Sunday Poster Session
Category: Functional Bowel Disease
P0827 - Mast Cell Activation Syndrome: An Entity Overlapping With Irritable Bowel Syndrome and Often Ignored
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
Theja V. Channapragada, DO, MBA, MS (he/him/his)
Penn State Health Milton S. Hershey Medical Center
Hershey, PA
Presenting Author(s)
Theja V. Channapragada, DO, MBA, MS1, Maryanna Schweininger, DO2, Michael Gistrak, MD3, Scott Merlin, MD3, Srinivas Channapragada, MD4, C.S. Pitchumoni, MD, MACG, MPH4
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2Cooper University Hospital, Camden, NJ; 3Robert Wood Johnson University Hospital Rahway, Rahway, NJ; 4Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Mast Cell Activation Syndrome (MCAS) displays diverse inflammatory and allergic symptoms across multiple body systems. Symptoms affecting the gastrointestinal (GI) tract include dyspepsia, gastroesophageal reflux, abdominal pain, nausea, vomiting, diarrhea, constipation, gastroparesis, angioedema, dysphagia (usually proximal), bloating (post-prandial or spontaneous), and malabsorption. Patients with MCAS exhibit a range of symptoms, including Irritable Bowel Syndrome (IBS)-like symptoms, various dysautonomia types, neuropathy, myalgia, migraine, headache, cognitive dysfunction, restless legs syndrome, sleep disturbances, non-pulsatile tinnitus, depression, anxiety, and panic attacks. The general population is estimated to have a 17% prevalence. In gastroenterology, MCAS is prevalent yet frequently excluded from diagnostic considerations. Misinterpretations of non-GI symptoms as IBS are common due to the past overemphasis on IBS as a psychosomatic illness. Medical school curricula typically exclude MCAS. Due to unsatisfactory medical experiences, individuals with MCAS may consult many specialists but eventually stop reporting their symptoms. This office-based case series highlights the importance of differentiating MCAS and IBS patients.
Case Description/
Methods: Please refer to Table 1 and Figure 1.
Discussion: Patients previously diagnosed with IBS received a MCAS diagnosis based on complex histories, multi-organ symptoms, non-bloody diarrhea (no alarm symptoms), negative endoscopies, and GI tract biopsies revealing mast cell hyperplasia via special staining. The patients' response to H1/H2 antagonists supported our MCAS diagnosis. This case series highlights