Sunday Poster Session
Category: Esophagus
P0763 - A Rare Presentation of Black Esophagus: Full-Length AEN in the Setting of Ischemic Cardiomyopathy
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Sergio Manzur, MS (he/him/his)
Universidad Católica de Santiago de Guayaquil
Guayquil, Guayas, Ecuador
Presenting Author(s)
Francisco Cano, MD1, Sergio Manzur, MS2, Monica Guillen, MS2, Wilton Cueva, MS2, Daniel Leal, MS2, Maria Jose Cueva, MD2
1Hospital Alfredo G. Paulson, Guayaquil, Guayas, Ecuador; 2Universidad Católica de Santiago de Guayaquil, Guayaquil, Guayas, Ecuador
Introduction: Acute esophageal necrosis is an infrequent clinical entity characterized by severe ischemic injury to the esophageal mucosa. It typically manifests as a diffuse circumferential black discoloration of the mucosa, predominantly involving the distal esophagus with an abrupt demarcation at the gastroesophageal junction.
Case Description/
Methods: A 73-year-old man presented to the emergency room after experiencing progressive chest pain, orthopnea, and impaired ventilatory mechanics for three weeks. He had a long-standing history of hypertension, myocardial infarction, and diabetes mellitus. Clinical evaluation was suggestive of an acute decompensation of chronic heart failure with reduced ejection fraction (HFrEF), necessitating admission to the intensive care unit (ICU). While receiving treatment, he experienced an episode of gastrointestinal bleeding manifested by hematemesis, for which an esophagogastroduodenoscopy (EGD) was performed. Ascending linear ulcers of moderate depth were observed. In the distal third, the mucosa appeared denuded with looped vascularization, extensive areas of ischemia, and marked friability, suggestive of an ischemic rather than peptic etiology. Following diagnosis, the patient was initiated on intravenous omeprazole 40 mg daily. Forty-eight hours post-procedure, the patient experienced abrupt clinical deterioration characterized by hemodynamic instability, followed by cardiopulmonary arrest resulting in death.
Discussion: Acute esophageal necrosis is identified in only 0.01–0.28% of upper endoscopies, yet it carries a mortality rate that can approach 50%. This particular patient presented with the rare full-length variant—characterized by circumferential black mucosa extending from the upper to the distal third of the esophagus—a pattern reported in fewer than 10% of cases and associated with complications such as perforation, mediastinitis, and late stricture formation. The patient received care in accordance with current clinical guidelines; however, the outcome was unfavorable. Although ischemic involvement of the esophagus is rare, this case highlights the crucial role of timely diagnosis in potentially altering clinical outcomes. It further contributes to the growing recognition of acute esophageal necrosis as a severe complication in critically ill patients—particularly those with underlying cardiovascular disease—and emphasizes the importance of maintaining a high index of suspicion and initiating prompt intervention.
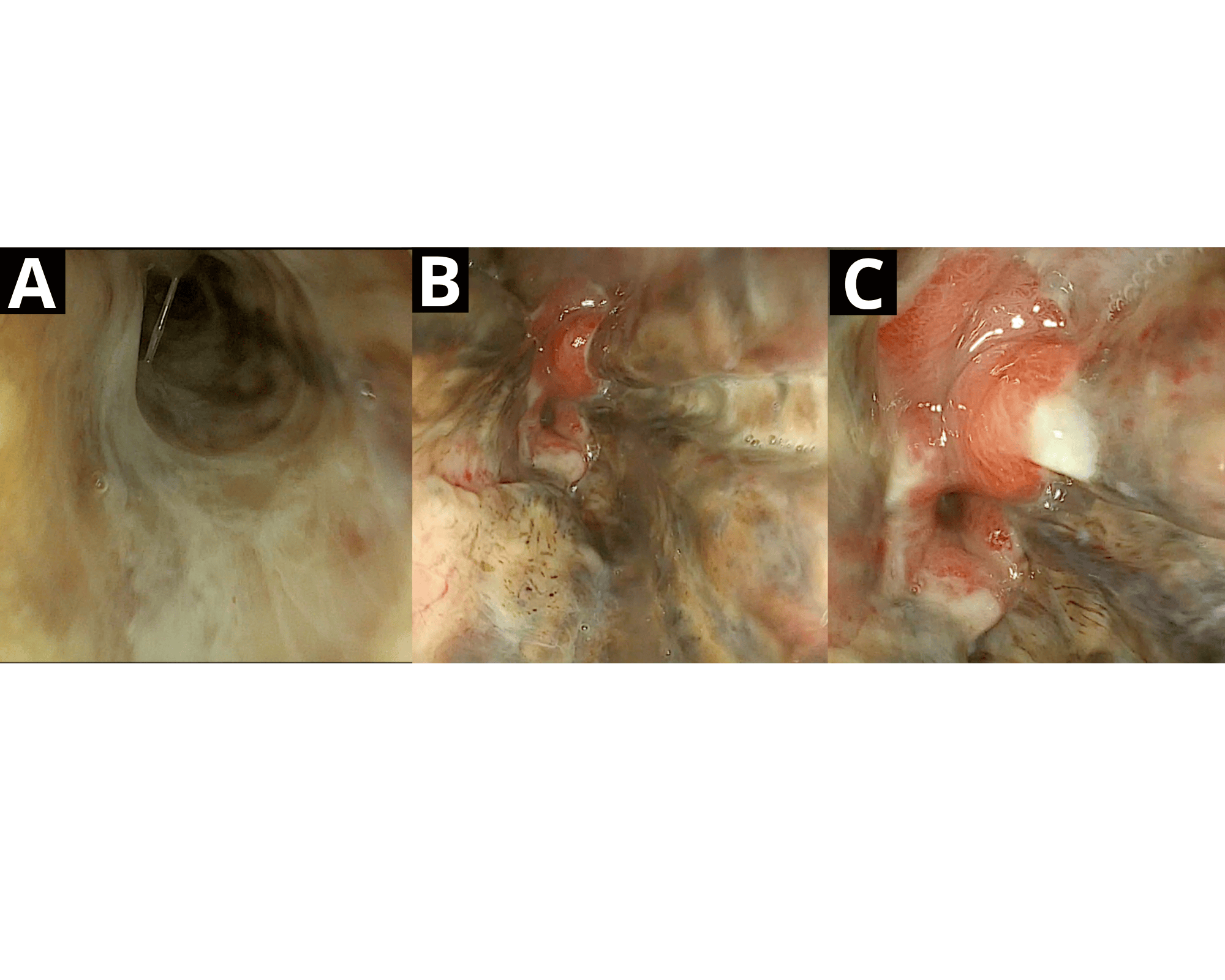
Figure: (A) Upper third of the esophagus, demonstrating extensive mucosal involvement of the organ (B) Distal third of the esophagus, showing full-thickness mucosal involvement with extensive ulcerations and areas of necrosis (C) Z-line with abrupt transition of ischemic involvement corresponding to the distinct vascular supply of each structure
