing SSLDR in colonoscopy with CADe vs colonoscopy without CADe
Disclosures:
Tasnim Ahmed indicated no relevant financial relationships.
Faisal Ali indicated no relevant financial relationships.
Rachel Hicklen indicated no relevant financial relationships.
Tyler Berzin: Boston Scientific – Consultant. Medtronic – Consultant. Wision AI – Consultant.
Tasnim Ahmed, MD1, Faisal S. Ali, MD1, Rachel Hicklen, MS2, Tyler M. Berzin, MD1. P0857 - Re-Examining Computer-Aided Polyp Detection in the Era of a New Quality Benchmark: A Meta-Analysis of ADR, PDR, and SSLDR, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Beth Israel Deaconess Medical Center, Boston, MA; 2University of Texas MD Anderson Cancer Center, Houston, TX
Introduction: In 2024, the American College of Gastroenterology (ACG) and the American Society for Gastrointestinal Endoscopy (ASGE) updated quality benchmarks for colonoscopy, highlighting adenoma detection rate (ADR) and introducing sessile serrated lesion detection rate (SSLDR) as a new priority quality indicator. While studies have examined the impact of artificial intelligence (AI)-assisted colonoscopy on ADR and polyp detection rate (PDR), no prior meta-analysis has systematically evaluated SSLDR in this context. We conducted a comprehensive meta-analysis of randomized controlled trials (RCTs) published through March 2025 to evaluate the effects of computer-aided detection (CADe) on ADR, PDR, and SSLDR.
Methods: We conducted a systematic review of Ovid Embase and Ovid MEDLINE to identify RCTs that compared AI-assisted colonoscopies with control. Random-effects meta-analyses were performed to compare the effect of computer assisted detection (CADe) on ADR, PDR, and SSLDR in colonoscopies.
Results: A total of 50 systematic reviews were included in our analysis and met inclusion criteria. 45 were used for ADR meta-analysis, 36 for PDR meta-analysis, and 25 for SSLDR meta-analysis. Overall, ADR, PDR, and SSLDR were all significantly higher with CADe than without. ADR was 21% higher in AI-assisted colonoscopies (44.68%) than those without (37.65%) (risk ratio [RR] 1.21, 95% confidence interval [CI] 1.16-1.26 I2 55.66%) (Figure 1). In the studies that included SSLDR data, SSDLDR was also significantly higher in CADe colonoscopies (8.66%) than those without (7.49%) (RR 1.17 95 % CI 1.04-1.32 I2 21.15%) (Figure 2). The risk difference for SSLDR was 0.01 between intervention and control arms (95% CI 0.000-.0135 I2 35.61%) (Figure 2). Finally, PDR, often used as a surrogate marker for ADR in studies, was 19% higher in AI-assisted colonoscopies (56.89%) than control (49.32%) (RR 1.19 95% CI 1.14-1.23 I2 70.64%) (Figure 1).
Discussion: CADe using artificial intelligence improves the quality of colonoscopies, using indicators determined by the newest ACG and AGSE guidelines. While both ADR (performance target > 35%) and SSLDR (performance target > 6%) were improved with CADe, the risk difference in SSLDR was minimal at 0.01. Given the degree of heterogeneity, it is important to standardize methods for future trials and may warrant further subgroup analyses. As CADe systems advance, they should be explicitly trained and validated for SSLDR to support newer colonoscopy quality benchmark expectations.
