Sunday Poster Session
Category: General Endoscopy
P0856 - Development of Comfort With Independent Endoscopy Following Gastroenterology Fellowship Training
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Benjamin M. Moy, MD
McGaw Medical Center of Northwestern University
Chicago, IL
Presenting Author(s)
Benjamin M. Moy, MD1, Terrance Rodrigues, MD2, Rajesh N. Keswani, MD, MS2, John E. Pandolfino, MD, MSCI2, Ronak V. Patel, MD2
1McGaw Medical Center of Northwestern University, Chicago, IL; 2Feinberg School of Medicine, Northwestern University, Chicago, IL
Introduction: Prior studies have set forth best practices in endoscopy education and assessment tools to ensure proper endoscopic skill acquisition during fellowship. Little is known about transitions to independent practice and readiness for unsupervised endoscopy. We aimed to evaluate factors influencing the development of comfort with independent endoscopy in gastroenterologists following gastroenterology (GI) fellowship.
Methods: Providers who graduated from a single academic-based general GI fellowship program over the past 25 years were invited to complete a 17-question survey exploring their experiences during and after fellowship and comfort with independent procedural skills post-graduation. Descriptive statistics are reported.
Results: Of 72 gastroenterologists invited, 23 (32%) completed the survey. Most (82.6%) had practiced independently for 0-10 years (47.8% 0-5yrs; 34.8% 6-10yrs) and worked at an academic hospital (65.2%). Mean (±SD) time to comfort with independent endoscopy post-fellowship was 1.35 ± 1.36 years. Upon graduating, respondents felt very comfortable (VC)/comfortable (C) performing upper endoscopy (87% VC, 13% C), administering sedation (87% VC, 13% C), performing esophageal band ligation (65% VC, 30% C), and performing colonoscopy (43% VC, 57% C). In contrast, fewer respondents felt very comfortable/comfortable performing esophageal dilation (30% VC, 17% C), PEG placement (17% VC, 43% C), and defect closure (13% VC, 35% C). Exposure to endoscopy curricula (n=15) and simulation (n=16) during training contributed to comfort in 100% and 56.3% of respondents respectively. Procedural volume/repetition, exposure to challenging cases, and a strong training environment were reported as the most important factors influencing perceived comfort. Within the first year post-fellowship, postoperative adverse event management and efficiency were rated as the most challenging aspects while sedation administration and patient communication were the least challenging (Fig 1).
Discussion: In our study, most gastroenterologists were comfortable with independent endoscopy 1-2 years after fellowship. Procedural volume/repetition and exposure to complex cases were highlighted as important factors contributing to comfort. More hands-on training for advanced techniques like defect closure and training for efficiency and management of postoperative adverse events may be needed in fellowship training. Additional studies are needed to better understand and support transitions to independent practice
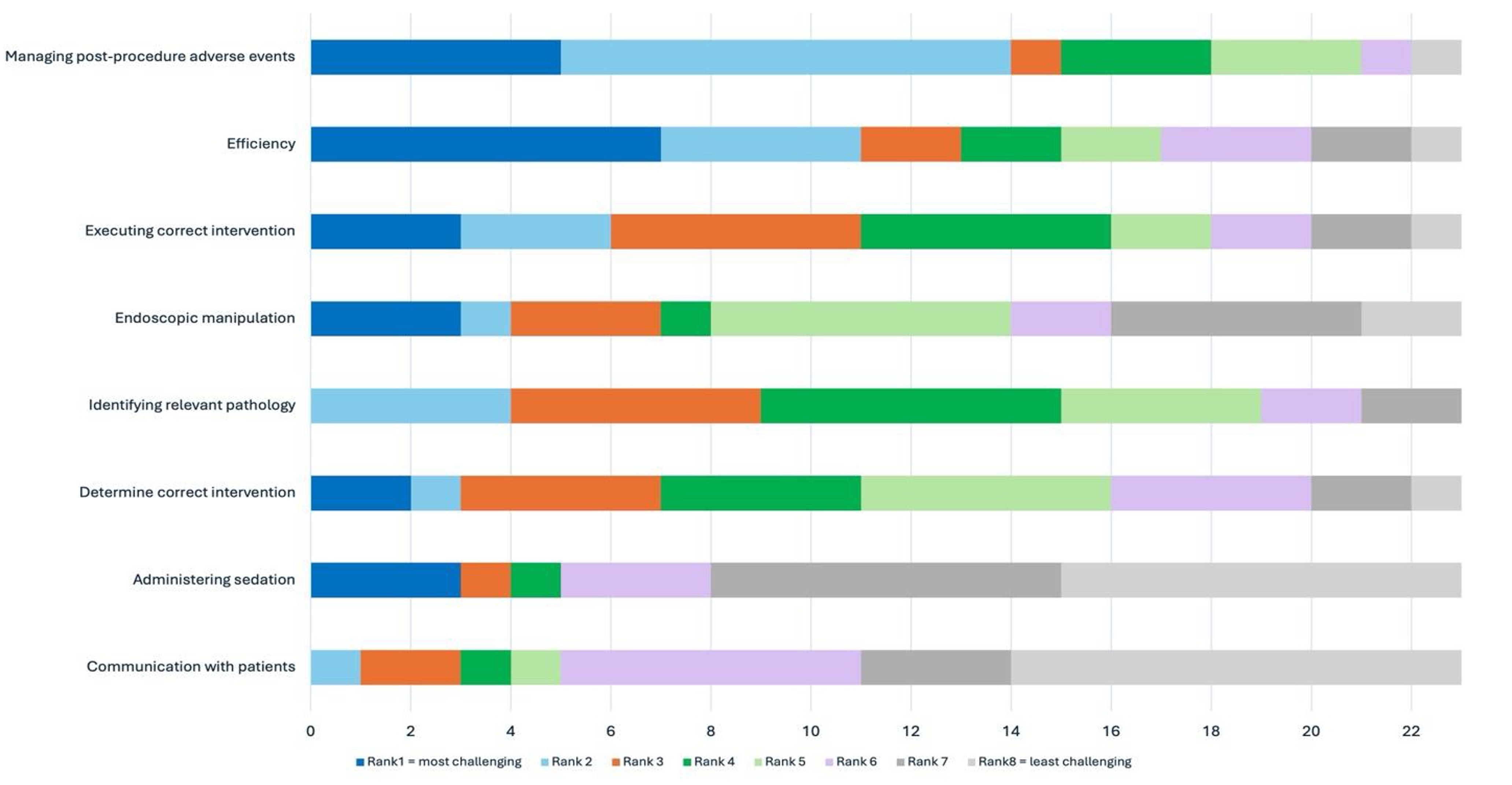
