Sunday Poster Session
Category: Esophagus
P0736 - Diagnostic and Therapeutic Role of Endoscopic Submucosal Dissection in Extensive Esophageal Leukoplakia
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Amro Altarawneh, MD
Marshall University Joan C. Edwards School of Medicine
Huntington, WV
Presenting Author(s)
Yasmeen Obeidat, MD, Amro Altarawneh, MD, Buaisha Haitam, MD, Wesam Frandah, MD
Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction:
Esophageal leukoplakia (epidermoid metaplasia) is a rare mucosal disorder characterized by white plaques with a potential risk for malignant transformation. Management guidelines are not standardized, but endoscopic submucosal dissection (ESD) has emerged as an effective tool for definitive treatment and accurate histologic assessment.
Case Description/
Methods:
A 63-year-old woman with a history of coronary artery disease, COPD, and chronic gastroesophageal reflux disease presented with dysphagia and significant weight loss. Esophagogastroduodenoscopy (EGD) revealed circumferential severe mucosal alterations in the lower third of the esophagus (28–34 cm from incisors), characterized by granularity, scalloping, altered texture, and decreased vascular pattern. Enhanced visualization techniques including zoom magnification, white-light endoscopy, narrow-band imaging, and Lugol’s iodine solution 2% was applied into the esophagus, and after 2 minutes, a diffuse circumferential area of no uptake was noted between 28 and 34 cm from the incisors. Pathology demonstrated squamous epithelium with orthokeratosis and hypergranulosis, consistent with epidermoid metaplasia.
Due to persistent symptoms and endoscopic suspicion of potential malignancy, the patient underwent ESD for definitive diagnostic and therapeutic purposes. A circumferential lesion measuring 10 x 10 cm was successfully resected en bloc without immediate complications. Pathology results from the ESD specimen are currently pending and will be updated upon availability.
Discussion: This case highlights the diagnostic challenge posed by extensive esophageal leukoplakia and emphasizes the role of ESD in managing extensive lesions. The procedure provided a definitive histopathological diagnosis and symptom relief, supporting the consideration of ESD as a primary therapeutic option in extensive or suspicious cases. Furthermore, ESD may uncover deeper invasions or hidden pathology that could be missed on superficial biopsy or other diagnostic modalities.
Endoscopic submucosal dissection is an effective and safe modality for managing extensive esophageal leukoplakia, offering both diagnostic accuracy and therapeutic benefit. Further studies and standardized guidelines are necessary to optimize the management of this rare condition.
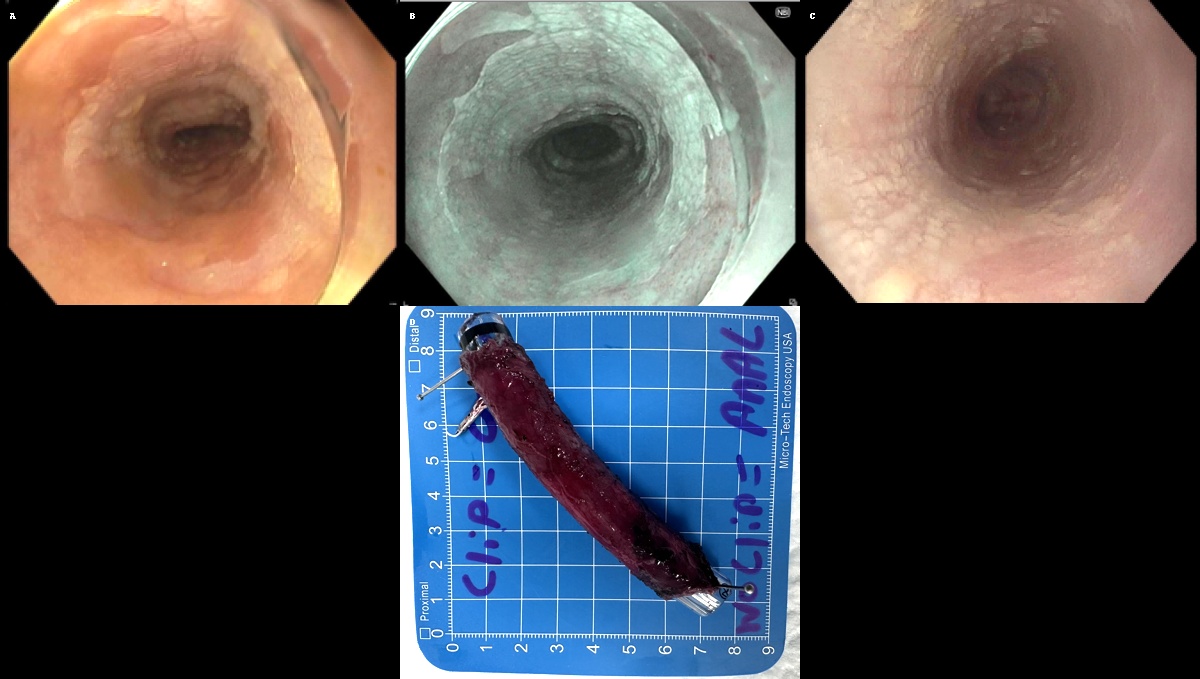
Figure: A: Application of Lugol’s iodine solution revealing a diffuse unstained lesion spanning from 28–34 cm from the incisors, indicative of esophageal leukoplakia.