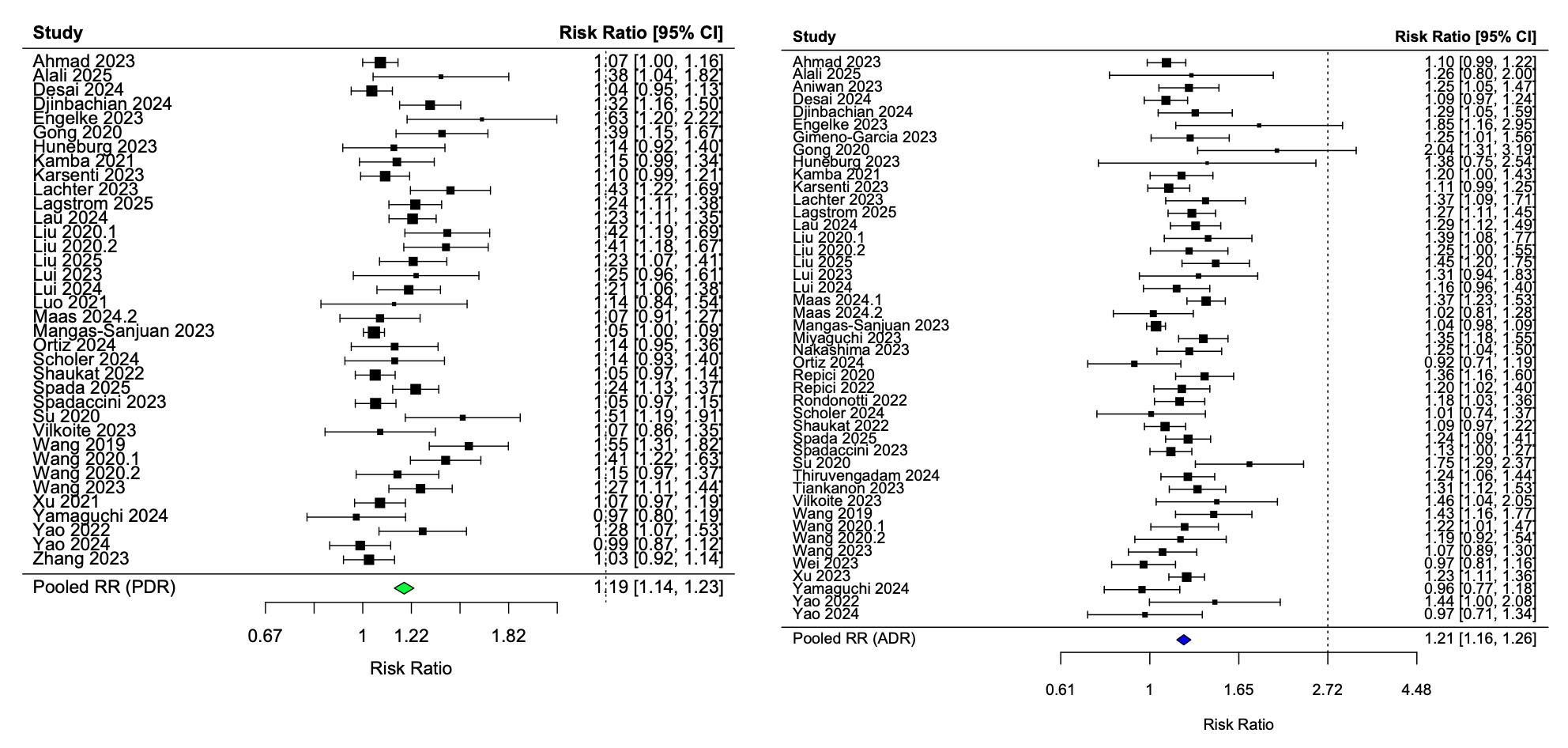
Figure: Figure 1: Risk ratio (RR) forest plots comparing ADR and PDR in colonoscopy with CADe vs colonoscopy without CADe
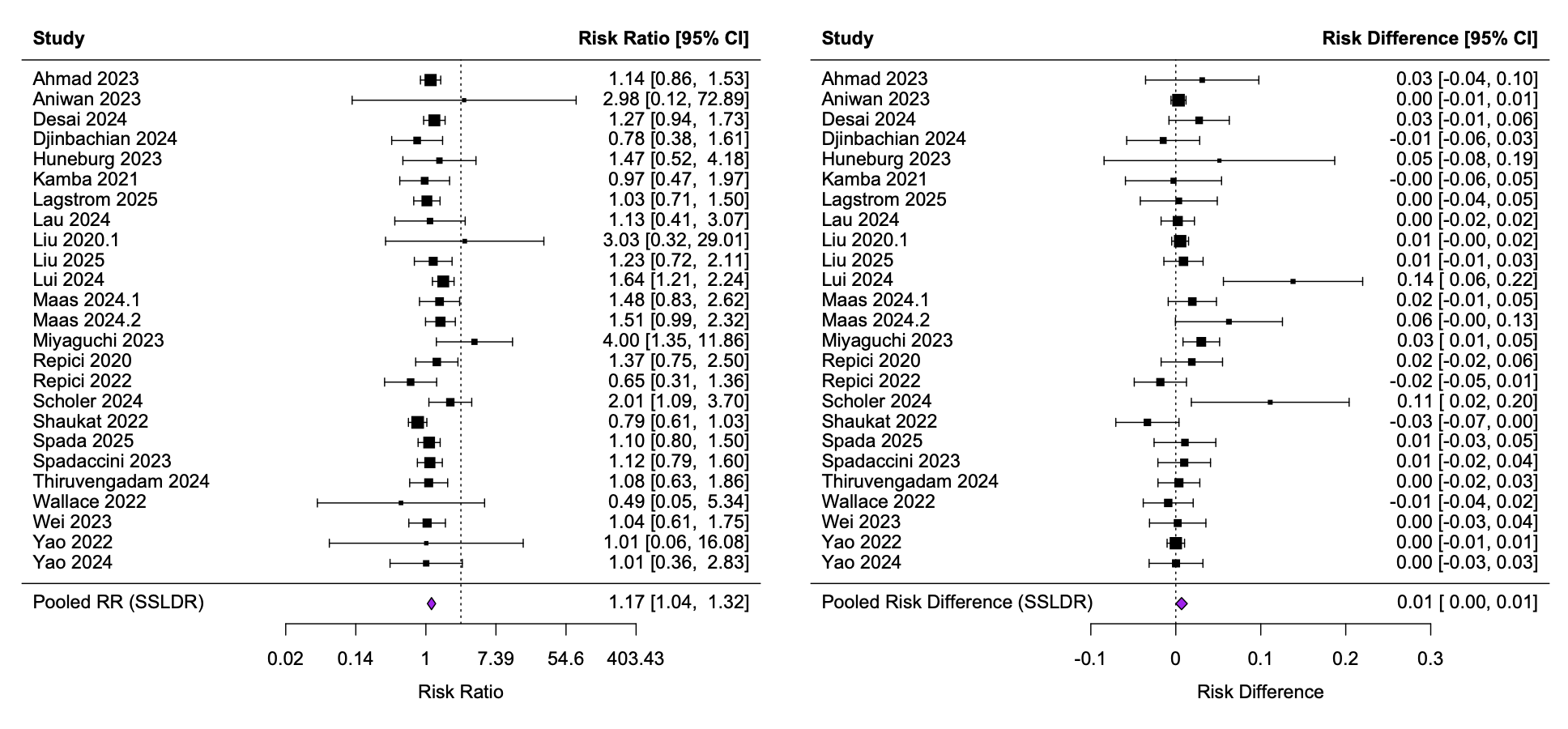
Figure: Figure 2: Risk ratio (RR) and risk difference (RD) forest plots comparing SSLDR in colonoscopy with CADe vs colonoscopy without CADe
Disclosures:
Tasnim Ahmed indicated no relevant financial relationships.
Faisal Ali indicated no relevant financial relationships.
Rachel Hicklen indicated no relevant financial relationships.
Tyler Berzin: Boston Scientific – Consultant. Medtronic – Consultant. Wision AI – Consultant.
Tasnim Ahmed, MD1, Faisal S. Ali, MD1, Rachel Hicklen, MS2, Tyler M. Berzin, MD1. P0857 - Re-Examining Computer-Aided Polyp Detection in the Era of a New Quality Benchmark: A Meta-Analysis of ADR, PDR, and SSLDR, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
