Sunday Poster Session
Category: Esophagus
P0735 - An Uncommon Cause of Esophageal Perforation in a Patient with Chronic Pancreatitis
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- MP
Mark Peicher, DO
University of New Mexico Hospital
Albuquerque, NM
Presenting Author(s)
Mark Peicher, DO, Amal Shine, MD
University of New Mexico Hospital, Albuquerque, NM
Introduction: Esophageal perforation is a rare but life-threatening condition with high morbidity and mortality, especially when diagnosis is delayed. While iatrogenic causes account for ~60% of cases, spontaneous rupture from emesis (Boerhaave syndrome) comprises only 10–15%. We present a rare case of spontaneous perforation secondary to vomiting from chronic gastric outlet obstruction (GOO) due to chronic pancreatitis.
Case Description/
Methods: A 58-year-old man with alcohol use disorder and chronic pancreatitis, complicated by partial GOO and biliary stricture with prior CBD stenting, presented with acute-onset back pain and 3 episodes of hematemesis. Vitals showed tachycardia; labs revealed WBC 17.0, hemoglobin 12.9 (baseline 14), and platelets 461; CMP and lactate were normal.
CT chest/abdomen/pelvis showed diffuse esophageal thickening and edema suggestive of esophagitis, pneumomediastinum concerning for perforation, and a distended stomach suggestive of GOO.
The patient was intubated and underwent emergent left VATS with washout and endoscopic stent placement. EGD revealed diffuse esophageal necrosis with black mucosa and a 30 mm perforation above the gastroesophageal junction. A 23x70 mm fully covered metal stent was placed and secured with an over-the-scope clip. Follow-up esophagram showed no leak.
Repeat EGD one week later showed mucosal healing after PPI therapy, with the stent in good position. To treat the GOO, EUS-guided gastrojejunostomy with a 20x10 mm AXIOS stent was performed.
The patient had an uncomplicated hospital course, received broad-spectrum antibiotics and antifungals, and was discharged on oral fluconazole and amoxicillin-clavulanate. He tolerated a stent diet and was scheduled for stent removal 3 months post-discharge.
Discussion: Esophageal perforation is a critical diagnosis with an estimated incidence of 3.1 per million annually. Causes include iatrogenic injury (59–75%), spontaneous rupture, trauma, or foreign body ingestion. Mortality can exceed 20–40%, particularly with delayed intervention.
In this case, persistent vomiting from chronic GOO likely caused a sudden increase in intraluminal pressure, resulting in perforation. This rare mechanism underscores the importance of considering esophageal perforation in patients with obstructive GI symptoms presenting with back or chest pain. Rapid multidisciplinary intervention was crucial to survival.
