Sunday Poster Session
Category: Esophagus
P0727 - Superior Mesenteric Artery (SMA) Syndrome After Colectomy: A Complex Postoperative Obstruction
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Bianca Thakkar, DO
University of Connecticut Health
Farmington, CT
Presenting Author(s)
Bianca Thakkar, DO1, Rachael Hagen, DO1, Minh Thu T.. Nguyen, MD2, Amir Masoud, MD3
1University of Connecticut Health, Farmington, CT; 2University of Connecticut, Farmington, CT; 3Hartford Healthcare/Connecticut GI, Fairfield, CT
Introduction: Superior mesenteric artery (SMA) syndrome is a rare cause of proximal small bowel obstruction (SBO) due to compression of the third portion of the duodenum between the SMA and aorta. It typically results from rapid or significant weight loss reducing the mesenteric fat pad that maintains the normal aortomesenteric angle (38–65°). When this angle narrows to less than 25°, duodenal compression may occur. SMA syndrome affects about 0.013% to 0.3% of the population and is associated with catabolic states, major abdominal surgery, eating disorders, or chronic illness. Symptoms include postprandial epigastric pain, nausea, vomiting, early satiety, and weight loss. Diagnosis is confirmed by CT or MR angiography demonstrating a narrowed aortomesenteric angle and duodenal compression. Management typically includes nutritional rehabilitation; surgery (e.g., duodenojejunostomy) is reserved for refractory cases.
Case Description/
Methods: A 39-year-old woman with colonic dysmotility, Ehlers-Danlos syndrome, and pancreatic insufficiency presented with postprandial abdominal distention and severe back-radiating pain after meals. The prior year, she had a total abdominal colectomy with ileorectal anastomosis complicated by SBO from an internal hernia requiring laparotomy. Postoperatively, she experienced poor oral intake and transitioned from total parenteral nutrition to IV fluids due to hypertriglyceridemia and hyperglycemia. She had lost approximately 8 lbs over the past year.
On presentation, vital signs were stable and labs were unremarkable. CT abdomen/pelvis revealed a distended stomach and proximal duodenum, with compression of the third portion of the duodenum between the SMA and aorta—consistent with SMA syndrome. Small bowel loops measuring up to 3.7 cm suggested a partial obstruction. Surgery recommended nasogastric decompression followed by a Gastrografin challenge, although the patient requested to follow up outpatient after decompression.
Discussion: This case highlights SMA syndrome in a patient with a connective tissue disorder and chronic malnutrition, including loss of retroperitoneal fat post-surgery. Nutritional support is the cornerstone of therapy. If unsuccessful, surgical options like duodenojejunostomy or Strong’s procedure may be considered. Vigilance is key in recognizing SMA syndrome, particularly postoperatively with rapid weight loss. Though rare, it remains a critical cause of SBO in high-risk patients.