Figure: Figure 1. Ranking of Most Challenging Aspects of Endoscopy during First Year Post-Fellowship
Disclosures:
Benjamin Moy indicated no relevant financial relationships.
Terrance Rodrigues indicated no relevant financial relationships.
Rajesh Keswani: Boston Scientific – Consultant. Cook Medical – Consultant. Medtronic, Inc. – Consultant, Grant/Research Support. Neptune Medical – Consultant. Olympus Corporation – Consultant.
John Pandolfino: Ethicon/J&J – Consultant, Speakers Bureau. Medtronic – Advisor or Review Panel Member, Consultant, Grant/Research Support, Intellectual Property/Patents, Royalties, Speakers Bureau. Phathom – Consultant, Speakers Bureau.
Ronak Patel: Carelon Health – Consultant. CVS Caremark – Consultant. US News and World Report – Consultant.
Benjamin M. Moy, MD1, Terrance Rodrigues, MD2, Rajesh N. Keswani, MD, MS2, John E. Pandolfino, MD, MSCI2, Ronak V. Patel, MD2. P0856 - Development of Comfort With Independent Endoscopy Following Gastroenterology Fellowship Training, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1McGaw Medical Center of Northwestern University, Chicago, IL; 2Feinberg School of Medicine, Northwestern University, Chicago, IL
Introduction: Prior studies have set forth best practices in endoscopy education and assessment tools to ensure proper endoscopic skill acquisition during fellowship. Little is known about transitions to independent practice and readiness for unsupervised endoscopy. We aimed to evaluate factors influencing the development of comfort with independent endoscopy in gastroenterologists following gastroenterology (GI) fellowship.
Methods: Providers who graduated from a single academic-based general GI fellowship program over the past 25 years were invited to complete a 17-question survey exploring their experiences during and after fellowship and comfort with independent procedural skills post-graduation. Descriptive statistics are reported.
Results: Of 72 gastroenterologists invited, 23 (32%) completed the survey. Most (82.6%) had practiced independently for 0-10 years (47.8% 0-5yrs; 34.8% 6-10yrs) and worked at an academic hospital (65.2%). Mean (±SD) time to comfort with independent endoscopy post-fellowship was 1.35 ± 1.36 years. Upon graduating, respondents felt very comfortable (VC)/comfortable (C) performing upper endoscopy (87% VC, 13% C), administering sedation (87% VC, 13% C), performing esophageal band ligation (65% VC, 30% C), and performing colonoscopy (43% VC, 57% C). In contrast, fewer respondents felt very comfortable/comfortable performing esophageal dilation (30% VC, 17% C), PEG placement (17% VC, 43% C), and defect closure (13% VC, 35% C). Exposure to endoscopy curricula (n=15) and simulation (n=16) during training contributed to comfort in 100% and 56.3% of respondents respectively. Procedural volume/repetition, exposure to challenging cases, and a strong training environment were reported as the most important factors influencing perceived comfort. Within the first year post-fellowship, postoperative adverse event management and efficiency were rated as the most challenging aspects while sedation administration and patient communication were the least challenging (Fig 1).
