Sunday Poster Session
Category: Esophagus
P0746 - Between a Rock and Esophageal Space: Calcified Leiomyoma
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- AV
Amberly Vaughan, MD (she/her/hers)
Keesler Medical Center
Biloxi, MS
Presenting Author(s)
Amberly Vaughan, MD, Rachel Pray, DO, Wassem Juakiem, MD
Keesler Medical Center, Biloxi, MS
Introduction: Leiomyomas are a rare albeit benign cause of esophageal subepithelial tumor with an incidence less than 1%. Similar to gastrointestinal stromal tumors (GIST), metastasis, and other more common causes of esophageal lesions, leiomyomas appear hypoechoic on endoscopic ultrasound (EUS), necessitating pathologic tissue diagnosis. The finding of dystrophic calcification in leiomyoma is exceedingly rare, but calcification of esophageal masses is seen almost exclusively in leiomyomas.
Case Description/
Methods: A 71-year-old prior Navy radio technician with history of papillary thyroid carcinoma status post thyroidectomy was initially admitted for evaluation after a mechanical fall with loss of consciousness. Workup of incidental findings, including exudative pleural and pericardial effusions with negative cytology, also revealed a partially calcified gastroesophageal (GE) junction mass on contrast-enhanced CT. Esophagogastroduodenoscopy (EGD) with EUS showed a well-defined hypoechoic calcified intramural lesion at the GE junction, appearing to originate from within the muscularis propria. Fine-needle biopsy confirmed the diagnosis of leiomyoma. It was not resected in the absence of symptoms.
Discussion: We present a rare case of esophageal leiomyoma, a benign smooth muscle tumor originating from the muscularis mucosa or muscularis propria. Symptomatic gastrointestinal subepithelial lesions (SEL) are typically resected. For asymptomatic SEL, EUS differentiates intramural versus extramural. EUS further characterizes lesions as anechoic (e.g. vascular, cystic), hyperechoic (lipoma), or hypoechoic (e.g. GIST, leiomyoma, neuroendocrine, nerve sheath tumor, metastasis). Tissue diagnosis is recommended for hypoechoic lesions, as