that MCAS may be overlooked due to a limited understanding of GI symptom prevalence and characteristics. MCAS is neglected due to IBS's high prevalence (up to 40% in healthy individuals), overlapping symptoms with IBS, and overall unfamiliarity within the medical community. We propose that MCAS should be evaluated in patients with IBS symptoms, testing for elevated serum tryptase can aid in diagnosing the active stage, gastrointestinal mucosal biopsies with specialized staining for mast cells should be conducted in all suspected cases, the effectiveness of antihistamines and H2 receptor antagonists should be assessed in a therapeutic trial involving suspected cases.
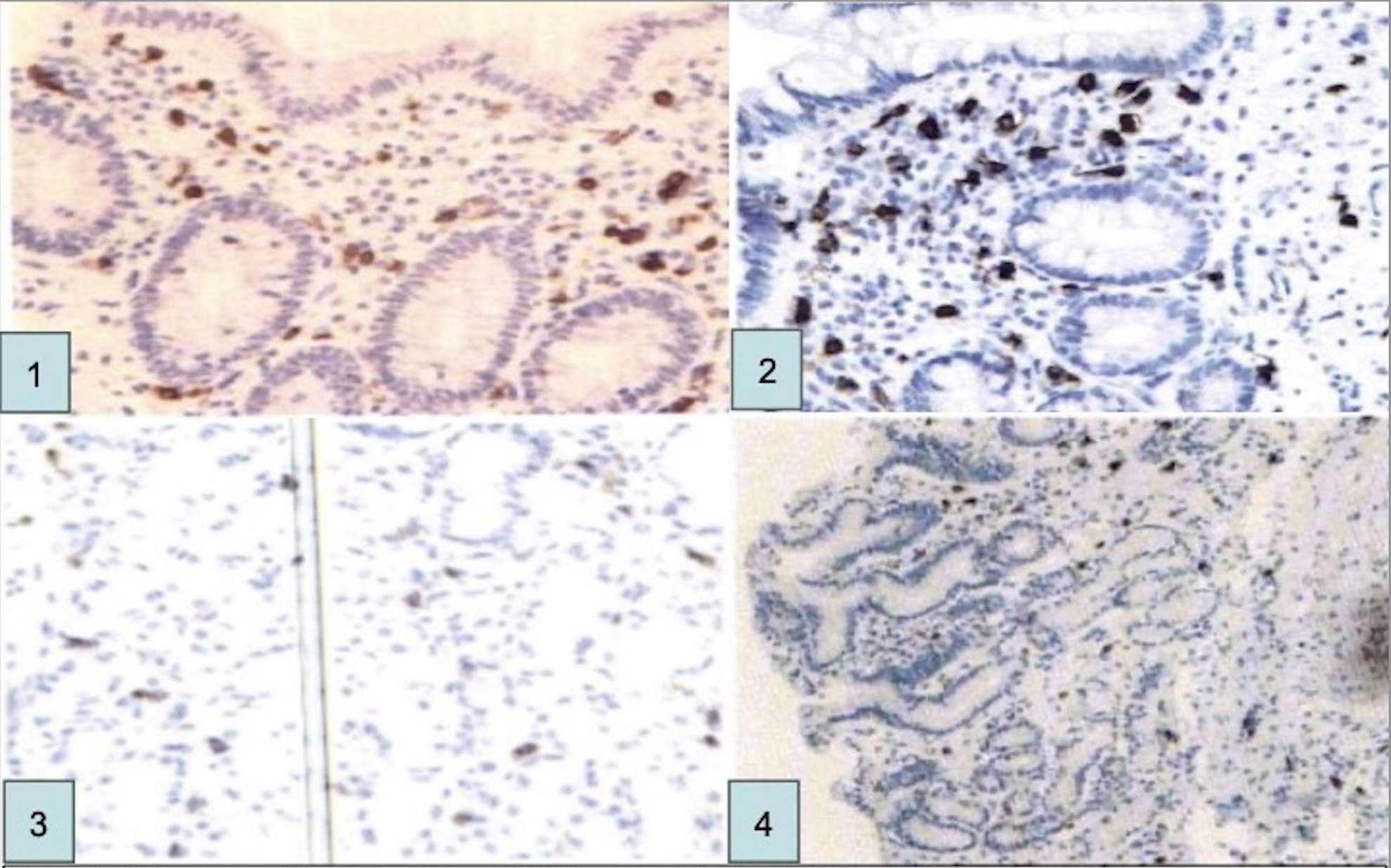
Figure: Figure 1: Biopsy results of patients who underwent colonoscopy and/or esophagogastroduodenoscopy(EGD). Immunohistochemical staining (CD117) revealed a range of 20–60 mast cells per high-power field. Note: Follow-up biopsies to confirm histological response were not performed. Case 1: Colonoscopy-Transverse Colon, CD117 Stain, 53 Mast Cells per High Powered Field. Case 2: Colonoscopy-Transverse Colon, CD117 Stain, 60 Mast Cells per High Powered Field. Case 3: Esophagogastroduodenoscopy- Stomach Body, CD117 Stain, 20 Mast Cells per High Powered Field. Case 4: Esophagogastroduodenoscopy- Stomach Body, CD117 Stain, 31 Mast Cells per High Powered Field

Figure: Table 1: Summary of clinical presentation, procedural and histologic findings, and treatment response in four patients with suspected MCAS. All patients had chronic gastrointestinal (GI) symptoms lasting more than 6 months, systemic symptoms in 2 or more organ systems, and responded to H1/H2 receptor antagonists. Note: Serum tryptase levels were not obtained during symptomatic episodes in this case series, which limited the assessment of mast cell activation by laboratory criteria. Abbreviations: CBC-Complete Blood Count, GAD-Generalized Anxiety Disorder, Hpf-High Powered Field, IBS-Irritable Bowel Syndrome, MC-Mast Cell
Disclosures:
Theja Channapragada indicated no relevant financial relationships.
Maryanna Schweininger indicated no relevant financial relationships.
Michael Gistrak indicated no relevant financial relationships.
Scott Merlin indicated no relevant financial relationships.
Srinivas Channapragada indicated no relevant financial relationships.
C.S. Pitchumoni indicated no relevant financial relationships.