Discussion: In our study, most gastroenterologists were comfortable with independent endoscopy 1-2 years after fellowship. Procedural volume/repetition and exposure to complex cases were highlighted as important factors contributing to comfort. More hands-on training for advanced techniques like defect closure and training for efficiency and management of postoperative adverse events may be needed in fellowship training. Additional studies are needed to better understand and support transitions to independent practice
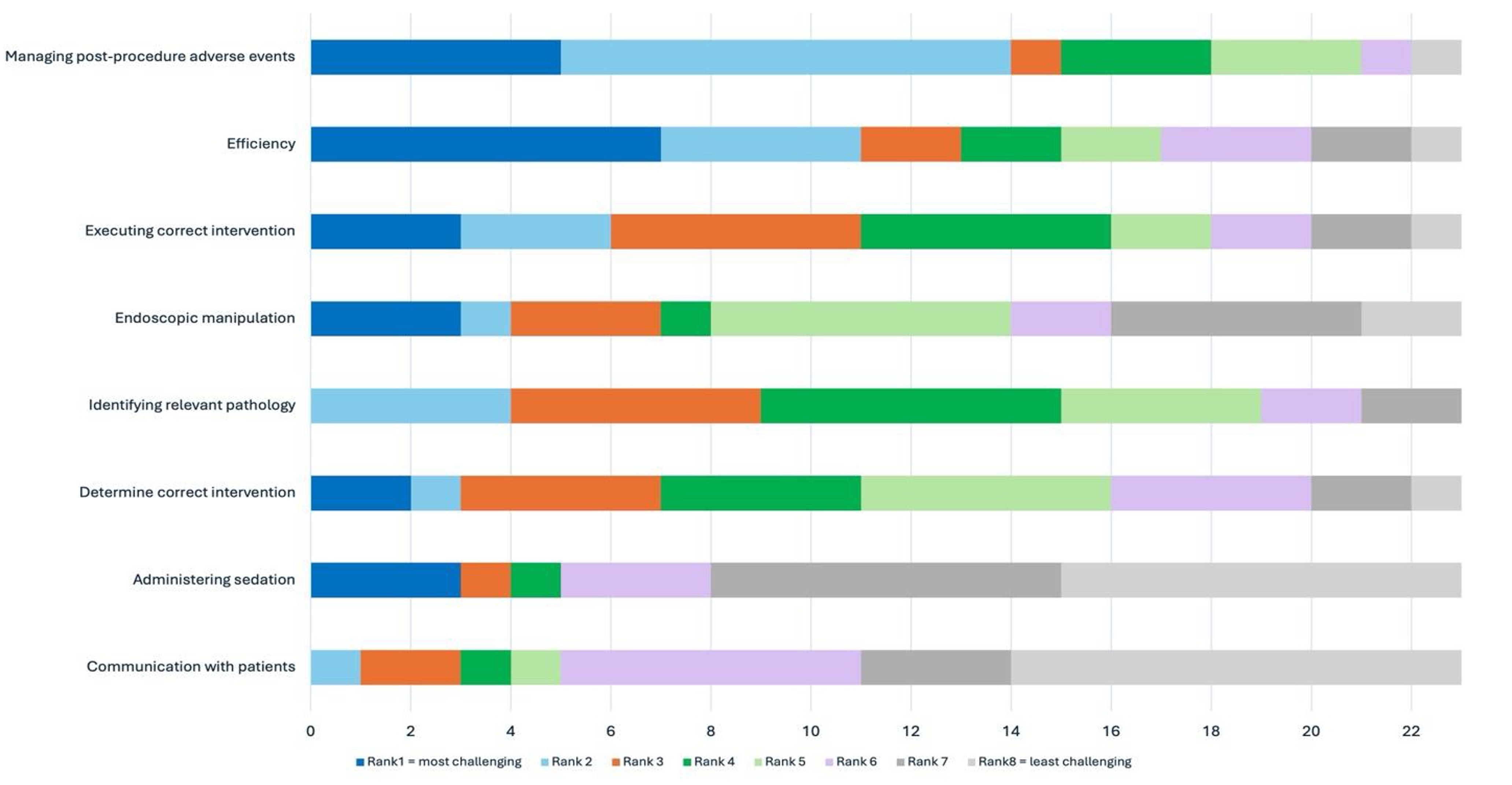
Figure: Figure 1. Ranking of Most Challenging Aspects of Endoscopy during First Year Post-Fellowship
Disclosures:
Benjamin Moy indicated no relevant financial relationships.
Terrance Rodrigues indicated no relevant financial relationships.
Rajesh Keswani: Boston Scientific – Consultant. Cook Medical – Consultant. Medtronic, Inc. – Consultant, Grant/Research Support. Neptune Medical – Consultant. Olympus Corporation – Consultant.
John Pandolfino: Ethicon/J&J – Consultant, Speakers Bureau. Medtronic – Advisor or Review Panel Member, Consultant, Grant/Research Support, Intellectual Property/Patents, Royalties, Speakers Bureau. Phathom – Consultant, Speakers Bureau.
Ronak Patel: Carelon Health – Consultant. CVS Caremark – Consultant. US News and World Report – Consultant.
Benjamin M. Moy, MD1, Terrance Rodrigues, MD2, Rajesh N. Keswani, MD, MS2, John E. Pandolfino, MD, MSCI2, Ronak V. Patel, MD2. P0856 - Development of Comfort With Independent Endoscopy Following Gastroenterology Fellowship Training, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