the sensitivity and specificity of EUS alone for differentiating benign from malignant are 64-80% and 77-80%, respectively. The incidence of esophageal leiomyoma is approximately 0.005%, but about two thirds of benign esophageal tumors are leiomyomas. Additionally, calcification of leiomyomas is unusual, seen in less than 2% of cases. The homogeneous, hypoechoic, regular margins of leiomyomas seen on EUS can suggest the benign tumor over more common etiologies, and calcification in esophageal masses is seen almost exclusively in leiomyomas. Pathologic staining confirmed diagnosis. Most initially small and asymptomatic leiomyomas never have symptomatic progression. Surveillance interval in cases of asymptomatic SEL with low malignant potential is on a case-by-case basis.
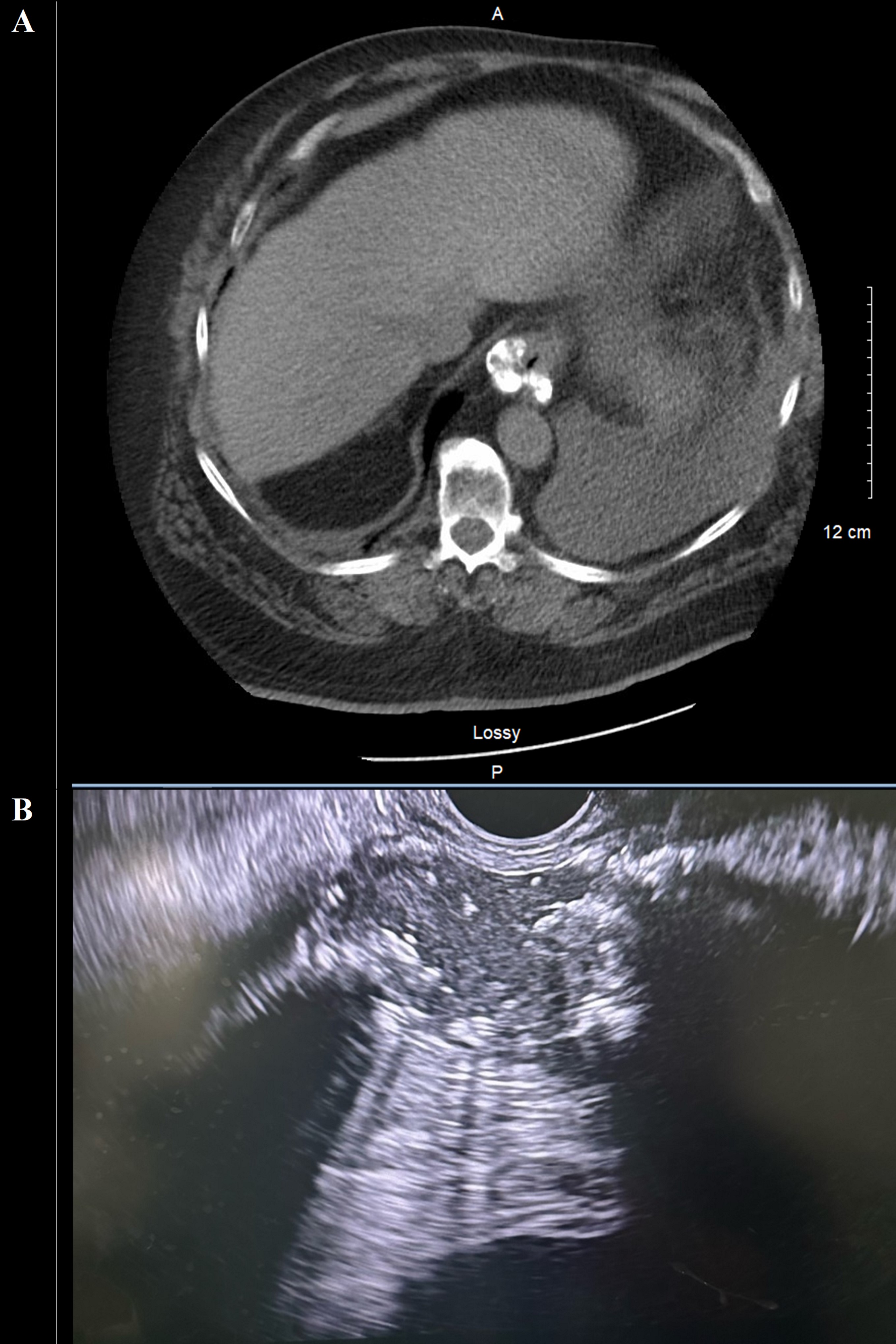
Figure: (A) Calcified esophageal mass (B) EUS showed a well-defined hypoechoic calcified intramural lesion.
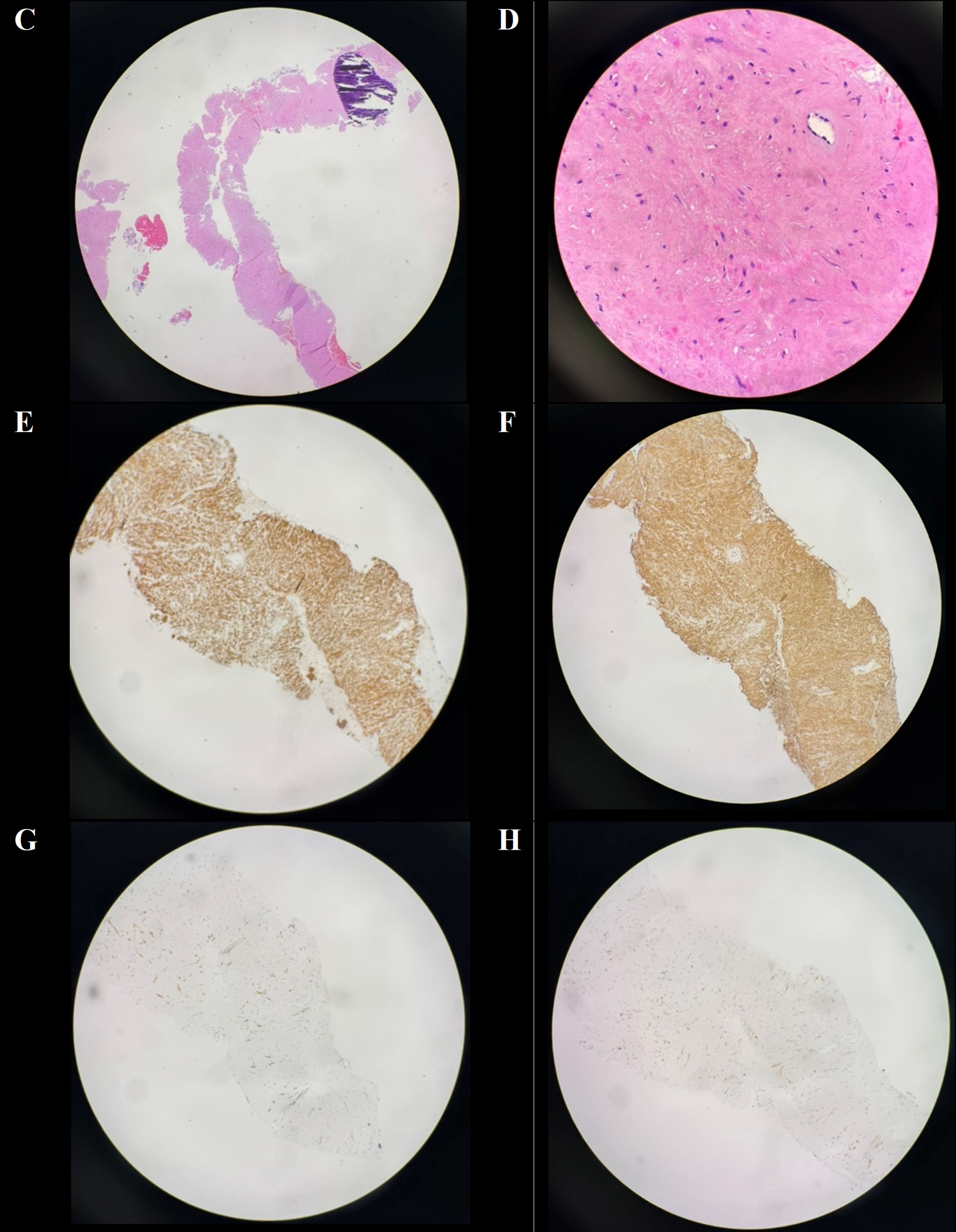
Figure: (C-D) H&E with bland spindle cell proliferation, dystrophic calcification, no atypia, no mitoses (E-F) IHC positive for desmin and smooth muscle actin, respectively, suggests leiomyoma. (G-H) IHC negative for CD117 (c-kit) and DOG-1, respectively, makes GIST less likely.
Disclosures:
Amberly Vaughan indicated no relevant financial relationships.
Rachel Pray indicated no relevant financial relationships.
Wassem Juakiem indicated no relevant financial relationships.
Amberly Vaughan, MD, Rachel Pray, DO, Wassem Juakiem, MD. P0746 - Between a Rock and Esophageal Space: Calcified Leiomyoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Keesler Medical Center, Biloxi, MS
Introduction: Leiomyomas are a rare albeit benign cause of esophageal subepithelial tumor with an incidence less than 1%. Similar to gastrointestinal stromal tumors (GIST), metastasis, and other more common causes of esophageal lesions, leiomyomas appear hypoechoic on endoscopic ultrasound (EUS), necessitating pathologic tissue diagnosis. The finding of dystrophic calcification in leiomyoma is exceedingly rare, but calcification of esophageal masses is seen almost exclusively in leiomyomas.