Theja V. Channapragada, DO, MBA, MS1, Maryanna Schweininger, DO2, Michael Gistrak, MD3, Scott Merlin, MD3, Srinivas Channapragada, MD4, C.S. Pitchumoni, MD, MACG, MPH4. P0827 - Mast Cell Activation Syndrome: An Entity Overlapping With Irritable Bowel Syndrome and Often Ignored, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2Cooper University Hospital, Camden, NJ; 3Robert Wood Johnson University Hospital Rahway, Rahway, NJ; 4Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ
Introduction: Mast Cell Activation Syndrome (MCAS) displays diverse inflammatory and allergic symptoms across multiple body systems. Symptoms affecting the gastrointestinal (GI) tract include dyspepsia, gastroesophageal reflux, abdominal pain, nausea, vomiting, diarrhea, constipation, gastroparesis, angioedema, dysphagia (usually proximal), bloating (post-prandial or spontaneous), and malabsorption. Patients with MCAS exhibit a range of symptoms, including Irritable Bowel Syndrome (IBS)-like symptoms, various dysautonomia types, neuropathy, myalgia, migraine, headache, cognitive dysfunction, restless legs syndrome, sleep disturbances, non-pulsatile tinnitus, depression, anxiety, and panic attacks. The general population is estimated to have a 17% prevalence. In gastroenterology, MCAS is prevalent yet frequently excluded from diagnostic considerations. Misinterpretations of non-GI symptoms as IBS are common due to the past overemphasis on IBS as a psychosomatic illness. Medical school curricula typically exclude MCAS. Due to unsatisfactory medical experiences, individuals with MCAS may consult many specialists but eventually stop reporting their symptoms. This office-based case series highlights the importance of differentiating MCAS and IBS patients.
Case Description/
Methods: Please refer to Table 1 and Figure 1.
Discussion: Patients previously diagnosed with IBS received a MCAS diagnosis based on complex histories, multi-organ symptoms, non-bloody diarrhea (no alarm symptoms), negative endoscopies, and GI tract biopsies revealing mast cell hyperplasia via special staining. The patients' response to H1/H2 antagonists supported our MCAS diagnosis. This case series highlights that MCAS may be overlooked due to a limited understanding of GI symptom prevalence and characteristics. MCAS is neglected due to IBS's high prevalence (up to 40% in healthy individuals), overlapping symptoms with IBS, and overall unfamiliarity within the medical community. We