Sunday Poster Session
Category: General Endoscopy
P0854 - Is Routine Antibiotic Prophylaxis Necessary in Full-Thickness Endoscopic Suturing? A Retrospective Analysis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Hadi Khaled Abou Zeid, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Hadi Khaled. Abou Zeid, MD1, Yara Salameh, MD1, Moataz Aboeldahb, MBBCh2, Alwatheq Al-Itelat, MD1, Khusboo Gala, MBBS1, Andrew Storm, MD1
1Mayo Clinic, Rochester, MN; 2Mayo Clinic College of Medicine and Science, Rochester, MN
Introduction: Current guidelines recommend against the routine use of prophylactic antibiotics for most endoscopic procedures to minimize antibiotic-related adverse events. However, no recommendations have been made for full-thickness endoscopic suturing procedures, even though such procedures are becoming more common and are used in multiple procedures including endoscopic sleeve gastroplasty (ESG), transoral outlet reduction (TORe), and fistula closure. This study aims to assess the complications associated with antibiotic prophylaxis during endoscopic suturing procedures.
Methods: We conducted a retrospective single-center study of patients who underwent full-thickness endoscopic suturing. Clinical data were extracted and included demographics, comorbidities, procedural details, and post-procedural outcomes. Patients were stratified into two groups based on the use of periprocedural antibiotics. The primary outcome was the rate of infectious complications graded based on the American Society of Gastrointestinal Endoscopy guidelines. Categorical variables were compared using chi-square or Fisher’s exact test, and continuous variables were compared using t-tests or Wilcoxon rank-sum tests. Multivariable logistic regression was performed to assess the association between antibiotic use and complication rates, adjusting for BMI and history of diabetes mellitus.
Results: A total of 100 patients (mean age 55 ± 12, 92% Female) were included (Table 1). Periprocedural antibiotics were administered in 62 (62%) of patients with Levofloxacin in 57 (92%) and Piperacillin-Tazobactam 5 (9%). There was no significant difference in the rate of infectious complications between patients who received periprocedural antibiotics and those who did not (13% vs. 11%, OR= 0.84, p = 0.76). In the no-antibiotic group, complications included 3 (10.5%) mild, 1 (2.6%) moderate, and 1 (2.6%) severe complication. While in the antibiotic group, there was 5 (8.1%) mild and 1 (1.6%) moderate complication. In a multivariate model including BMI and history of diabetes mellitus, antibiotic use was not associated with a statistically significant difference in complication rates (OR: 1.13, 95% CI: 0.27–4.69, p = 0.865).
Discussion: Periprocedural antibiotic use was not associated with a reduction in post-procedural complications in patients undergoing endoscopic suturing. Our findings suggest that routine antibiotic prophylaxis may be unnecessary in low-risk cases, warranting further prospective evaluation to improve procedural outcomes.
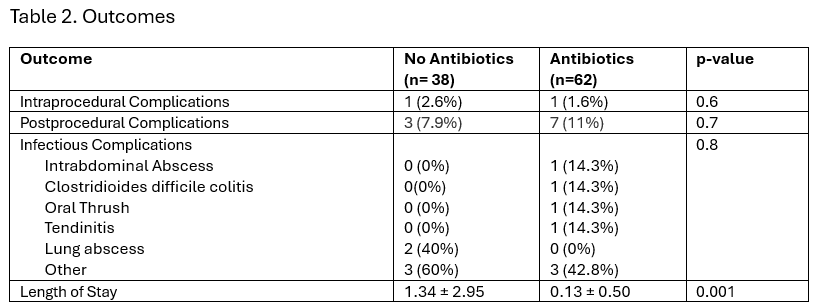
Figure: Table 1. Patient Characteristics
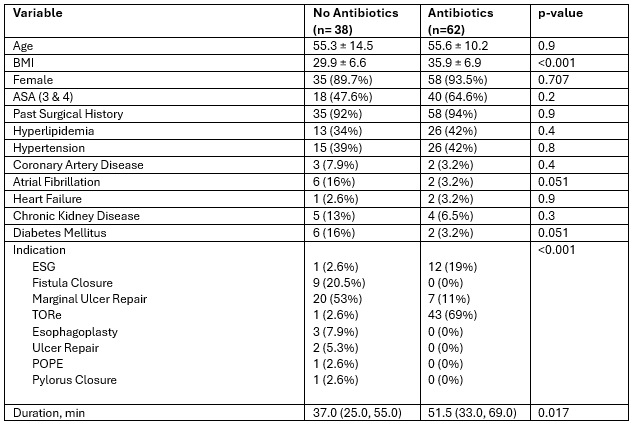
Figure: Table 2. Outcomes
Disclosures:
Hadi Abou Zeid indicated no relevant financial relationships.
Yara Salameh indicated no relevant financial relationships.
Moataz Aboeldahb indicated no relevant financial relationships.
Alwatheq Al-Itelat indicated no relevant financial relationships.
Khusboo Gala indicated no relevant financial relationships.
Andrew Storm: Ambu – Consultant. Apollo Endosurgery – Consultant, Grant/Research Support. Boston Scientific – Consultant, Grant/Research Support. Cook – Consultant. Endogenex – Grant/Research Support. Endo-Tagss – Grant/Research Support. Enterasense – Grant/Research Support. Envision Endoscopy – Grant/Research Support. Intuitive – Consultant. Medtronic – Consultant. MGI Medical – Grant/Research Support. Microtech – Consultant. Olympus – Consultant. OnePass – Grant/Research Support. SofTac – Grant/Research Support. Sotelix – Consultant. Steris – Consultant.