Disclosures:
Francisco Cano indicated no relevant financial relationships.
Sergio Manzur indicated no relevant financial relationships.
Monica Guillen indicated no relevant financial relationships.
Wilton Cueva indicated no relevant financial relationships.
Daniel Leal indicated no relevant financial relationships.
Maria Jose Cueva indicated no relevant financial relationships.
Francisco Cano, MD1, Sergio Manzur, MS2, Monica Guillen, MS2, Wilton Cueva, MS2, Daniel Leal, MS2, Maria Jose Cueva, MD2. P0763 - A Rare Presentation of Black Esophagus: Full-Length AEN in the Setting of Ischemic Cardiomyopathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Hospital Alfredo G. Paulson, Guayaquil, Guayas, Ecuador; 2Universidad Católica de Santiago de Guayaquil, Guayaquil, Guayas, Ecuador
Introduction: Acute esophageal necrosis is an infrequent clinical entity characterized by severe ischemic injury to the esophageal mucosa. It typically manifests as a diffuse circumferential black discoloration of the mucosa, predominantly involving the distal esophagus with an abrupt demarcation at the gastroesophageal junction.
Case Description/
Methods: A 73-year-old man presented to the emergency room after experiencing progressive chest pain, orthopnea, and impaired ventilatory mechanics for three weeks. He had a long-standing history of hypertension, myocardial infarction, and diabetes mellitus. Clinical evaluation was suggestive of an acute decompensation of chronic heart failure with reduced ejection fraction (HFrEF), necessitating admission to the intensive care unit (ICU). While receiving treatment, he experienced an episode of gastrointestinal bleeding manifested by hematemesis, for which an esophagogastroduodenoscopy (EGD) was performed. Ascending linear ulcers of moderate depth were observed. In the distal third, the mucosa appeared denuded with looped vascularization, extensive areas of ischemia, and marked friability, suggestive of an ischemic rather than peptic etiology. Following diagnosis, the patient was initiated on intravenous omeprazole 40 mg daily. Forty-eight hours post-procedure, the patient experienced abrupt clinical deterioration characterized by hemodynamic instability, followed by cardiopulmonary arrest resulting in death.
Discussion: Acute esophageal necrosis is identified in only 0.01–0.28% of upper endoscopies, yet it carries a mortality rate that can approach 50%. This particular patient presented with the rare full-length variant—characterized by circumferential black mucosa extending from the upper to the distal third of the esophagus—a pattern reported in fewer than 10% of cases and associated with complications such as perforation, mediastinitis, and late stricture formation. The patient received care in accordance with current clinical guidelines; however, the outcome was unfavorable. Although ischemic involvement of the esophagus is rare, this case highlights the crucial role of timely diagnosis in potentially altering clinical outcomes. It further contributes to the growing recognition of acute esophageal necrosis as a severe complication in critically ill patients—particularly those with underlying cardiovascular disease—and emphasizes the importance of maintaining a high index of suspicion and initiating prompt intervention.