B: Enhanced visualization using narrow-band imaging (NBI), highlighting extensive mucosal changes consistent with leukoplakia.
C: Endoscopic view demonstrating circumferential severe mucosal alterations characterized by granularity, scalloping, altered texture, and decreased vascular pattern in the lower esophagus.
D: Gross pathology of the resected specimen demonstrating a uniform, en bloc resection of the esophageal leukoplakia lesion.
Disclosures:
Yasmeen Obeidat indicated no relevant financial relationships.
Amro Altarawneh indicated no relevant financial relationships.
Buaisha Haitam indicated no relevant financial relationships.
Wesam Frandah: Boston Scientific – Advisor or Review Panel Member, Consultant. Merritt – Consultant. Olympus corporation of America – Consultant.
Yasmeen Obeidat, MD, Amro Altarawneh, MD, Buaisha Haitam, MD, Wesam Frandah, MD. P0736 - Diagnostic and Therapeutic Role of Endoscopic Submucosal Dissection in Extensive Esophageal Leukoplakia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Marshall University Joan C. Edwards School of Medicine, Huntington, WV
Introduction:
Esophageal leukoplakia (epidermoid metaplasia) is a rare mucosal disorder characterized by white plaques with a potential risk for malignant transformation. Management guidelines are not standardized, but endoscopic submucosal dissection (ESD) has emerged as an effective tool for definitive treatment and accurate histologic assessment.
Case Description/
Methods:
A 63-year-old woman with a history of coronary artery disease, COPD, and chronic gastroesophageal reflux disease presented with dysphagia and significant weight loss. Esophagogastroduodenoscopy (EGD) revealed circumferential severe mucosal alterations in the lower third of the esophagus (28–34 cm from incisors), characterized by granularity, scalloping, altered texture, and decreased vascular pattern. Enhanced visualization techniques including zoom magnification, white-light endoscopy, narrow-band imaging, and Lugol’s iodine solution 2% was applied into the esophagus, and after 2 minutes, a diffuse circumferential area of no uptake was noted between 28 and 34 cm from the incisors. Pathology demonstrated squamous epithelium with orthokeratosis and hypergranulosis, consistent with epidermoid metaplasia.
Due to persistent symptoms and endoscopic suspicion of potential malignancy, the patient underwent ESD for definitive diagnostic and therapeutic purposes. A circumferential lesion measuring 10 x 10 cm was successfully resected en bloc without immediate complications. Pathology results from the ESD specimen are currently pending and will be updated upon availability.
Discussion: This case highlights the diagnostic challenge posed by extensive esophageal leukoplakia and emphasizes the role of ESD in managing extensive lesions. The procedure provided a definitive histopathological diagnosis and symptom relief, supporting the consideration of ESD as a primary therapeutic option in extensive or suspicious cases. Furthermore, ESD may uncover deeper invasions or hidden pathology that could be missed on superficial biopsy or other diagnostic modalities.
