Sunday Poster Session
Category: Functional Bowel Disease
P0793 - Association of Metabolic Dysfunction-Associated Steatotic Liver Disease With Lower Gastrointestinal Motility Disorders: A Nationwide Population-Based Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rishi Chowdhary, MD (he/him/his)
Case Western Reserve University / MetroHealth
Cleveland, OH
Presenting Author(s)
Rishi Chowdhary, MD1, Thai Hau Koo, MD2, Rohit Goyal, MD3, Venkata Sunkesula, MD1, Yan Sun, MD1, Gengqing Song, MD4
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 3Louisiana State University, Shreveport, LA; 4Division of Gastroenterology and Hepatology, Metrohealth Medical Center, Cleveland, OH
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) has systemic implications, potentially affecting gastrointestinal (GI) motility. This study aimed to assess the incidence and risk of lower GI motility disorders, specifically functional diarrhea, irritable bowel syndrome (IBS, including diarrhea-predominant [IBS-D], constipation-predominant [IBS-C], and mixed subtype [IBS-mixed]), and constipation, among patients with MASLD compared to matched controls.
Methods: We conducted a retrospective cohort analysis using the TriNetX U.S. Adults (≥18 years) diagnosed with MASLD (ICD-10 codes K76.0 or K75.81) who underwent abdominal imaging were included. Exclusion criteria encompassed conditions that could confound GI outcomes, such as inflammatory bowel disease, colorectal malignancies, prior gastrointestinal surgeries, and other liver diseases. A control cohort without MASLD was propensity score-matched (1:1) based on age, sex, body mass index (BMI), and comorbidities. Outcomes measured over a 5-year follow-up included the incidence of functional diarrhea, IBS (overall and subtypes: IBS-D, IBS-C, and IBS-mixed), and constipation. Statistical analyses included Kaplan-Meier survival analyses and calculations of risk ratios (RR) with 95% confidence intervals (CI).
