Sunday Poster Session
Category: Esophagus
P0756 - Acute Esophageal Dilation and Necrosis Complicated by Tracheoesophageal Fistula
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rebhi Rabah, MD (he/him/his)
SUNY Downstate Health Sciences University
Brooklyn, NY
Presenting Author(s)
Rebhi Rabah, MD1, Fariha Chowdhury, MD2, Selome Yewedalsew, MD1, Tarah Magloire, MD3, Sohum Patwa, MD1, Yaniuska Lescaille, MD, MPH4
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2Garnet Health Medical Center, Brooklyn, NY; 3SUNY Downstate Medical Center, Brooklyn, NY; 4NYC Health + Hospitals/Kings County, Brooklyn, NY
Introduction: Acute dilation of the esophagus is a rare and poorly studied condition. This phenomenon can occur in the setting of critically ill patients. Acute dilation of the esophagus can be seen in various clinical pictures such as acute necrosis of the esophagus. Very few cases have been seen with acute dilation of the esophagus leading to tracheoesophageal fistula. We present a case of acute dilation of the esophagus likely secondary to esophageal necrosis and complicated by tracheoesophageal fistula (TEF).
Case Description/
Methods: We present the case of a 49-year-old female with a history of hypertension, prediabetes, alcohol use disorder, and seizures who was admitted for altered mental status. Vitals were concerning for septic shock. Labs were significant for venous lactate of 3.2 mmol/L and white blood cell count elevated to 15,750 k/uL. Chest Xray was significant for bilateral patchy opacities. After admission, the patient developed acute hypoxic respiratory failure requiring intubation and was transferred to the MICU. On day 5 of admission, CTA of chest revealed new esophageal distention with diverticula and wall thickening for which gastroenterology was consulted. EGD was performed to elucidate the etiology of the patients dilated esophagus. EGD was notable for esophageal necrosis, possibly from ischemia vs infection. Shortly after the procedure, the patient's hemodynamics deteriorated and imaging was obtained to assess for a perforation which revealed a TEF but no free air or free fluid suggestive of a perforation. The patient was not a candidate for an esophageal stent due to esophageal necrosis. Patient was then emergently transferred to another facility for tracheal stenting.
Discussion: Necrosis of the upper gastrointestinal tract can develop in longstanding intubation without proper decompression. In critically ill patients, acute esophageal dilation can occur secondary to ischemia and infection. Our case is novel in that it highlights an uncommon progression from acute esophageal dilation to necrosis and development of a TEF. In this case the esophageal necrosis is likely due to patients septic shock. However, TEF normally requires longer periods of mechanical ventilation to develop. Additionally, the necrosis found during endoscopy limit options for intervention as the patient is not a candidate for esophageal stenting. This case highlights the importance of multidisciplinary management and the need for further research on acute esophageal dilation especially in a critical care setting.