Case Description/
Methods: A 71-year-old prior Navy radio technician with history of papillary thyroid carcinoma status post thyroidectomy was initially admitted for evaluation after a mechanical fall with loss of consciousness. Workup of incidental findings, including exudative pleural and pericardial effusions with negative cytology, also revealed a partially calcified gastroesophageal (GE) junction mass on contrast-enhanced CT. Esophagogastroduodenoscopy (EGD) with EUS showed a well-defined hypoechoic calcified intramural lesion at the GE junction, appearing to originate from within the muscularis propria. Fine-needle biopsy confirmed the diagnosis of leiomyoma. It was not resected in the absence of symptoms.
Discussion: We present a rare case of esophageal leiomyoma, a benign smooth muscle tumor originating from the muscularis mucosa or muscularis propria. Symptomatic gastrointestinal subepithelial lesions (SEL) are typically resected. For asymptomatic SEL, EUS differentiates intramural versus extramural. EUS further characterizes lesions as anechoic (e.g. vascular, cystic), hyperechoic (lipoma), or hypoechoic (e.g. GIST, leiomyoma, neuroendocrine, nerve sheath tumor, metastasis). Tissue diagnosis is recommended for hypoechoic lesions, as the sensitivity and specificity of EUS alone for differentiating benign from malignant are 64-80% and 77-80%, respectively. The incidence of esophageal leiomyoma is approximately 0.005%, but about two thirds of benign esophageal tumors are leiomyomas. Additionally, calcification of leiomyomas is unusual, seen in less than 2% of cases. The homogeneous, hypoechoic, regular margins of leiomyomas seen on EUS can suggest the benign tumor over more common etiologies, and calcification in esophageal masses is seen almost exclusively in leiomyomas. Pathologic staining confirmed diagnosis. Most initially small and asymptomatic leiomyomas never have symptomatic progression. Surveillance interval in cases of asymptomatic SEL with low malignant potential is on a case-by-case basis.