Results: After matching, each cohort comprised 633,241 patients. Patients with MASLD demonstrated significantly higher risks of developing lower GI motility disorders compared to controls. Specifically, the risk of functional diarrhea was elevated (RR 1.60; 95% CI: 1.43–1.78). The overall risk of IBS was significantly increased (RR 1.62; 95% CI: 1.56–1.68), as were risks for IBS subtypes, including IBS-D (RR 1.82; 95% CI: 1.70–1.95), IBS-C (RR 1.71; 95% CI: 1.54–1.89), and IBS-mixed (RR 1.62; 95% CI: 1.56–1.69). Constipation was also more common in the MASLD cohort (RR 1.39; 95% CI: 1.37–1.42). Kaplan-Meier analyses demonstrated significantly reduced event-free survival probabilities in MASLD patients for all assessed outcomes (log-rank p< 0.001).
Discussion: Patients with MASLD exhibit a significantly increased risk of developing lower GI motility disorders, particularly functional diarrhea, IBS (all subtypes), and constipation. Clinicians should routinely evaluate GI symptoms in patients with MASLD.
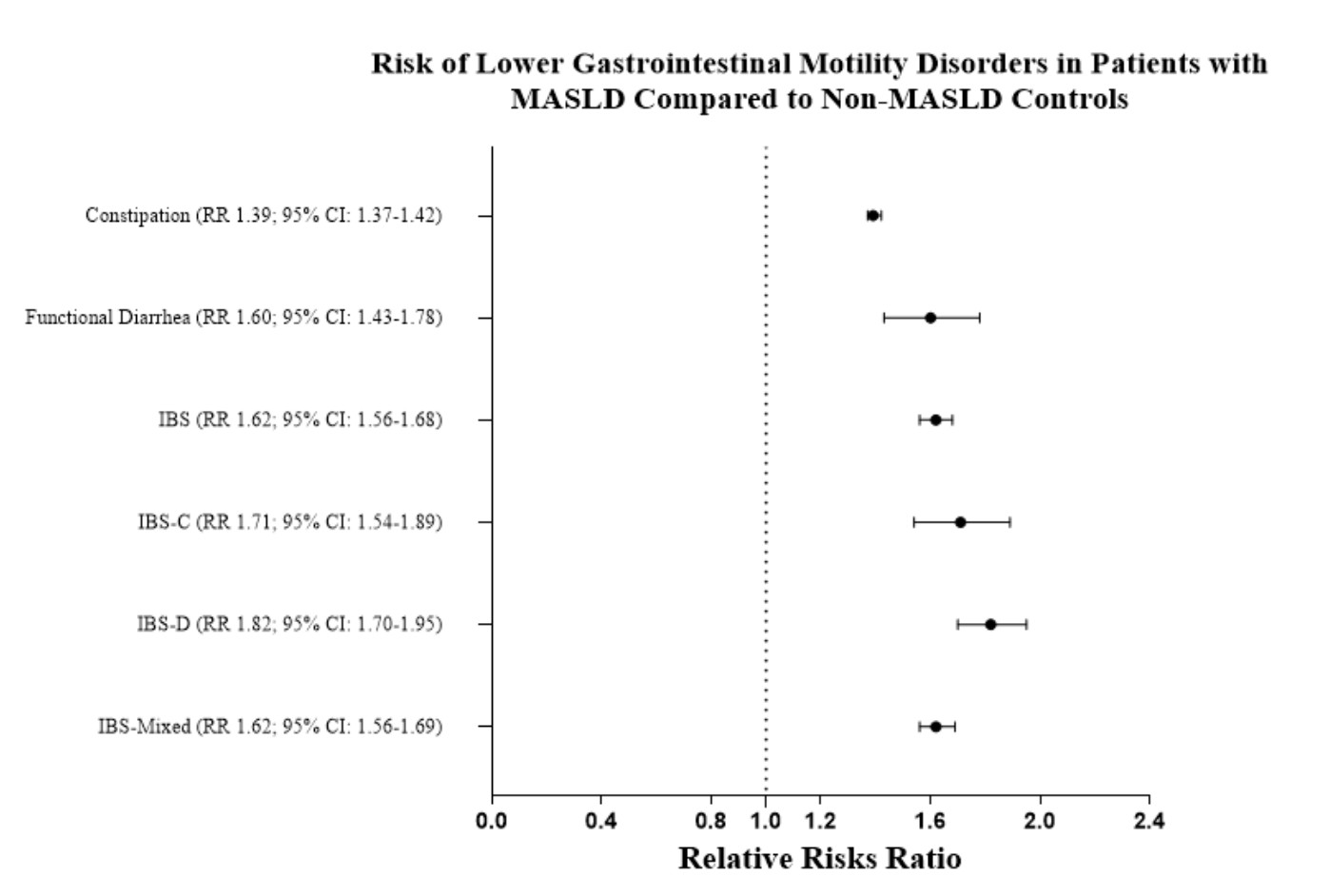
Figure: Forest plot of relative risks (RR) with 95% confidence intervals for lower gastrointestinal motility disorders in MASLD versus non-MASLD patients.
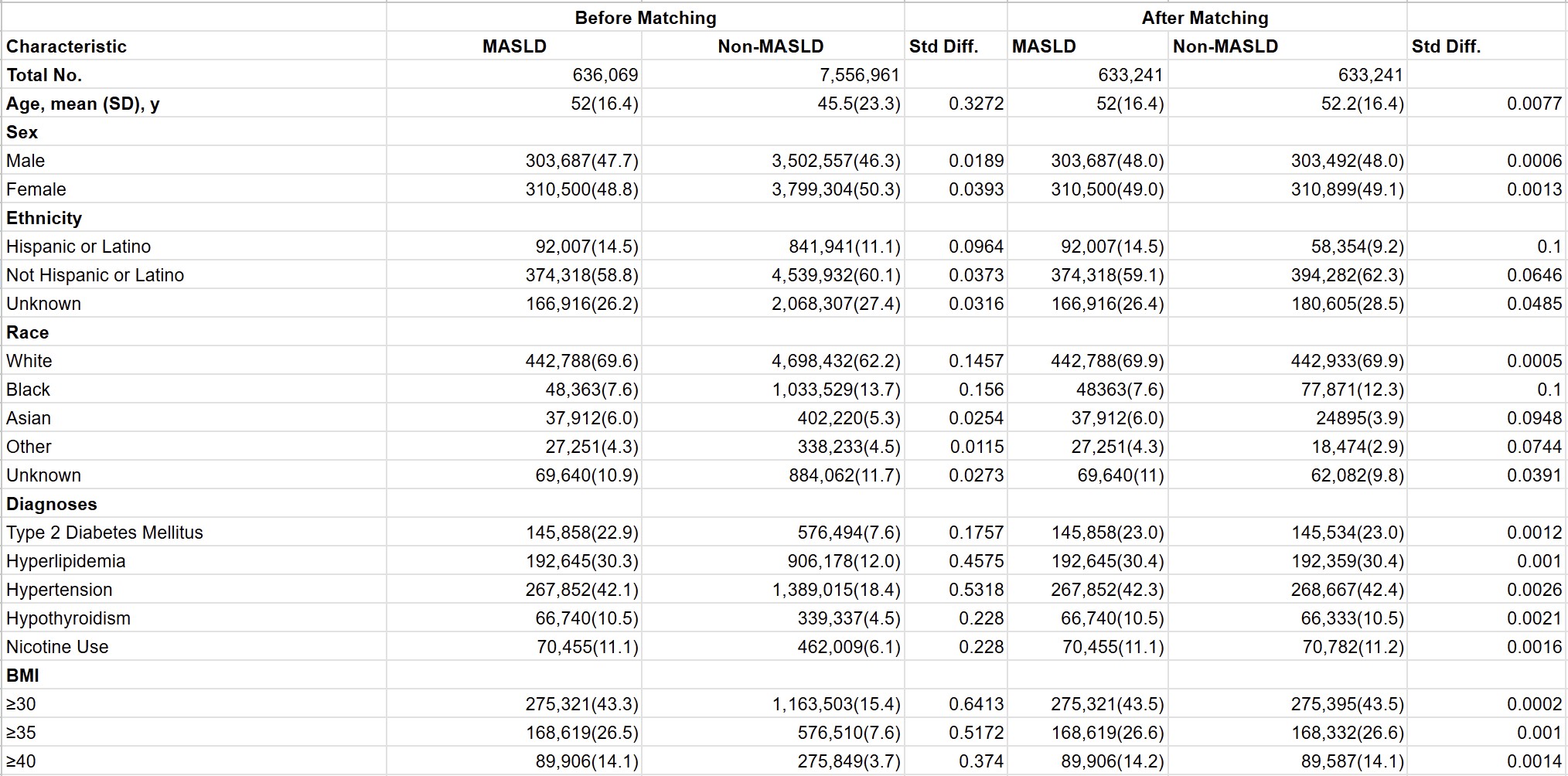
Figure: Baseline Demographics, Comorbidities, and BMI in Patients With and Without MASLD Before and After Propensity Score Matching (MASLD = Metabolic Dysfunction-Associated Steatotic Liver Disease)
Disclosures:
Rishi Chowdhary indicated no relevant financial relationships.
Thai Hau Koo indicated no relevant financial relationships.
Rohit Goyal indicated no relevant financial relationships.
Venkata Sunkesula indicated no relevant financial relationships.
Yan Sun indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Rishi Chowdhary, MD1, Thai Hau Koo, MD2, Rohit Goyal, MD3, Venkata Sunkesula, MD1, Yan Sun, MD1, Gengqing Song, MD4. P0793 - Association of Metabolic Dysfunction-Associated Steatotic Liver Disease With Lower Gastrointestinal Motility Disorders: A Nationwide Population-Based Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 3Louisiana State University, Shreveport, LA; 4Division of Gastroenterology and Hepatology, Metrohealth Medical Center, Cleveland, OH