Endoscopic submucosal dissection is an effective and safe modality for managing extensive esophageal leukoplakia, offering both diagnostic accuracy and therapeutic benefit. Further studies and standardized guidelines are necessary to optimize the management of this rare condition.
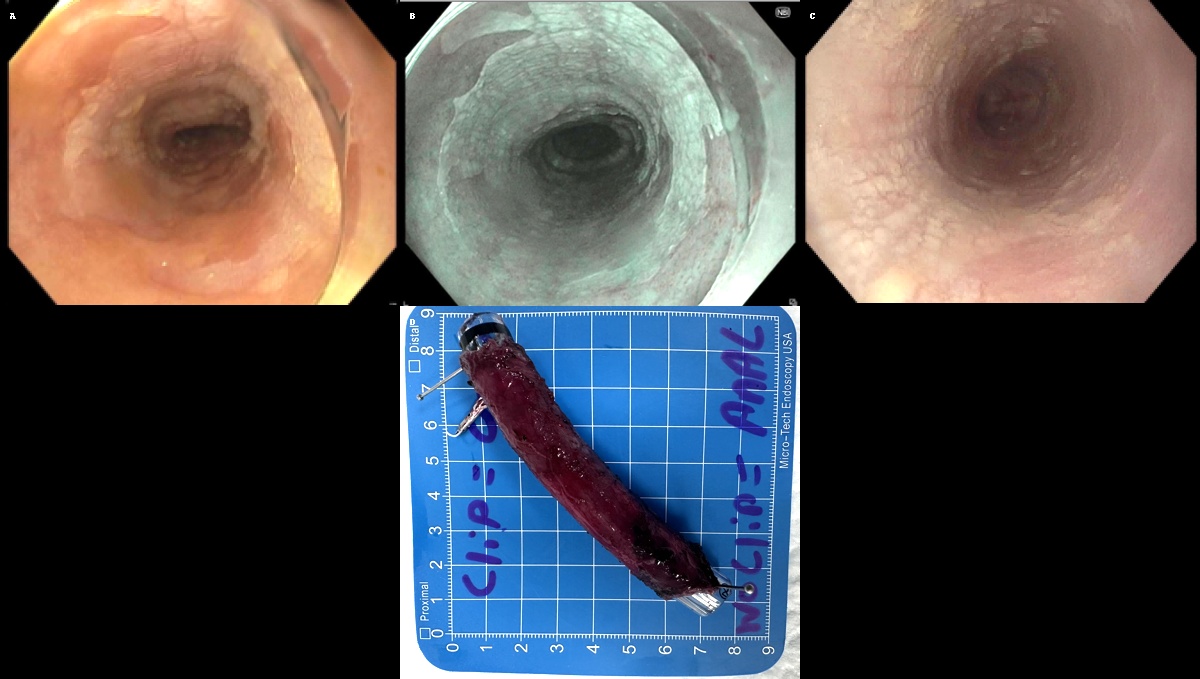
Figure: A: Application of Lugol’s iodine solution revealing a diffuse unstained lesion spanning from 28–34 cm from the incisors, indicative of esophageal leukoplakia.
B: Enhanced visualization using narrow-band imaging (NBI), highlighting extensive mucosal changes consistent with leukoplakia.
C: Endoscopic view demonstrating circumferential severe mucosal alterations characterized by granularity, scalloping, altered texture, and decreased vascular pattern in the lower esophagus.
D: Gross pathology of the resected specimen demonstrating a uniform, en bloc resection of the esophageal leukoplakia lesion.
Disclosures:
Yasmeen Obeidat indicated no relevant financial relationships.
Amro Altarawneh indicated no relevant financial relationships.
Buaisha Haitam indicated no relevant financial relationships.
Wesam Frandah: Boston Scientific – Advisor or Review Panel Member, Consultant. Merritt – Consultant. Olympus corporation of America – Consultant.
Yasmeen Obeidat, MD, Amro Altarawneh, MD, Buaisha Haitam, MD, Wesam Frandah, MD. P0736 - Diagnostic and Therapeutic Role of Endoscopic Submucosal Dissection in Extensive Esophageal Leukoplakia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