Hadi Khaled. Abou Zeid, MD1, Yara Salameh, MD1, Moataz Aboeldahb, MBBCh2, Alwatheq Al-Itelat, MD1, Khusboo Gala, MBBS1, Andrew Storm, MD1. P0854 - Is Routine Antibiotic Prophylaxis Necessary in Full-Thickness Endoscopic Suturing? A Retrospective Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2Mayo Clinic College of Medicine and Science, Rochester, MN
Introduction: Current guidelines recommend against the routine use of prophylactic antibiotics for most endoscopic procedures to minimize antibiotic-related adverse events. However, no recommendations have been made for full-thickness endoscopic suturing procedures, even though such procedures are becoming more common and are used in multiple procedures including endoscopic sleeve gastroplasty (ESG), transoral outlet reduction (TORe), and fistula closure. This study aims to assess the complications associated with antibiotic prophylaxis during endoscopic suturing procedures.
Methods: We conducted a retrospective single-center study of patients who underwent full-thickness endoscopic suturing. Clinical data were extracted and included demographics, comorbidities, procedural details, and post-procedural outcomes. Patients were stratified into two groups based on the use of periprocedural antibiotics. The primary outcome was the rate of infectious complications graded based on the American Society of Gastrointestinal Endoscopy guidelines. Categorical variables were compared using chi-square or Fisher’s exact test, and continuous variables were compared using t-tests or Wilcoxon rank-sum tests. Multivariable logistic regression was performed to assess the association between antibiotic use and complication rates, adjusting for BMI and history of diabetes mellitus.
Results: A total of 100 patients (mean age 55 ± 12, 92% Female) were included (Table 1). Periprocedural antibiotics were administered in 62 (62%) of patients with Levofloxacin in 57 (92%) and Piperacillin-Tazobactam 5 (9%). There was no significant difference in the rate of infectious complications between patients who received periprocedural antibiotics and those who did not (13% vs. 11%, OR= 0.84, p = 0.76). In the no-antibiotic group, complications included 3 (10.5%) mild, 1 (2.6%) moderate, and 1 (2.6%) severe complication. While in the antibiotic group, there was 5 (8.1%) mild and 1 (1.6%) moderate complication. In a multivariate model including BMI and history of diabetes mellitus, antibiotic use was not associated with a statistically significant difference in complication rates (OR: 1.13, 95% CI: 0.27–4.69, p = 0.865).
Discussion: Periprocedural antibiotic use was not associated with a reduction in post-procedural complications in patients undergoing endoscopic suturing. Our findings suggest that routine antibiotic prophylaxis may be unnecessary in low-risk cases, warranting further prospective evaluation to improve procedural outcomes.
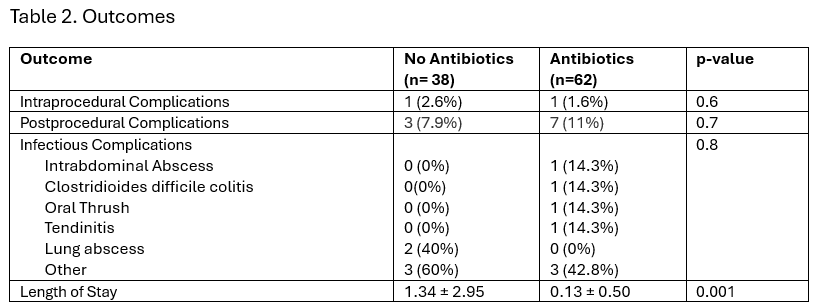
Figure: Table 1. Patient Characteristics
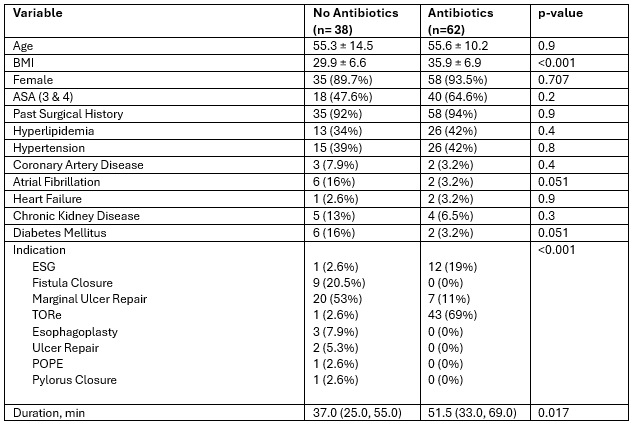
Figure: Table 2. Outcomes
Disclosures:
Hadi Abou Zeid indicated no relevant financial relationships.
Yara Salameh indicated no relevant financial relationships.
Moataz Aboeldahb indicated no relevant financial relationships.
Alwatheq Al-Itelat indicated no relevant financial relationships.
Khusboo Gala indicated no relevant financial relationships.
Andrew Storm: Ambu – Consultant. Apollo Endosurgery – Consultant, Grant/Research Support. Boston Scientific – Consultant, Grant/Research Support. Cook – Consultant. Endogenex – Grant/Research Support. Endo-Tagss – Grant/Research Support. Enterasense – Grant/Research Support. Envision Endoscopy – Grant/Research Support. Intuitive – Consultant. Medtronic – Consultant. MGI Medical – Grant/Research Support. Microtech – Consultant. Olympus – Consultant. OnePass – Grant/Research Support. SofTac – Grant/Research Support. Sotelix – Consultant. Steris – Consultant.
Hadi Khaled. Abou Zeid, MD1, Yara Salameh, MD1, Moataz Aboeldahb, MBBCh2, Alwatheq Al-Itelat, MD1, Khusboo Gala, MBBS1, Andrew Storm, MD1. P0854 - Is Routine Antibiotic Prophylaxis Necessary in Full-Thickness Endoscopic Suturing? A Retrospective Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