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) has systemic implications, potentially affecting gastrointestinal (GI) motility. This study aimed to assess the incidence and risk of lower GI motility disorders, specifically functional diarrhea, irritable bowel syndrome (IBS, including diarrhea-predominant [IBS-D], constipation-predominant [IBS-C], and mixed subtype [IBS-mixed]), and constipation, among patients with MASLD compared to matched controls.
Methods: We conducted a retrospective cohort analysis using the TriNetX U.S. Adults (≥18 years) diagnosed with MASLD (ICD-10 codes K76.0 or K75.81) who underwent abdominal imaging were included. Exclusion criteria encompassed conditions that could confound GI outcomes, such as inflammatory bowel disease, colorectal malignancies, prior gastrointestinal surgeries, and other liver diseases. A control cohort without MASLD was propensity score-matched (1:1) based on age, sex, body mass index (BMI), and comorbidities. Outcomes measured over a 5-year follow-up included the incidence of functional diarrhea, IBS (overall and subtypes: IBS-D, IBS-C, and IBS-mixed), and constipation. Statistical analyses included Kaplan-Meier survival analyses and calculations of risk ratios (RR) with 95% confidence intervals (CI).
Results: After matching, each cohort comprised 633,241 patients. Patients with MASLD demonstrated significantly higher risks of developing lower GI motility disorders compared to controls. Specifically, the risk of functional diarrhea was elevated (RR 1.60; 95% CI: 1.43–1.78). The overall risk of IBS was significantly increased (RR 1.62; 95% CI: 1.56–1.68), as were risks for IBS subtypes, including IBS-D (RR 1.82; 95% CI: 1.70–1.95), IBS-C (RR 1.71; 95% CI: 1.54–1.89), and IBS-mixed (RR 1.62; 95% CI: 1.56–1.69). Constipation was also more common in the MASLD cohort (RR 1.39; 95% CI: 1.37–1.42). Kaplan-Meier analyses demonstrated significantly reduced event-free survival probabilities in MASLD patients for all assessed outcomes (log-rank p< 0.001).