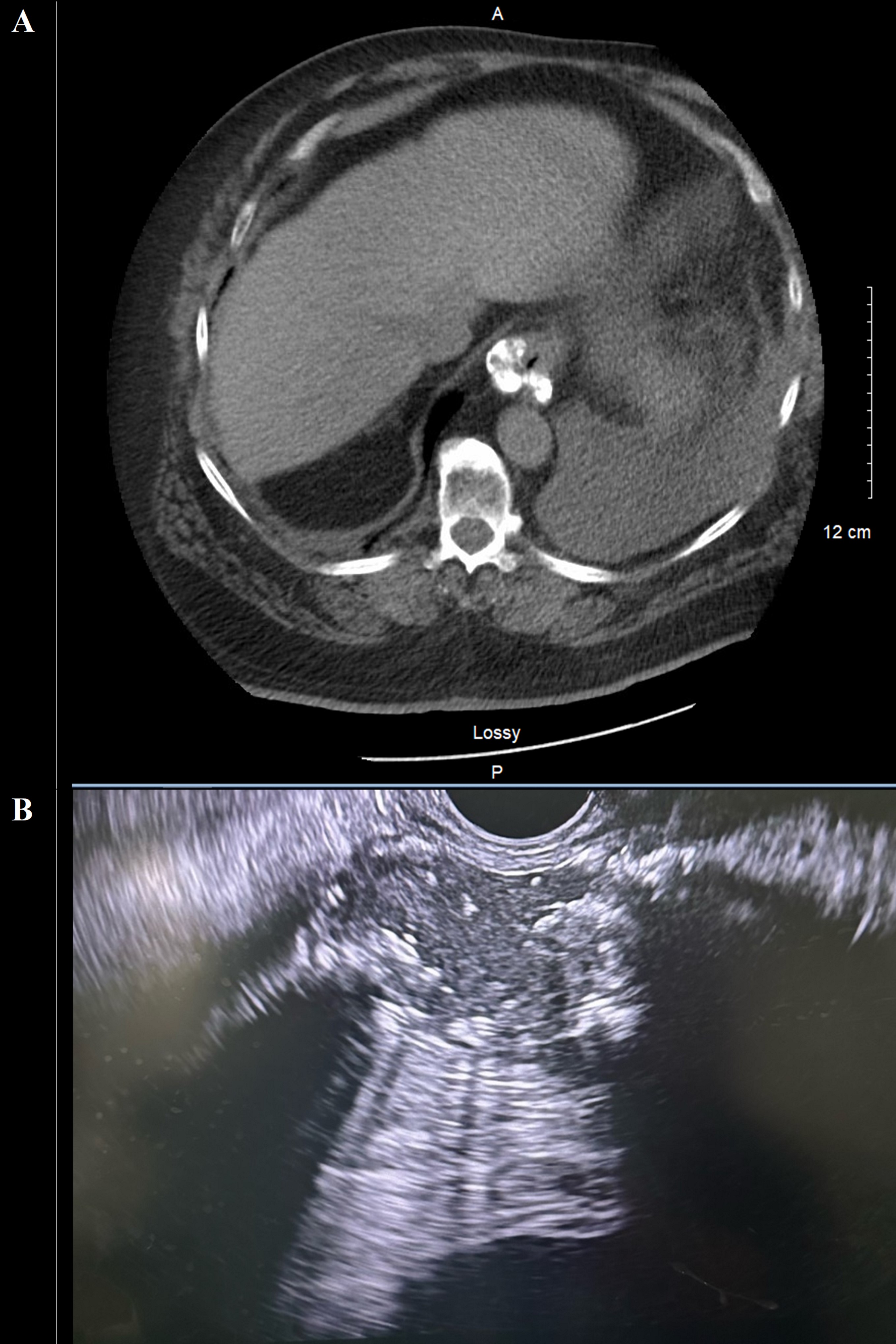
Figure: (A) Calcified esophageal mass (B) EUS showed a well-defined hypoechoic calcified intramural lesion.
