Sunday Poster Session
Category: Esophagus
P0741 - The Dark Side of Upper GI Bleeding: Acute Esophageal Necrosis in a Patient With Cirrhosis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Diwanshu Soni, DO
University of Arizona College of Medicine, Phoenix VA Medical Center
Phoenix, AZ
Presenting Author(s)
Diwanshu Soni, DO, Bhupinder Kaur, MD, Phoebe Newell, MD, Yasmin Alishahi, MD
University of Arizona College of Medicine, Phoenix VA Medical Center, Phoenix, AZ
Introduction: Acute esophageal necrosis is a rare condition characterized by circumferential black discoloration of the distal esophageal mucosa. Diagnosis is made via esophagogastroduodenoscopy (EGD) and treatment involves supportive care. This case highlights AEN in a patient with decompensated cirrhosis.
Case Description/
Methods: A 64-year-old male with cirrhosis due to alcohol use, esophageal varices, and chronic portal vein thrombosis presented with hematemesis. Physical exam was unremarkable. Lab results showed hemoglobin 11.9 g/dL and platelets 130 K/uL. Computed tomography (CT) abdomen/pelvis with intravenous (IV) contrast showed mild ascites and stable varices. EGD showed circumferential black, ulcerated distal esophageal mucosa suggestive of AEN (Figure 1), and two non-bleeding duodenal ulcers (Forrest Class III). No specimen were collected. Management included nil-per-os (NPO) status with IV fluids for 4 days followed by clear liquid diet. Patient was also started on sucralfate and ceftriaxone. EGD on day 7 showed significant improvement (Figure 2) and the patient was discharged on sucralfate with a follow-up EGD in 2 weeks.
Discussion: AEN is rare (0.2% incidence) and typically presents with hematemesis, melena, and anemia. EGD findings show patchy or circumferential pigmentation of the distal esophageal mucosa with a distinct demarcation from the normal mucosa at the gastroesophageal junction. The distal esophagus is prone to ischemic injury due to its watershed blood supply. Biopsy was avoided due to a 5% perforation risk. AEN has a mortality rate of 32% and risk factors include male sex, age >65, cirrhosis, diabetes, hypertension, chronic kidney disease, GERD, gastric/duodenal ulcers, hemodynamic compromise, alcohol intoxication. Cirrhosis contributes to AEN through variceal bleeding, malnutrition, impaired mucosal integrity and ability to heal. Our patient’s risk factors included male sex, duodenal ulcers, cirrhosis, and decreased esophageal blood flow due to chronic portal vein thrombosis. Management is supportive, starting with NPO for 24 hours and transitioning to oral feeds. If not tolerated, total parenteral nutrition is preferred over nasogastric feeding due to perforation risk. IV proton pump inhibitors should be initiated promptly and with clinical improvement patients can be transitioned to sucralfate to aid in mucosal healing. Early diagnosis and treatment improve outcomes, emphasizing the need for a broad differential in cirrhotic patients with upper GI bleeding.
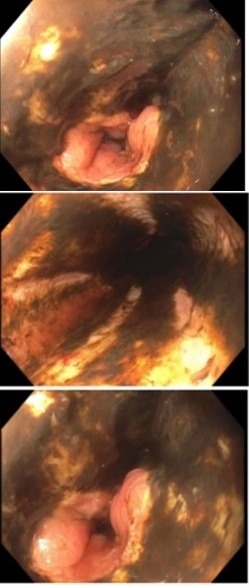
Figure: Figure 1: circumferentially ulcerated and black appearing esophageal mucosa in the distal esophagus extending from 25 cm to 35 cm.
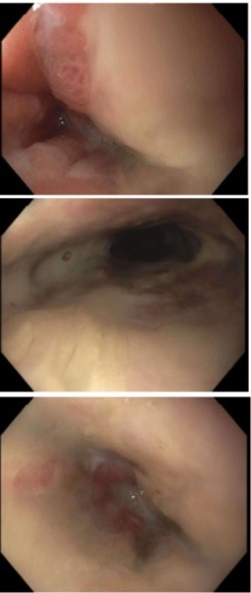
Figure: Figure 2: circumferentially ulcerated esophageal mucosa in the distal esophagus extending from 23 cm to 34 cm however it appears to be improved from prior black appearing esophagus.
Disclosures:
Diwanshu Soni indicated no relevant financial relationships.
Bhupinder Kaur indicated no relevant financial relationships.
Phoebe Newell indicated no relevant financial relationships.
Yasmin Alishahi indicated no relevant financial relationships.
