Sunday Poster Session
Category: Functional Bowel Disease
P0796 - Beyond Biofeedback: Expanding Perspectives on Pelvic Floor Physical Therapy for Evacuation Disorders
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Mira Yang, MD (she/her/hers)
Tufts Medical Center
Boston, MA
Presenting Author(s)
Mira Yang, MD1, Cayla Bales, MD2, Felipe Carvao, MD2, Jenna Iberle, PT, DPT, WCS3, Joy Liu, MD2
1Tufts Medical Center, Boston, MA; 2Feinberg School of Medicine, Northwestern University, Chicago, IL; 3Northwestern Medicine, Chicago, IL
Introduction: Pelvic floor physical therapy (PFPT) addresses coordination, strength and relaxation of the pelvic floor with potential to treat conditions including fecal incontinence and constipation. Emerging evidence supports PFPT for functional constipation and earlier referral not necessitating laxative failure. Rectal biofeedback is a neuromuscular technique using sensory feedback that is recommended in the treatment of dyssynergia. This study surveyed PFPT providers to describe perspectives and real-world practice patterns on managing evaluation disorders, including the use of biofeedback and other techniques including manual therapy, in the Chicagoland area.
Methods: We surveyed 149 PFPT practices identified through professional directories and word of mouth and contacted via email or phone. There were 48 individual respondents representing 58 practices; reasons for non-response were not recorded. Practice characteristics and treatment tools were aggregated. Select open survey questions were analyzed using thematic analysis.
Results: Most respondents (81%, n = 39) used biofeedback in their practice, most commonly rectal balloon training (54%, n = 26) and EMG-guided (46%, n = 22) (Table 1). Manual techniques, such as visceral mobilization and massage, were the second most common treatment procedure (63%, n = 30), with 27% (n = 13) using tactile biofeedback. Thematic analysis emphasized earlier adoption of PFPT for constipation regardless of dyssynergia, use of manual therapies instead of or to augment biofeedback, and recognition of referral and education gaps impacting access (Table 2). When asked generally about misconceptions, 29% of therapists reported overemphasis on biofeedback by referring providers over manual therapy and education on mechanics of evacuation.
Discussion: Our study describes types of rectal biofeedback provided in one ecological setting (Chicagoland) and physical therapist (PT) perspectives on treating constipation that may differ from recommendations in gastroenterology (GI). GI guidelines cite manometric or EMG-based biofeedback for PFPT, but our findings suggest a significant proportion of PTs may use tactile biofeedback and/or manual therapies, and therefore direct GI-PT communication may be useful for guiding referrals. Our findings suggest that a broader survey may improve management of PFPT referrals and can inform interdisciplinary consensus recommendations for care of patients with constipation.
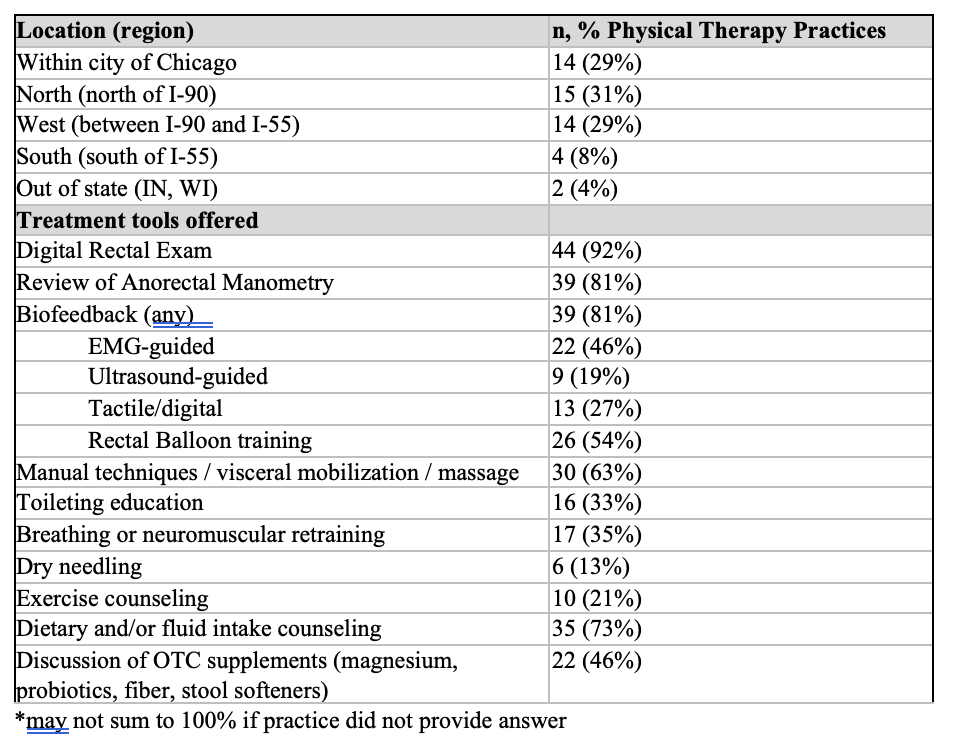
Figure: Table 1. Pelvic floor physical therapist survey responses. Responses displayed as percentage of total practices (n = 48)*

Figure: Table 2. Illustrative data extracts of thematic analysis on referring provider attitudes and patient barriers regarding pelvic floor physical therapy (PT)
Disclosures:
Mira Yang indicated no relevant financial relationships.
Cayla Bales indicated no relevant financial relationships.
Felipe Carvao indicated no relevant financial relationships.
Jenna Iberle indicated no relevant financial relationships.
Joy Liu: Ironwood – Consultant.
