Sunday Poster Session
Category: Esophagus
P0732 - Histological Heterogeneity in Malignancy: Coexisting Squamous Cell Carcinoma and Adenocarcinoma of the Esophagus in a Single Patient
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Tarah Magloire, MD (she/her/hers)
SUNY Downstate Medical Center
Brooklyn, NY
Presenting Author(s)
Tarah Magloire, MD1, Kevin Han, MD2, Rebhi Rabah, MD3, Qi Yu, MD4
1SUNY Downstate Medical Center, Brooklyn, NY; 2SUNY Downstate Health Sciences University, New York, NY; 3SUNY Downstate Health Sciences University, Brooklyn, NY; 4SUNY Downstate, Brooklyn, NY
Introduction: Esophageal adenosquamous carcinoma (ASC) is a rare tumor with histopathologic characteristics of both adenocarcinoma (AC) and squamous cell carcinoma (SCC). ASC remains extremely rare with low estimated incidence rates. We present the case of an 81-year-old African American male with imaging showing esophageal mass and biopsy revealing both AC and SCC.
Case Description/
Methods: An 81-year-old male presented with 1 month history of dysphagia to both solids and liquid along with a 30 lbs weight loss, worsening nausea, and abdominal pain. Physical exam was notable for right upper quadrant and epigastric tenderness. CT imaging showed left chest wall lymphadenopathy up to 2.3 cm; diffuse circumferential distal esophageal wall thickening concerning for esophageal carcinoma and innumerable hypodense hepatic lesions. EGD revealed a partially obstructing large fungating mass in the lower third of the esophagus 45 cm from incisors (consistent with Siewert type I lesion) which was biopsied. Ultra slim endoscope was used to traverse the esophagus; a single large subepithelial nodule was also found in the duodenal bulb and was biopsied. Pathology results revealed poorly differentiated esophageal carcinoma with features of both AC and SCC. Liver biopsy showed similar features. Repeat imaging 3 weeks later showed rapid progression of esophageal mass, increase in size of the liver lesions, new development of perihepatic ascites and peritoneal carcinomatosis. The patient had a rapid decline and passed from multi-organ failure.
Discussion: ASC differs from single-type esophageal cancers in both biological behavior and treatment response. Some studies have suggested that ASC may arise from esophageal glands or ductal cells, while others believe that ASC first develops into SCC then eventually glandular differentiation occurs. EGD with biopsy is the cornerstone for diagnosis. However, there is a high rate of misdiagnosis from superficial tissue biopsies. A few case series have found a lower median survival time for ASC compared to SCC. In our case, the patient deteriorated rapidly, highlighting that ASC tends to be more aggressive with poor clinical outcomes. No targeted therapy has been established and surgical resection with neoadjuvant chemoradiotherapy for locally advanced disease is the mainstay of treatment. Our case highlights the need for further research with a multidisciplinary approach involving gastroenterologist, oncologists and pathologist in order to improve outcomes.
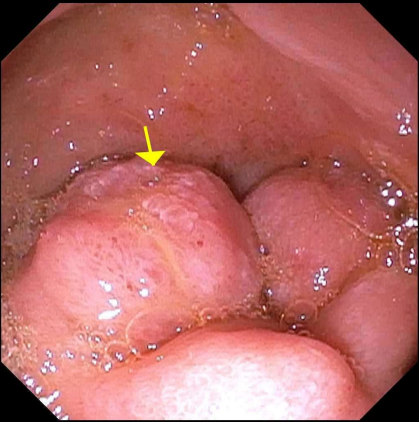
Figure: Partially obstructing mass located at the lower third of the esophagus on EGD (arrows indicating the mass and the endoscope)

Figure: Duodenal bulb nodule found on EGD
Disclosures:
Tarah Magloire indicated no relevant financial relationships.
Kevin Han indicated no relevant financial relationships.
Rebhi Rabah indicated no relevant financial relationships.
Qi Yu indicated no relevant financial relationships.