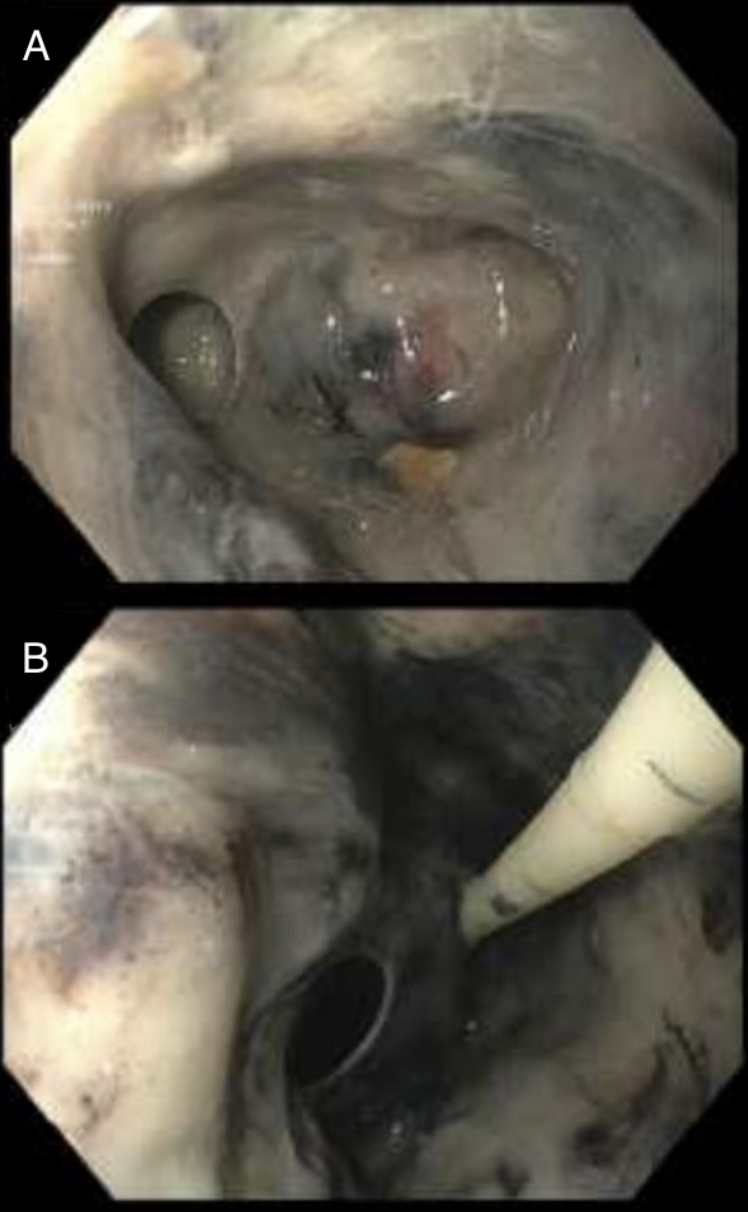
Figure: Figure 1. EGD revealing abnormal dusky mucosa concerning for ischemia (A) and necrosis (B) in the lower one third of the esophagus.
Disclosures:
Rebhi Rabah indicated no relevant financial relationships.
Fariha Chowdhury indicated no relevant financial relationships.
Selome Yewedalsew indicated no relevant financial relationships.
Tarah Magloire indicated no relevant financial relationships.
Sohum Patwa indicated no relevant financial relationships.
Yaniuska Lescaille indicated no relevant financial relationships.
Rebhi Rabah, MD1, Fariha Chowdhury, MD2, Selome Yewedalsew, MD1, Tarah Magloire, MD3, Sohum Patwa, MD1, Yaniuska Lescaille, MD, MPH4. P0756 - Acute Esophageal Dilation and Necrosis Complicated by Tracheoesophageal Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Downstate Health Sciences University, Brooklyn, NY; 2Garnet Health Medical Center, Brooklyn, NY; 3SUNY Downstate Medical Center, Brooklyn, NY; 4NYC Health + Hospitals/Kings County, Brooklyn, NY
Introduction: Acute dilation of the esophagus is a rare and poorly studied condition. This phenomenon can occur in the setting of critically ill patients. Acute dilation of the esophagus can be seen in various clinical pictures such as acute necrosis of the esophagus. Very few cases have been seen with acute dilation of the esophagus leading to tracheoesophageal fistula. We present a case of acute dilation of the esophagus likely secondary to esophageal necrosis and complicated by tracheoesophageal fistula (TEF).
Case Description/
Methods: We present the case of a 49-year-old female with a history of hypertension, prediabetes, alcohol use disorder, and seizures who was admitted for altered mental status. Vitals were concerning for septic shock. Labs were significant for venous lactate of 3.2 mmol/L and white blood cell count elevated to 15,750 k/uL. Chest Xray was significant for bilateral patchy opacities. After admission, the patient developed acute hypoxic respiratory failure requiring intubation and was transferred to the MICU. On day 5 of admission, CTA of chest revealed new esophageal distention with diverticula and wall thickening for which gastroenterology was consulted. EGD was performed to elucidate the etiology of the patients dilated esophagus. EGD was notable for esophageal necrosis, possibly from ischemia vs infection. Shortly after the procedure, the patient's hemodynamics deteriorated and imaging was obtained to assess for a perforation which revealed a TEF but no free air or free fluid suggestive of a perforation. The patient was not a candidate for an esophageal stent due to esophageal necrosis. Patient was then emergently transferred to another facility for tracheal stenting.