Mira Yang, MD1, Cayla Bales, MD2, Felipe Carvao, MD2, Jenna Iberle, PT, DPT, WCS3, Joy Liu, MD2. P0796 - Beyond Biofeedback: Expanding Perspectives on Pelvic Floor Physical Therapy for Evacuation Disorders, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Tufts Medical Center, Boston, MA; 2Feinberg School of Medicine, Northwestern University, Chicago, IL; 3Northwestern Medicine, Chicago, IL
Introduction: Pelvic floor physical therapy (PFPT) addresses coordination, strength and relaxation of the pelvic floor with potential to treat conditions including fecal incontinence and constipation. Emerging evidence supports PFPT for functional constipation and earlier referral not necessitating laxative failure. Rectal biofeedback is a neuromuscular technique using sensory feedback that is recommended in the treatment of dyssynergia. This study surveyed PFPT providers to describe perspectives and real-world practice patterns on managing evaluation disorders, including the use of biofeedback and other techniques including manual therapy, in the Chicagoland area.
Methods: We surveyed 149 PFPT practices identified through professional directories and word of mouth and contacted via email or phone. There were 48 individual respondents representing 58 practices; reasons for non-response were not recorded. Practice characteristics and treatment tools were aggregated. Select open survey questions were analyzed using thematic analysis.
Results: Most respondents (81%, n = 39) used biofeedback in their practice, most commonly rectal balloon training (54%, n = 26) and EMG-guided (46%, n = 22) (Table 1). Manual techniques, such as visceral mobilization and massage, were the second most common treatment procedure (63%, n = 30), with 27% (n = 13) using tactile biofeedback. Thematic analysis emphasized earlier adoption of PFPT for constipation regardless of dyssynergia, use of manual therapies instead of or to augment biofeedback, and recognition of referral and education gaps impacting access (Table 2). When asked generally about misconceptions, 29% of therapists reported overemphasis on biofeedback by referring providers over manual therapy and education on mechanics of evacuation.
Discussion: Our study describes types of rectal biofeedback provided in one ecological setting (Chicagoland) and physical therapist (PT) perspectives on treating constipation that may differ from recommendations in gastroenterology (GI). GI guidelines cite manometric or EMG-based biofeedback for PFPT, but our findings suggest a significant proportion of PTs may use tactile biofeedback and/or manual therapies, and therefore direct GI-PT communication may be useful for guiding referrals. Our findings suggest that a broader survey may improve management of PFPT referrals and can inform interdisciplinary consensus recommendations for care of patients with constipation.
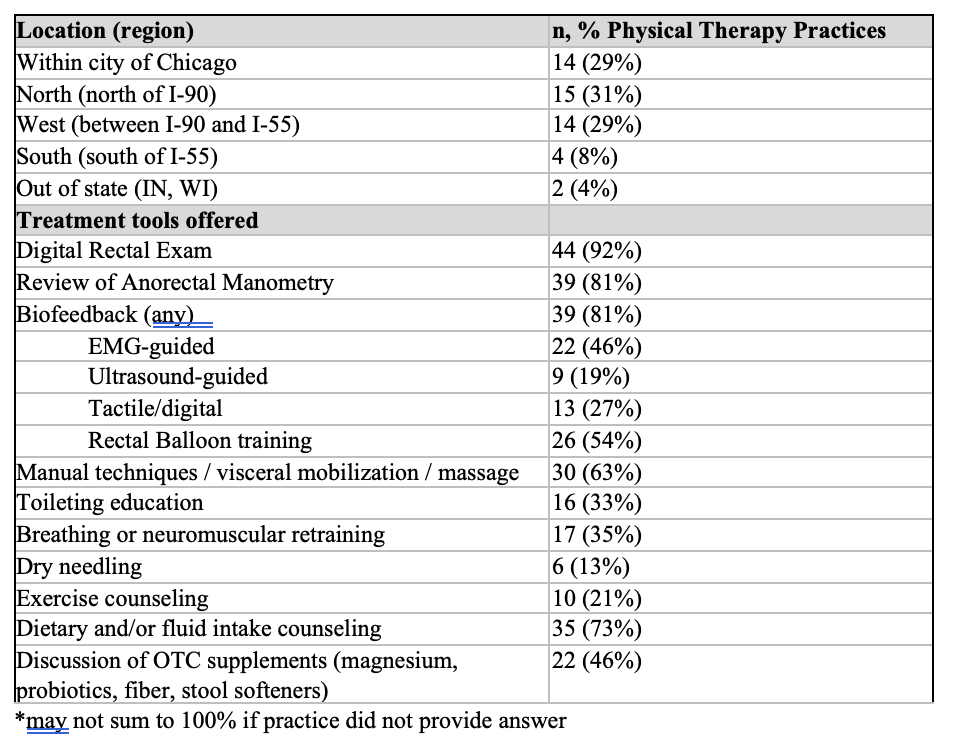
Figure: Table 1. Pelvic floor physical therapist survey responses. Responses displayed as percentage of total practices (n = 48)*

Figure: Table 2. Illustrative data extracts of thematic analysis on referring provider attitudes and patient barriers regarding pelvic floor physical therapy (PT)
Disclosures:
Mira Yang indicated no relevant financial relationships.
Cayla Bales indicated no relevant financial relationships.
Felipe Carvao indicated no relevant financial relationships.
Jenna Iberle indicated no relevant financial relationships.
Joy Liu: Ironwood – Consultant.
Mira Yang, MD1, Cayla Bales, MD2, Felipe Carvao, MD2, Jenna Iberle, PT, DPT, WCS3, Joy Liu, MD2. P0796 - Beyond Biofeedback: Expanding Perspectives on Pelvic Floor Physical Therapy for Evacuation Disorders, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