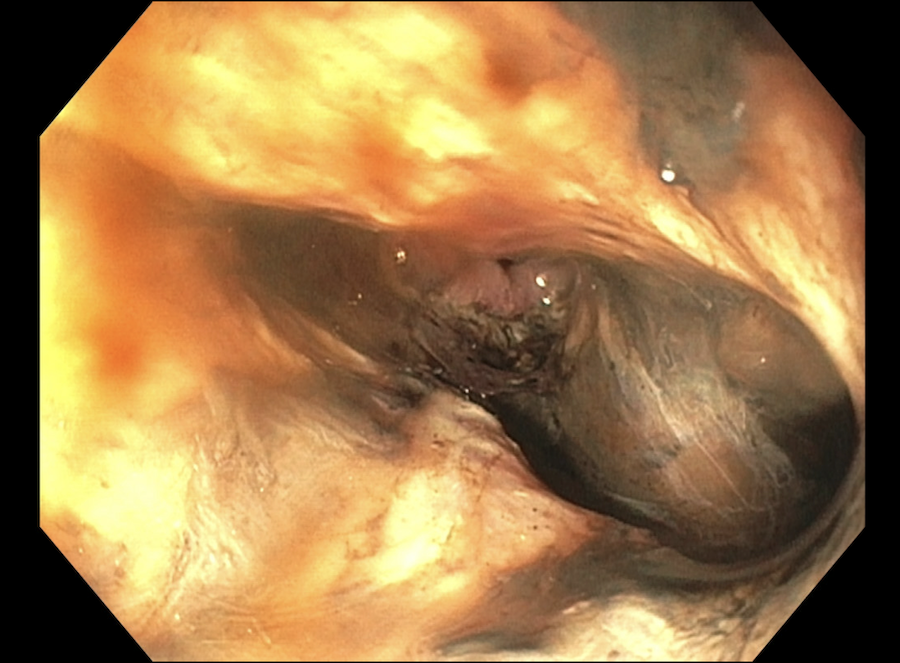
Figure: Esophageal Perforation
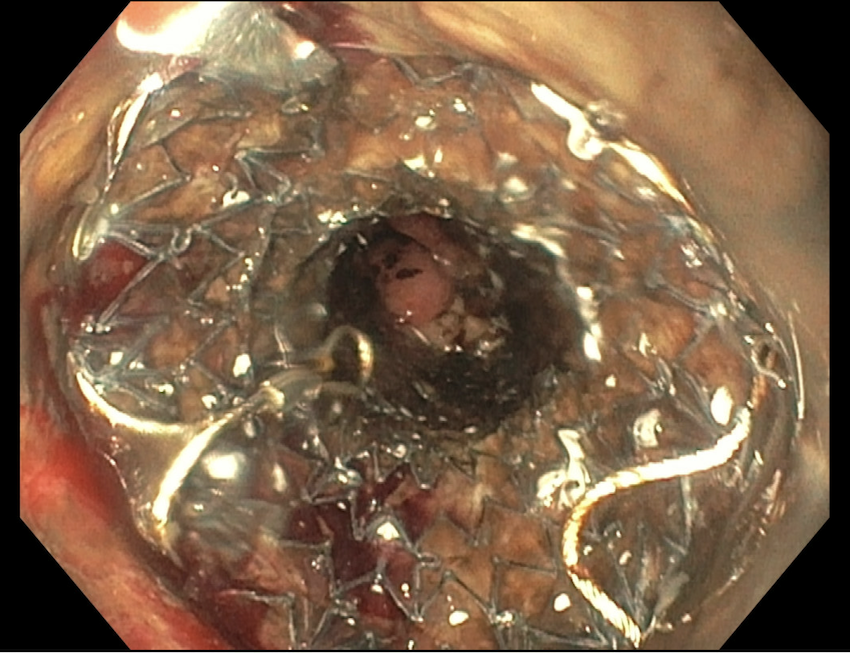
Figure: Fully covered metal stent placement
Disclosures:
Mark Peicher indicated no relevant financial relationships.
Amal Shine indicated no relevant financial relationships.
Mark Peicher, DO, Amal Shine, MD. P0735 - An Uncommon Cause of Esophageal Perforation in a Patient with Chronic Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of New Mexico Hospital, Albuquerque, NM
Introduction: Esophageal perforation is a rare but life-threatening condition with high morbidity and mortality, especially when diagnosis is delayed. While iatrogenic causes account for ~60% of cases, spontaneous rupture from emesis (Boerhaave syndrome) comprises only 10–15%. We present a rare case of spontaneous perforation secondary to vomiting from chronic gastric outlet obstruction (GOO) due to chronic pancreatitis.
Case Description/
Methods: A 58-year-old man with alcohol use disorder and chronic pancreatitis, complicated by partial GOO and biliary stricture with prior CBD stenting, presented with acute-onset back pain and 3 episodes of hematemesis. Vitals showed tachycardia; labs revealed WBC 17.0, hemoglobin 12.9 (baseline 14), and platelets 461; CMP and lactate were normal.
CT chest/abdomen/pelvis showed diffuse esophageal thickening and edema suggestive of esophagitis, pneumomediastinum concerning for perforation, and a distended stomach suggestive of GOO.
The patient was intubated and underwent emergent left VATS with washout and endoscopic stent placement. EGD revealed diffuse esophageal necrosis with black mucosa and a 30 mm perforation above the gastroesophageal junction. A 23x70 mm fully covered metal stent was placed and secured with an over-the-scope clip. Follow-up esophagram showed no leak.
Repeat EGD one week later showed mucosal healing after PPI therapy, with the stent in good position. To treat the GOO, EUS-guided gastrojejunostomy with a 20x10 mm AXIOS stent was performed.
The patient had an uncomplicated hospital course, received broad-spectrum antibiotics and antifungals, and was discharged on oral fluconazole and amoxicillin-clavulanate. He tolerated a stent diet and was scheduled for stent removal 3 months post-discharge.
Discussion: Esophageal perforation is a critical diagnosis with an estimated incidence of 3.1 per million annually. Causes include iatrogenic injury (59–75%), spontaneous rupture, trauma, or foreign body ingestion. Mortality can exceed 20–40%, particularly with delayed intervention.