propose that MCAS should be evaluated in patients with IBS symptoms, testing for elevated serum tryptase can aid in diagnosing the active stage, gastrointestinal mucosal biopsies with specialized staining for mast cells should be conducted in all suspected cases, the effectiveness of antihistamines and H2 receptor antagonists should be assessed in a therapeutic trial involving suspected cases.
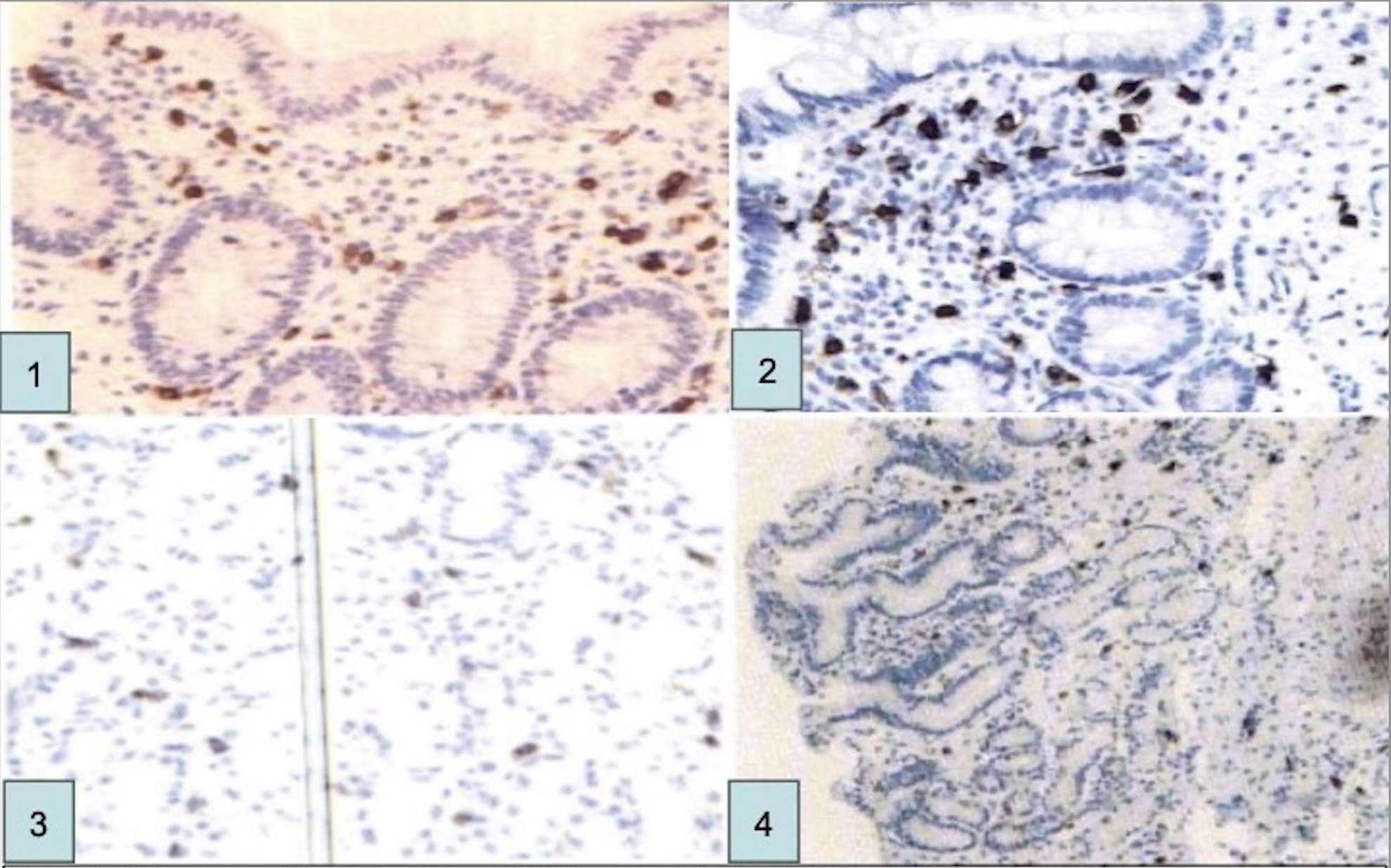
Figure: Figure 1: Biopsy results of patients who underwent colonoscopy and/or esophagogastroduodenoscopy(EGD). Immunohistochemical staining (CD117) revealed a range of 20–60 mast cells per high-power field. Note: Follow-up biopsies to confirm histological response were not performed. Case 1: Colonoscopy-Transverse Colon, CD117 Stain, 53 Mast Cells per High Powered Field. Case 2: Colonoscopy-Transverse Colon, CD117 Stain, 60 Mast Cells per High Powered Field. Case 3: Esophagogastroduodenoscopy- Stomach Body, CD117 Stain, 20 Mast Cells per High Powered Field. Case 4: Esophagogastroduodenoscopy- Stomach Body, CD117 Stain, 31 Mast Cells per High Powered Field

Figure: Table 1: Summary of clinical presentation, procedural and histologic findings, and treatment response in four patients with suspected MCAS. All patients had chronic gastrointestinal (GI) symptoms lasting more than 6 months, systemic symptoms in 2 or more organ systems, and responded to H1/H2 receptor antagonists. Note: Serum tryptase levels were not obtained during symptomatic episodes in this case series, which limited the assessment of mast cell activation by laboratory criteria. Abbreviations: CBC-Complete Blood Count, GAD-Generalized Anxiety Disorder, Hpf-High Powered Field, IBS-Irritable Bowel Syndrome, MC-Mast Cell
Disclosures:
Theja Channapragada indicated no relevant financial relationships.
Maryanna Schweininger indicated no relevant financial relationships.
Michael Gistrak indicated no relevant financial relationships.
Scott Merlin indicated no relevant financial relationships.
Srinivas Channapragada indicated no relevant financial relationships.
C.S. Pitchumoni indicated no relevant financial relationships.
Theja V. Channapragada, DO, MBA, MS1, Maryanna Schweininger, DO2, Michael Gistrak, MD3, Scott Merlin, MD3, Srinivas Channapragada, MD4, C.S. Pitchumoni, MD, MACG, MPH4. P0827 - Mast Cell Activation Syndrome: An Entity Overlapping With Irritable Bowel Syndrome and Often Ignored, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