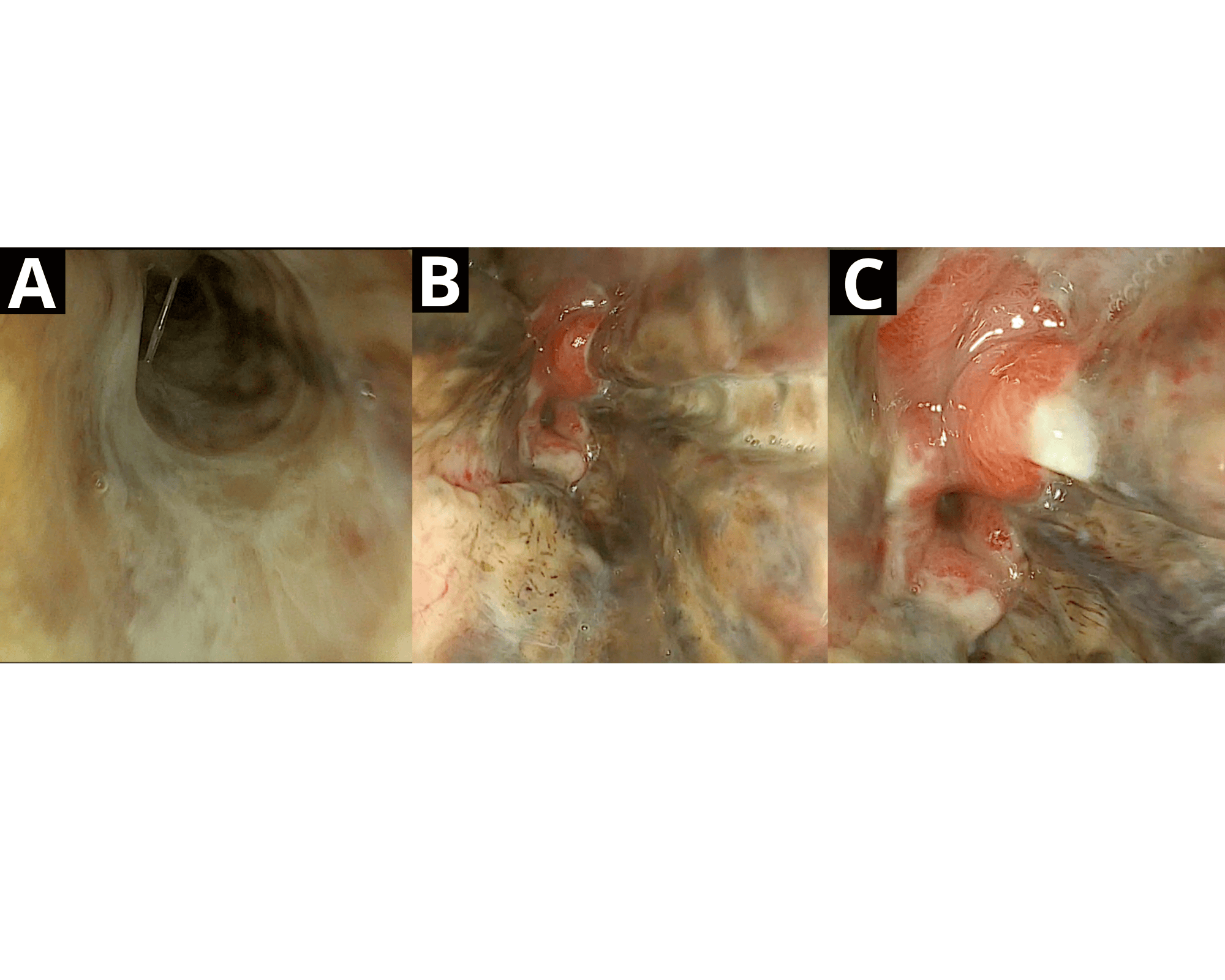
Figure: (A) Upper third of the esophagus, demonstrating extensive mucosal involvement of the organ (B) Distal third of the esophagus, showing full-thickness mucosal involvement with extensive ulcerations and areas of necrosis (C) Z-line with abrupt transition of ischemic involvement corresponding to the distinct vascular supply of each structure
Disclosures:
Francisco Cano indicated no relevant financial relationships.
Sergio Manzur indicated no relevant financial relationships.
Monica Guillen indicated no relevant financial relationships.
Wilton Cueva indicated no relevant financial relationships.
Daniel Leal indicated no relevant financial relationships.
Maria Jose Cueva indicated no relevant financial relationships.
Francisco Cano, MD1, Sergio Manzur, MS2, Monica Guillen, MS2, Wilton Cueva, MS2, Daniel Leal, MS2, Maria Jose Cueva, MD2. P0763 - A Rare Presentation of Black Esophagus: Full-Length AEN in the Setting of Ischemic Cardiomyopathy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