In this case, persistent vomiting from chronic GOO likely caused a sudden increase in intraluminal pressure, resulting in perforation. This rare mechanism underscores the importance of considering esophageal perforation in patients with obstructive GI symptoms presenting with back or chest pain. Rapid multidisciplinary intervention was crucial to survival.
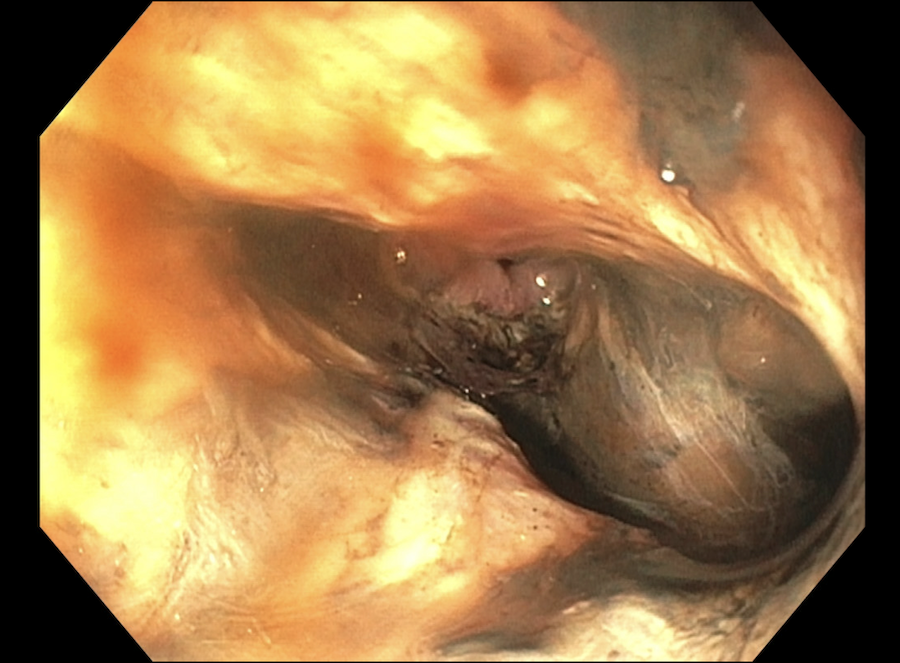
Figure: Esophageal Perforation
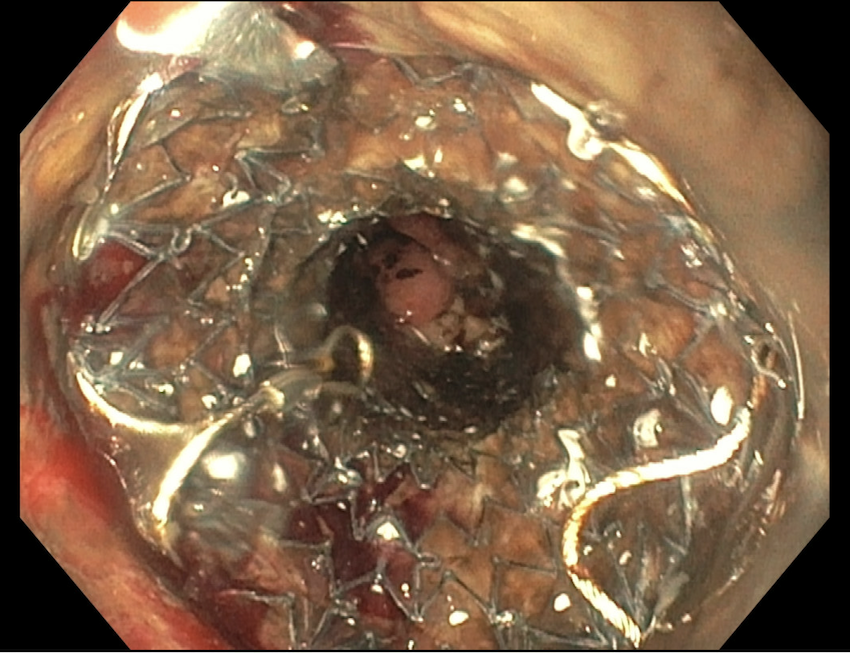
Figure: Fully covered metal stent placement
Disclosures:
Mark Peicher indicated no relevant financial relationships.
Amal Shine indicated no relevant financial relationships.
Mark Peicher, DO, Amal Shine, MD. P0735 - An Uncommon Cause of Esophageal Perforation in a Patient with Chronic Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
