Sunday Poster Session
Category: Esophagus
P0733 - Dysphagia Aortica: A Rare Cause of Dysphagia
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Ahmed abdelwahed, MBBCh
University of Connecticut Health Center
Farmington, CT
Presenting Author(s)
Ahmed Abdelwahed, MBBCh1, Mayra Sanchez, MD2, Amir Masoud, MD3
1University of Connecticut Health Center, Farmington, CT; 2Hartford HealthCare's Neurogastroenterology and Motility Center, Fairfield, CT; 3Hartford Healthcare/Connecticut GI, Fairfield, CT
Introduction: Dysphagia is a relatively common complaint among adults, particularly in adults over the age of 50, with a reported prevalence of approximately 7–10% in this population. One rare cause is dysphagia aortica, which results from external compression of the esophagus by a dilated, tortuous, or aneurysmal aorta. This condition is often underrecognized. Hence, we present a case of dysphagia secondary to a dilated aorta, occurring shortly after graft repair, to highlight this uncommon etiology.
Case Description/
Methods: We present a 75-year-old female with a past medical history of multiple saccular aneurysms, hypertension, peripheral artery disease, and coronary artery disease, who presented with dysphagia and frequent aspirations after undergoing ascending aortic arch repair with graft insertion. The patient reported that she could not belch and had difficulty getting food down. She also experienced severe epigastric abdominal pain lasting for about 20 minutes after meals. She was initially referred to ENT and underwent flexible laryngoscopy, which revealed reduced vocal cord function; however, this did not explain the cause of her dysphagia. She was referred for an esophagram, which showed delayed emptying into the stomach, raising concern for esophageal dysmotility. She was then seen in the gastroenterology motility center, where further review of her esophagram and chest CT revealed clear impingement of the distal esophagus by the dilated aorta. The patient elected to undergo upper endoscopy with dilation; however, the extrinsic compression was not amenable to endoscopic intervention, given patient's frailty.
Discussion: Dysphagia aortica is more common in older patients, those with hypertension, kyphosis, and women of short stature. It is often an under-recognized condition, and a high index of suspicion is necessary to establish the diagnosis. There is no established gold standard for diagnosis; however, an esophageal barium swallow can be useful. Video fluoroscopic swallowing studies and chest CT can also aid in diagnosis. Upper endoscopy plays an important role in ruling out other causes of dysphagia.
Treatment is mainly conservative, as patients typically have multiple chronic comorbidities. Conservative management includes dietary modification and addressing the underlying cause of aortic dilation, such as controlling hypertension, to prevent progression. Surgical options may include esophageal dilation with stent placement or percutaneous endoscopic gastrostomy.
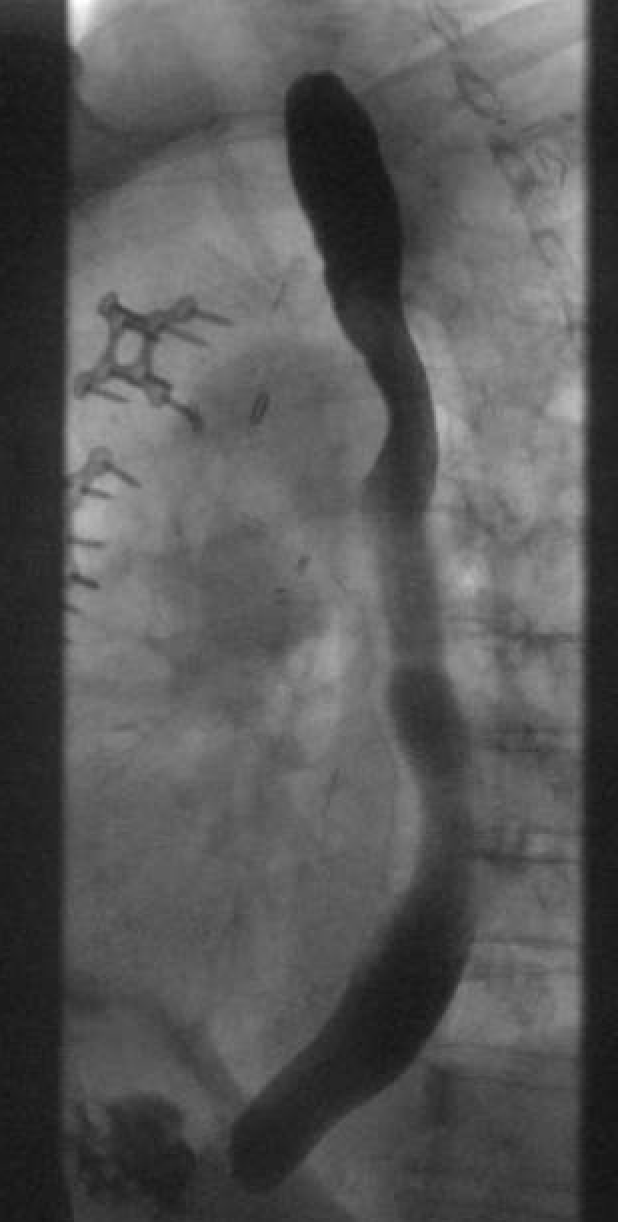
Figure: Esophagram showing impingement of the distal esophagus

Figure: A sagittal view of CT chest showing compression by aorta on distal esophagus
Disclosures:
Ahmed Abdelwahed indicated no relevant financial relationships.
Mayra Sanchez indicated no relevant financial relationships.
Amir Masoud indicated no relevant financial relationships.