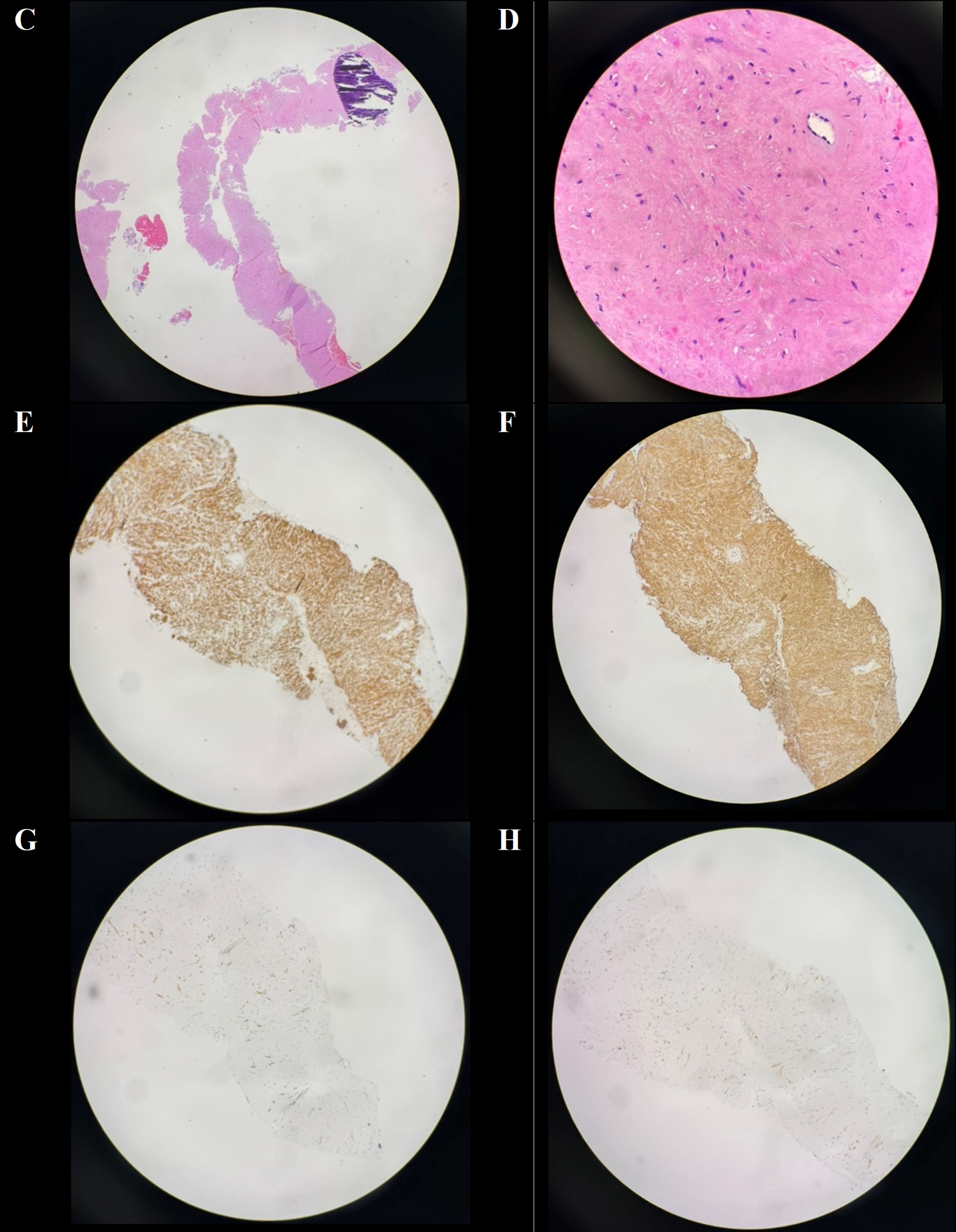
Figure: (C-D) H&E with bland spindle cell proliferation, dystrophic calcification, no atypia, no mitoses (E-F) IHC positive for desmin and smooth muscle actin, respectively, suggests leiomyoma. (G-H) IHC negative for CD117 (c-kit) and DOG-1, respectively, makes GIST less likely.
Disclosures:
Amberly Vaughan indicated no relevant financial relationships.
Rachel Pray indicated no relevant financial relationships.
Wassem Juakiem indicated no relevant financial relationships.
Amberly Vaughan, MD, Rachel Pray, DO, Wassem Juakiem, MD. P0746 - Between a Rock and Esophageal Space: Calcified Leiomyoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