Diwanshu Soni, DO, Bhupinder Kaur, MD, Phoebe Newell, MD, Yasmin Alishahi, MD. P0741 - The Dark Side of Upper GI Bleeding: Acute Esophageal Necrosis in a Patient With Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Arizona College of Medicine, Phoenix VA Medical Center, Phoenix, AZ
Introduction: Acute esophageal necrosis is a rare condition characterized by circumferential black discoloration of the distal esophageal mucosa. Diagnosis is made via esophagogastroduodenoscopy (EGD) and treatment involves supportive care. This case highlights AEN in a patient with decompensated cirrhosis.
Case Description/
Methods: A 64-year-old male with cirrhosis due to alcohol use, esophageal varices, and chronic portal vein thrombosis presented with hematemesis. Physical exam was unremarkable. Lab results showed hemoglobin 11.9 g/dL and platelets 130 K/uL. Computed tomography (CT) abdomen/pelvis with intravenous (IV) contrast showed mild ascites and stable varices. EGD showed circumferential black, ulcerated distal esophageal mucosa suggestive of AEN (Figure 1), and two non-bleeding duodenal ulcers (Forrest Class III). No specimen were collected. Management included nil-per-os (NPO) status with IV fluids for 4 days followed by clear liquid diet. Patient was also started on sucralfate and ceftriaxone. EGD on day 7 showed significant improvement (Figure 2) and the patient was discharged on sucralfate with a follow-up EGD in 2 weeks.
Discussion: AEN is rare (0.2% incidence) and typically presents with hematemesis, melena, and anemia. EGD findings show patchy or circumferential pigmentation of the distal esophageal mucosa with a distinct demarcation from the normal mucosa at the gastroesophageal junction. The distal esophagus is prone to ischemic injury due to its watershed blood supply. Biopsy was avoided due to a 5% perforation risk. AEN has a mortality rate of 32% and risk factors include male sex, age >65, cirrhosis, diabetes, hypertension, chronic kidney disease, GERD, gastric/duodenal ulcers, hemodynamic compromise, alcohol intoxication. Cirrhosis contributes to AEN through variceal bleeding, malnutrition, impaired mucosal integrity and ability to heal. Our patient’s risk factors included male sex, duodenal ulcers, cirrhosis, and decreased esophageal blood flow due to chronic portal vein thrombosis. Management is supportive, starting with NPO for 24 hours and transitioning to oral feeds. If not tolerated, total parenteral nutrition is preferred over nasogastric feeding due to perforation risk. IV proton pump inhibitors should be initiated promptly and with clinical improvement patients can be transitioned to sucralfate to aid in mucosal healing. Early diagnosis and treatment improve outcomes, emphasizing the need for a broad differential in cirrhotic patients with upper GI bleeding.
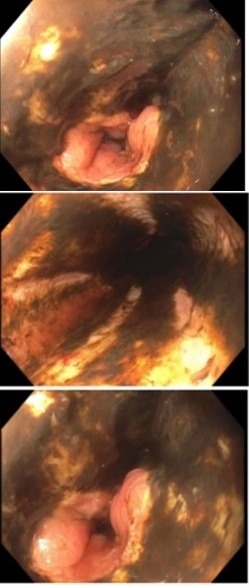
Figure: Figure 1: circumferentially ulcerated and black appearing esophageal mucosa in the distal esophagus extending from 25 cm to 35 cm.
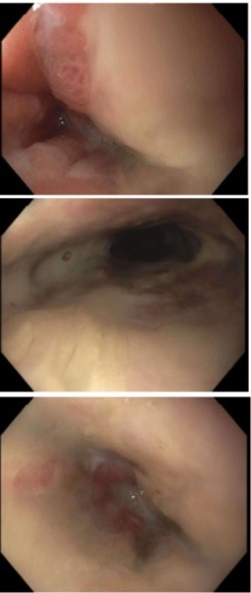
Figure: Figure 2: circumferentially ulcerated esophageal mucosa in the distal esophagus extending from 23 cm to 34 cm however it appears to be improved from prior black appearing esophagus.
Disclosures:
Diwanshu Soni indicated no relevant financial relationships.
Bhupinder Kaur indicated no relevant financial relationships.
Phoebe Newell indicated no relevant financial relationships.
Yasmin Alishahi indicated no relevant financial relationships.
Diwanshu Soni, DO, Bhupinder Kaur, MD, Phoebe Newell, MD, Yasmin Alishahi, MD. P0741 - The Dark Side of Upper GI Bleeding: Acute Esophageal Necrosis in a Patient With Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