Discussion: Patients with MASLD exhibit a significantly increased risk of developing lower GI motility disorders, particularly functional diarrhea, IBS (all subtypes), and constipation. Clinicians should routinely evaluate GI symptoms in patients with MASLD.
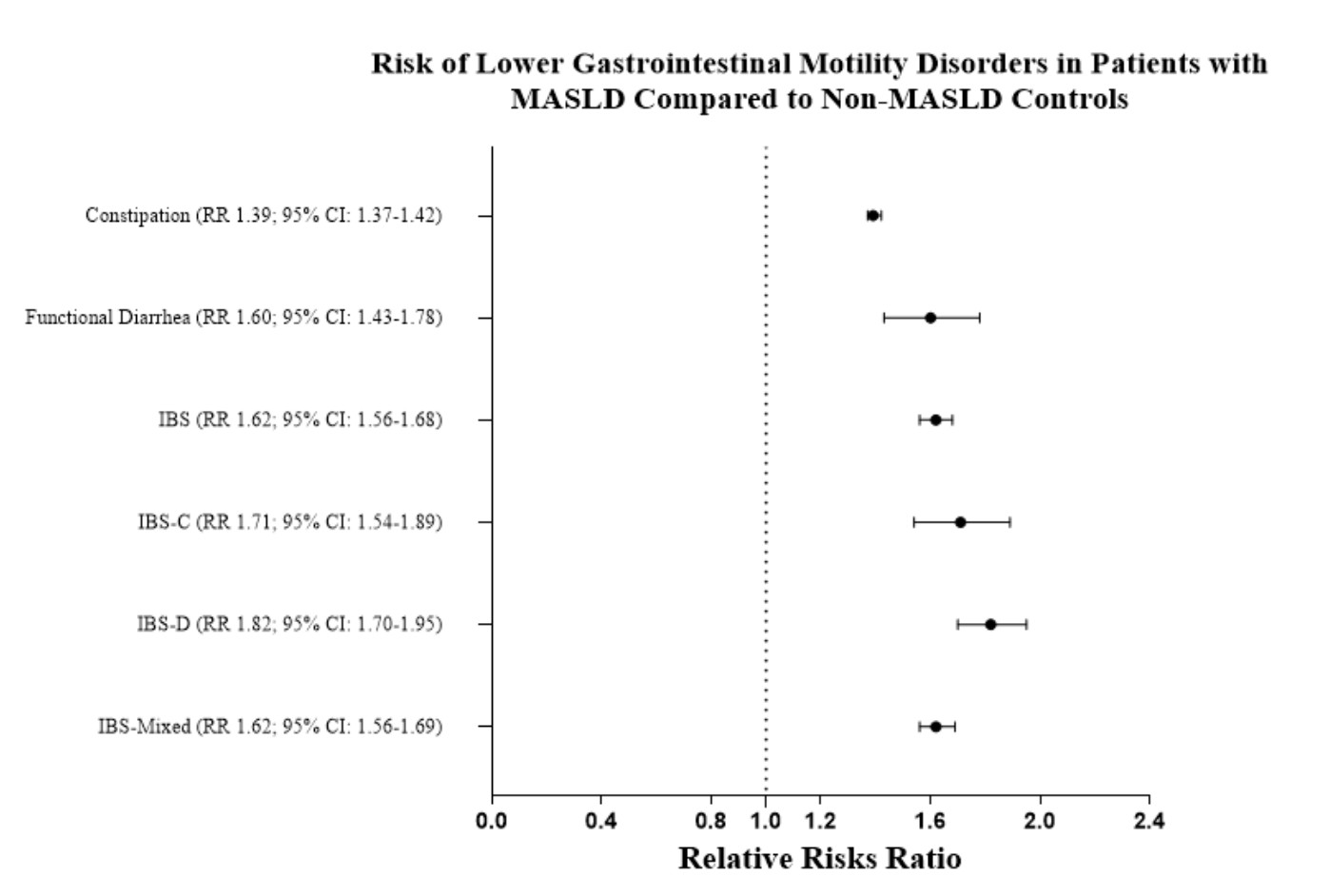
Figure: Forest plot of relative risks (RR) with 95% confidence intervals for lower gastrointestinal motility disorders in MASLD versus non-MASLD patients.