Ahmed Abdelwahed, MBBCh1, Mayra Sanchez, MD2, Amir Masoud, MD3. P0733 - Dysphagia Aortica: A Rare Cause of Dysphagia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health Center, Farmington, CT; 2Hartford HealthCare's Neurogastroenterology and Motility Center, Fairfield, CT; 3Hartford Healthcare/Connecticut GI, Fairfield, CT
Introduction: Dysphagia is a relatively common complaint among adults, particularly in adults over the age of 50, with a reported prevalence of approximately 7–10% in this population. One rare cause is dysphagia aortica, which results from external compression of the esophagus by a dilated, tortuous, or aneurysmal aorta. This condition is often underrecognized. Hence, we present a case of dysphagia secondary to a dilated aorta, occurring shortly after graft repair, to highlight this uncommon etiology.
Case Description/
Methods: We present a 75-year-old female with a past medical history of multiple saccular aneurysms, hypertension, peripheral artery disease, and coronary artery disease, who presented with dysphagia and frequent aspirations after undergoing ascending aortic arch repair with graft insertion. The patient reported that she could not belch and had difficulty getting food down. She also experienced severe epigastric abdominal pain lasting for about 20 minutes after meals. She was initially referred to ENT and underwent flexible laryngoscopy, which revealed reduced vocal cord function; however, this did not explain the cause of her dysphagia. She was referred for an esophagram, which showed delayed emptying into the stomach, raising concern for esophageal dysmotility. She was then seen in the gastroenterology motility center, where further review of her esophagram and chest CT revealed clear impingement of the distal esophagus by the dilated aorta. The patient elected to undergo upper endoscopy with dilation; however, the extrinsic compression was not amenable to endoscopic intervention, given patient's frailty.
Discussion: Dysphagia aortica is more common in older patients, those with hypertension, kyphosis, and women of short stature. It is often an under-recognized condition, and a high index of suspicion is necessary to establish the diagnosis. There is no established gold standard for diagnosis; however, an esophageal barium swallow can be useful. Video fluoroscopic swallowing studies and chest CT can also aid in diagnosis. Upper endoscopy plays an important role in ruling out other causes of dysphagia.
Treatment is mainly conservative, as patients typically have multiple chronic comorbidities. Conservative management includes dietary modification and addressing the underlying cause of aortic dilation, such as controlling hypertension, to prevent progression. Surgical options may include esophageal dilation with stent placement or percutaneous endoscopic gastrostomy.
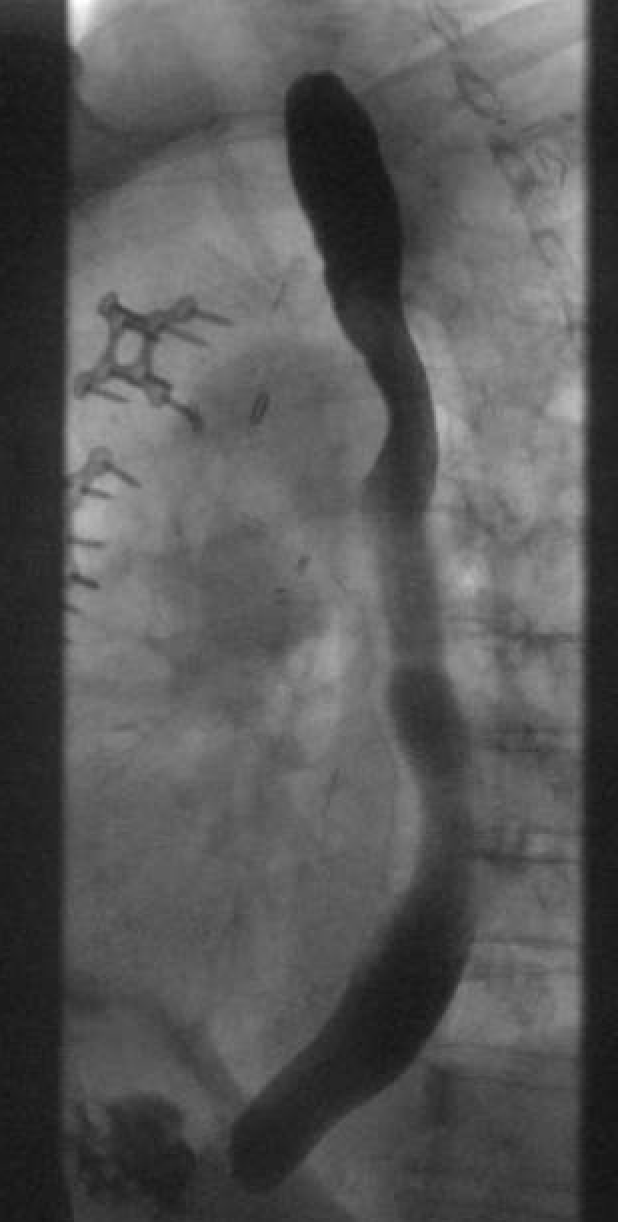
Figure: Esophagram showing impingement of the distal esophagus

Figure: A sagittal view of CT chest showing compression by aorta on distal esophagus
Disclosures:
Ahmed Abdelwahed indicated no relevant financial relationships.
Mayra Sanchez indicated no relevant financial relationships.
Amir Masoud indicated no relevant financial relationships.
Ahmed Abdelwahed, MBBCh1, Mayra Sanchez, MD2, Amir Masoud, MD3. P0733 - Dysphagia Aortica: A Rare Cause of Dysphagia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