Tarah Magloire, MD1, Kevin Han, MD2, Rebhi Rabah, MD3, Qi Yu, MD4. P0732 - Histological Heterogeneity in Malignancy: Coexisting Squamous Cell Carcinoma and Adenocarcinoma of the Esophagus in a Single Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Downstate Medical Center, Brooklyn, NY; 2SUNY Downstate Health Sciences University, New York, NY; 3SUNY Downstate Health Sciences University, Brooklyn, NY; 4SUNY Downstate, Brooklyn, NY
Introduction: Esophageal adenosquamous carcinoma (ASC) is a rare tumor with histopathologic characteristics of both adenocarcinoma (AC) and squamous cell carcinoma (SCC). ASC remains extremely rare with low estimated incidence rates. We present the case of an 81-year-old African American male with imaging showing esophageal mass and biopsy revealing both AC and SCC.
Case Description/
Methods: An 81-year-old male presented with 1 month history of dysphagia to both solids and liquid along with a 30 lbs weight loss, worsening nausea, and abdominal pain. Physical exam was notable for right upper quadrant and epigastric tenderness. CT imaging showed left chest wall lymphadenopathy up to 2.3 cm; diffuse circumferential distal esophageal wall thickening concerning for esophageal carcinoma and innumerable hypodense hepatic lesions. EGD revealed a partially obstructing large fungating mass in the lower third of the esophagus 45 cm from incisors (consistent with Siewert type I lesion) which was biopsied. Ultra slim endoscope was used to traverse the esophagus; a single large subepithelial nodule was also found in the duodenal bulb and was biopsied. Pathology results revealed poorly differentiated esophageal carcinoma with features of both AC and SCC. Liver biopsy showed similar features. Repeat imaging 3 weeks later showed rapid progression of esophageal mass, increase in size of the liver lesions, new development of perihepatic ascites and peritoneal carcinomatosis. The patient had a rapid decline and passed from multi-organ failure.
Discussion: ASC differs from single-type esophageal cancers in both biological behavior and treatment response. Some studies have suggested that ASC may arise from esophageal glands or ductal cells, while others believe that ASC first develops into SCC then eventually glandular differentiation occurs. EGD with biopsy is the cornerstone for diagnosis. However, there is a high rate of misdiagnosis from superficial tissue biopsies. A few case series have found a lower median survival time for ASC compared to SCC. In our case, the patient deteriorated rapidly, highlighting that ASC tends to be more aggressive with poor clinical outcomes. No targeted therapy has been established and surgical resection with neoadjuvant chemoradiotherapy for locally advanced disease is the mainstay of treatment. Our case highlights the need for further research with a multidisciplinary approach involving gastroenterologist, oncologists and pathologist in order to improve outcomes.
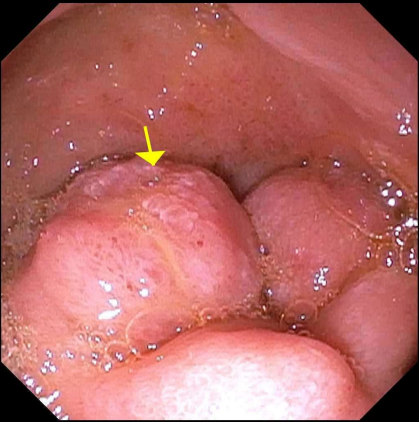
Figure: Partially obstructing mass located at the lower third of the esophagus on EGD (arrows indicating the mass and the endoscope)

Figure: Duodenal bulb nodule found on EGD
Disclosures:
Tarah Magloire indicated no relevant financial relationships.
Kevin Han indicated no relevant financial relationships.
Rebhi Rabah indicated no relevant financial relationships.
Qi Yu indicated no relevant financial relationships.
Tarah Magloire, MD1, Kevin Han, MD2, Rebhi Rabah, MD3, Qi Yu, MD4. P0732 - Histological Heterogeneity in Malignancy: Coexisting Squamous Cell Carcinoma and Adenocarcinoma of the Esophagus in a Single Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