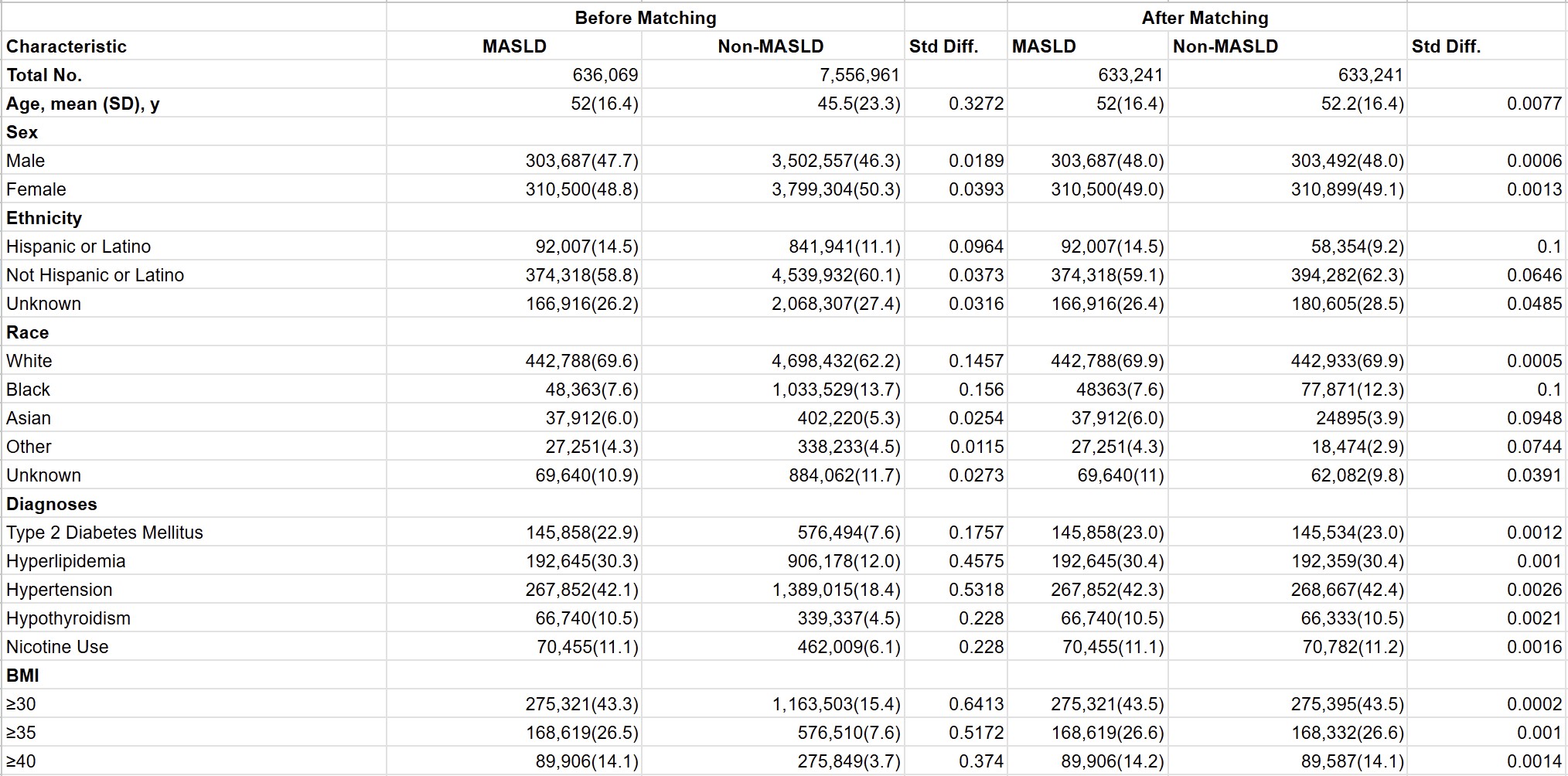
Figure: Baseline Demographics, Comorbidities, and BMI in Patients With and Without MASLD Before and After Propensity Score Matching (MASLD = Metabolic Dysfunction-Associated Steatotic Liver Disease)
Disclosures:
Rishi Chowdhary indicated no relevant financial relationships.
Thai Hau Koo indicated no relevant financial relationships.
Rohit Goyal indicated no relevant financial relationships.
Venkata Sunkesula indicated no relevant financial relationships.
Yan Sun indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Rishi Chowdhary, MD1, Thai Hau Koo, MD2, Rohit Goyal, MD3, Venkata Sunkesula, MD1, Yan Sun, MD1, Gengqing Song, MD4. P0793 - Association of Metabolic Dysfunction-Associated Steatotic Liver Disease With Lower Gastrointestinal Motility Disorders: A Nationwide Population-Based Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
