Sunday Poster Session
Category: Esophagus
P0750 - A Diverting Diagnosis: When Epiphrenic Diverticulum Masquerades as Esophageal Perforation
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Jessica E. McClain, MD
University of Illinois Chicago
Chicago, IL
Presenting Author(s)
Jessica E. McClain, MD1, James S. Love, MD2, Asim Shuja, MD1
1University of Illinois Chicago, Chicago, IL; 2University of Illinois College of Medicine, Chicago, IL
Introduction: Esophageal diverticula (ED) are outpouchings of the esophageal wall, classified by location and etiology. Zenker’s and epiphrenic diverticula are pulsion-type, resulting from increased intraluminal pressure due to esophageal dysmotility. Traction diverticula are true diverticula involving all layers of the esophageal wall, typically occurring in the mid-esophagus due to external traction from mediastinal inflammation. Symptoms of ED include dysphagia, regurgitation, and chest pain. Complications can involve aspiration, perforation, fistula formation, and malignant transformation. Diagnosis is primarily through barium esophagram, though some cases are identified incidentally via esophagogastroduodenoscopy (EGD) or radiographic imaging. We present a case of a 65-year-old woman suspected of having an esophageal perforation; however, the diagnostic EGD revealed an undiagnosed epiphrenic diverticulum instead.
Case Description/
Methods: A 65-year-old woman with heart failure was transferred for neurosurgical evaluation after being found to have C1-C2 subluxation and a T2 odontoid fracture. Surgical intervention was deferred due to acute decompensated heart failure. Her condition was further complicated by pulseless electrical activity (PEA) arrest requiring resuscitation and biventricular impella support. Following intubation, a nasogastric tube (NGT) was placed. CT chest was significant for bilateral consolidations suggestive of aspiration pneumonia, as well as an NGT deviating to the right lung base possibly within a distal ruptured esophagus (Figure 1). Radiology recommended removal of NGT and emergent EGD, which revealed a large epiphrenic diverticulum without perforation (Figure 2). Despite aggressive treatment, the patient developed multiorgan failure and died.
Discussion: Our patient with an undiagnosed ED likely experienced aspiration due to food or liquid accumulation within the pouch, leading to pulmonary compromise. This aspiration may have precipitated the PEA arrest, a recognized complication of an ED. Such cases emphasize the importance of considering structural esophageal abnormalities in patients presenting with unexplained cardiac arrest, particularly when aspiration is suspected. Interestingly, on review of the patient’s chart, a CT chest at an outside hospital two months prior revealed a massively dilated esophagus filled with debris, which was not explored further. Early recognition and appropriate management are crucial to prevent potential complications associated with ED.
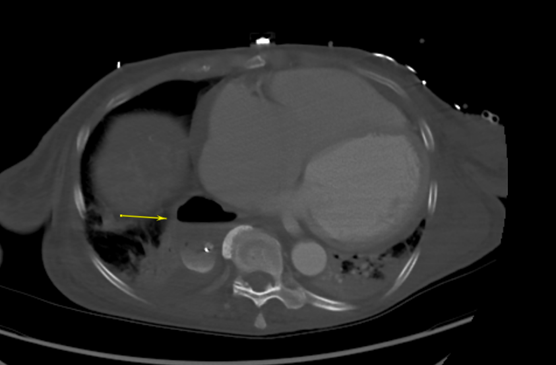
Figure: Figure 1. Computed tomography of the chest showing a right posterior medial basilar air or fluid collection with trace layering contrast concerning for esophageal rupture

Figure: Figure 2. Lower third of the esophagus, arrow pointing at the lower esophageal diverticulum and arrowhead pointing at the gastroesophageal junction
Disclosures:
Jessica McClain indicated no relevant financial relationships.
James Love indicated no relevant financial relationships.
Asim Shuja indicated no relevant financial relationships.
Jessica E. McClain, MD1, James S. Love, MD2, Asim Shuja, MD1. P0750 - A Diverting Diagnosis: When Epiphrenic Diverticulum Masquerades as Esophageal Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Illinois Chicago, Chicago, IL; 2University of Illinois College of Medicine, Chicago, IL
Introduction: Esophageal diverticula (ED) are outpouchings of the esophageal wall, classified by location and etiology. Zenker’s and epiphrenic diverticula are pulsion-type, resulting from increased intraluminal pressure due to esophageal dysmotility. Traction diverticula are true diverticula involving all layers of the esophageal wall, typically occurring in the mid-esophagus due to external traction from mediastinal inflammation. Symptoms of ED include dysphagia, regurgitation, and chest pain. Complications can involve aspiration, perforation, fistula formation, and malignant transformation. Diagnosis is primarily through barium esophagram, though some cases are identified incidentally via esophagogastroduodenoscopy (EGD) or radiographic imaging. We present a case of a 65-year-old woman suspected of having an esophageal perforation; however, the diagnostic EGD revealed an undiagnosed epiphrenic diverticulum instead.
Case Description/
Methods: A 65-year-old woman with heart failure was transferred for neurosurgical evaluation after being found to have C1-C2 subluxation and a T2 odontoid fracture. Surgical intervention was deferred due to acute decompensated heart failure. Her condition was further complicated by pulseless electrical activity (PEA) arrest requiring resuscitation and biventricular impella support. Following intubation, a nasogastric tube (NGT) was placed. CT chest was significant for bilateral consolidations suggestive of aspiration pneumonia, as well as an NGT deviating to the right lung base possibly within a distal ruptured esophagus (Figure 1). Radiology recommended removal of NGT and emergent EGD, which revealed a large epiphrenic diverticulum without perforation (Figure 2). Despite aggressive treatment, the patient developed multiorgan failure and died.
Discussion: Our patient with an undiagnosed ED likely experienced aspiration due to food or liquid accumulation within the pouch, leading to pulmonary compromise. This aspiration may have precipitated the PEA arrest, a recognized complication of an ED. Such cases emphasize the importance of considering structural esophageal abnormalities in patients presenting with unexplained cardiac arrest, particularly when aspiration is suspected. Interestingly, on review of the patient’s chart, a CT chest at an outside hospital two months prior revealed a massively dilated esophagus filled with debris, which was not explored further. Early recognition and appropriate management are crucial to prevent potential complications associated with ED.
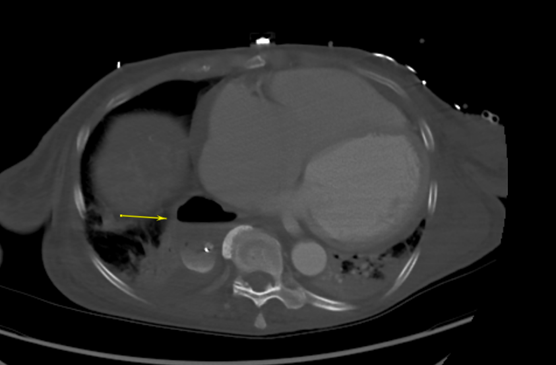
Figure: Figure 1. Computed tomography of the chest showing a right posterior medial basilar air or fluid collection with trace layering contrast concerning for esophageal rupture

Figure: Figure 2. Lower third of the esophagus, arrow pointing at the lower esophageal diverticulum and arrowhead pointing at the gastroesophageal junction
Disclosures:
Jessica McClain indicated no relevant financial relationships.
James Love indicated no relevant financial relationships.
Asim Shuja indicated no relevant financial relationships.
Jessica E. McClain, MD1, James S. Love, MD2, Asim Shuja, MD1. P0750 - A Diverting Diagnosis: When Epiphrenic Diverticulum Masquerades as Esophageal Perforation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