Discussion: Necrosis of the upper gastrointestinal tract can develop in longstanding intubation without proper decompression. In critically ill patients, acute esophageal dilation can occur secondary to ischemia and infection. Our case is novel in that it highlights an uncommon progression from acute esophageal dilation to necrosis and development of a TEF. In this case the esophageal necrosis is likely due to patients septic shock. However, TEF normally requires longer periods of mechanical ventilation to develop. Additionally, the necrosis found during endoscopy limit options for intervention as the patient is not a candidate for esophageal stenting. This case highlights the importance of multidisciplinary management and the need for further research on acute esophageal dilation especially in a critical care setting.
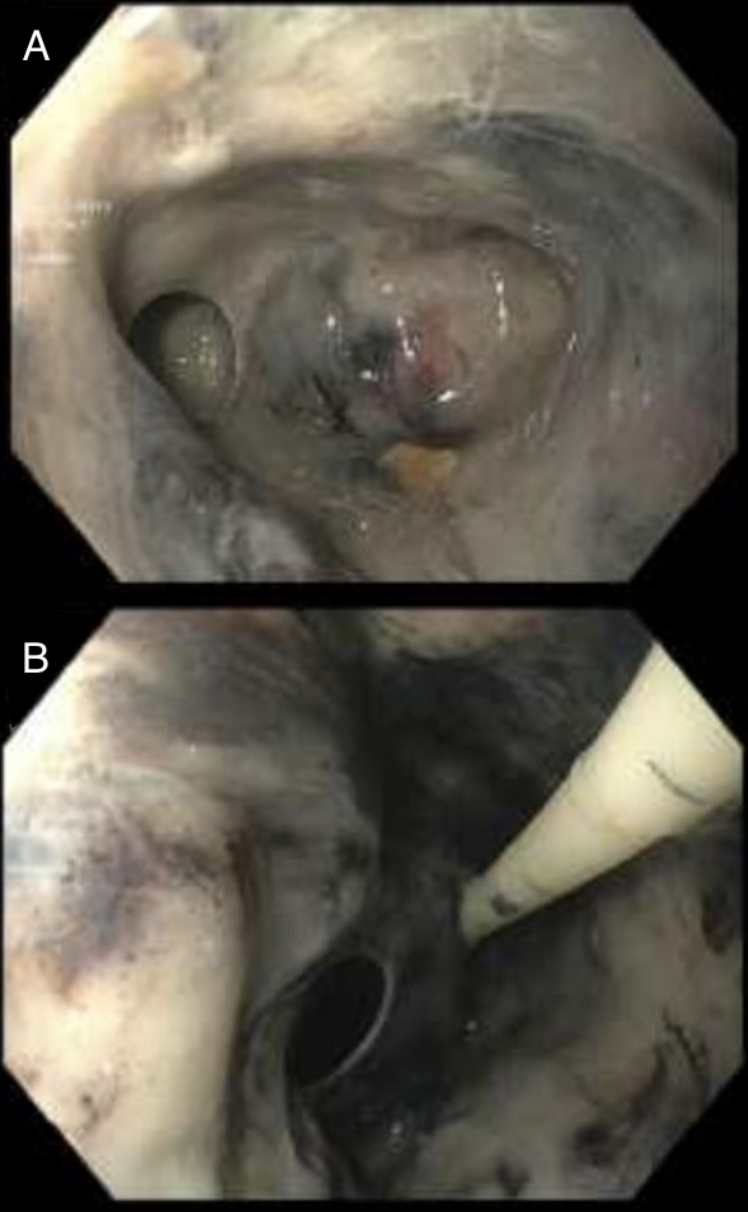
Figure: Figure 1. EGD revealing abnormal dusky mucosa concerning for ischemia (A) and necrosis (B) in the lower one third of the esophagus.
Disclosures:
Rebhi Rabah indicated no relevant financial relationships.
Fariha Chowdhury indicated no relevant financial relationships.
Selome Yewedalsew indicated no relevant financial relationships.
Tarah Magloire indicated no relevant financial relationships.
Sohum Patwa indicated no relevant financial relationships.
Yaniuska Lescaille indicated no relevant financial relationships.
Rebhi Rabah, MD1, Fariha Chowdhury, MD2, Selome Yewedalsew, MD1, Tarah Magloire, MD3, Sohum Patwa, MD1, Yaniuska Lescaille, MD, MPH4. P0756 - Acute Esophageal Dilation and Necrosis Complicated by Tracheoesophageal Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