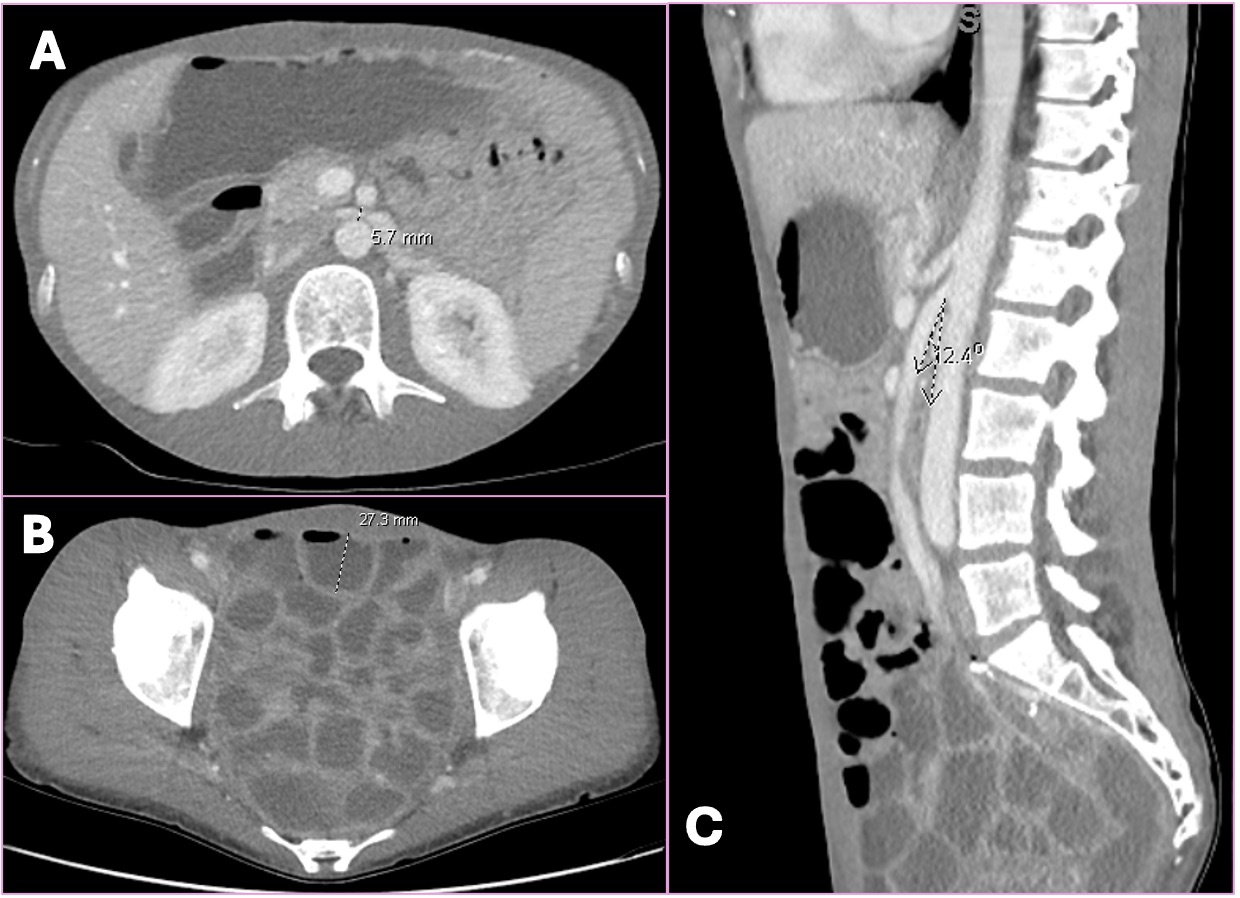
Figure: Figure 1. CT Abdomen/Pelvis without contrast
A. The distance between the aorta and the SMA measured at 5.7mm, from a normal distance of 10-34 mm.
B. Ileorectal anastomosis within the pelvis with extensive fluid-filled loops of small bowel that measure up to 3.7 cm in diameter.
C. The aortomesenteric angle, which is normally 28-65 degrees, is measured at 12.4 degrees, consistent with SMA syndrome.
Disclosures:
Bianca Thakkar indicated no relevant financial relationships.
Rachael Hagen indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Amir Masoud indicated no relevant financial relationships.
Bianca Thakkar, DO1, Rachael Hagen, DO1, Minh Thu T.. Nguyen, MD2, Amir Masoud, MD3. P0727 - Superior Mesenteric Artery (SMA) Syndrome After Colectomy: A Complex Postoperative Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Connecticut Health, Farmington, CT; 2University of Connecticut, Farmington, CT; 3Hartford Healthcare/Connecticut GI, Fairfield, CT
Introduction: Superior mesenteric artery (SMA) syndrome is a rare cause of proximal small bowel obstruction (SBO) due to compression of the third portion of the duodenum between the SMA and aorta. It typically results from rapid or significant weight loss reducing the mesenteric fat pad that maintains the normal aortomesenteric angle (38–65°). When this angle narrows to less than 25°, duodenal compression may occur. SMA syndrome affects about 0.013% to 0.3% of the population and is associated with catabolic states, major abdominal surgery, eating disorders, or chronic illness. Symptoms include postprandial epigastric pain, nausea, vomiting, early satiety, and weight loss. Diagnosis is confirmed by CT or MR angiography demonstrating a narrowed aortomesenteric angle and duodenal compression. Management typically includes nutritional rehabilitation; surgery (e.g., duodenojejunostomy) is reserved for refractory cases.
Case Description/
Methods: A 39-year-old woman with colonic dysmotility, Ehlers-Danlos syndrome, and pancreatic insufficiency presented with postprandial abdominal distention and severe back-radiating pain after meals. The prior year, she had a total abdominal colectomy with ileorectal anastomosis complicated by SBO from an internal hernia requiring laparotomy. Postoperatively, she experienced poor oral intake and transitioned from total parenteral nutrition to IV fluids due to hypertriglyceridemia and hyperglycemia. She had lost approximately 8 lbs over the past year.
On presentation, vital signs were stable and labs were unremarkable. CT abdomen/pelvis revealed a distended stomach and proximal duodenum, with compression of the third portion of the duodenum between the SMA and aorta—consistent with SMA syndrome. Small bowel loops measuring up to 3.7 cm suggested a partial obstruction. Surgery recommended nasogastric decompression followed by a Gastrografin challenge, although the patient requested to follow up outpatient after decompression.
Discussion: This case highlights SMA syndrome in a patient with a connective tissue disorder and chronic malnutrition, including loss of retroperitoneal fat post-surgery. Nutritional support is the cornerstone of therapy. If unsuccessful, surgical options like duodenojejunostomy or Strong’s procedure may be considered. Vigilance is key in recognizing SMA syndrome, particularly postoperatively with rapid weight loss. Though rare, it remains a critical cause of SBO in high-risk patients.
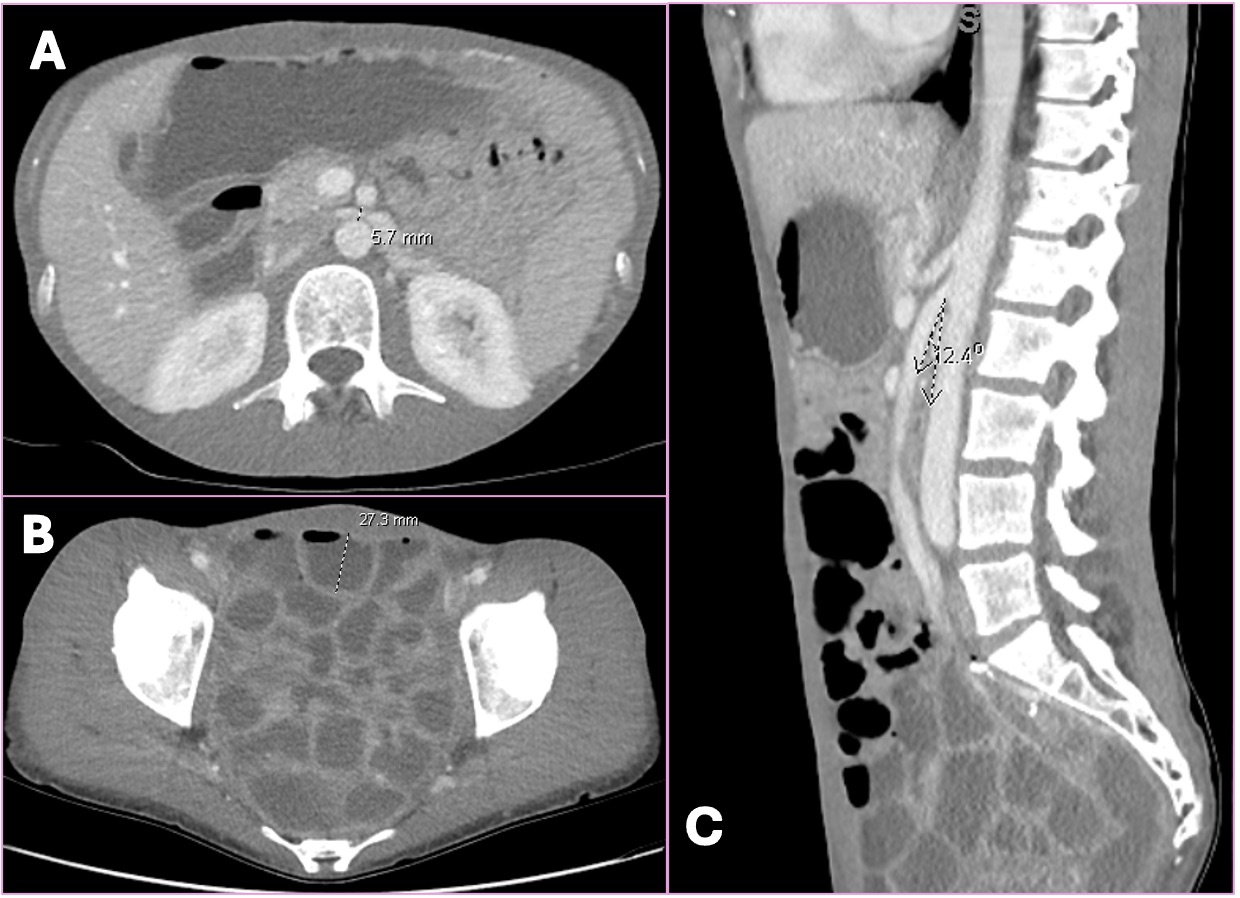
Figure: Figure 1. CT Abdomen/Pelvis without contrast
A. The distance between the aorta and the SMA measured at 5.7mm, from a normal distance of 10-34 mm.
B. Ileorectal anastomosis within the pelvis with extensive fluid-filled loops of small bowel that measure up to 3.7 cm in diameter.
C. The aortomesenteric angle, which is normally 28-65 degrees, is measured at 12.4 degrees, consistent with SMA syndrome.
Disclosures:
Bianca Thakkar indicated no relevant financial relationships.
Rachael Hagen indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Amir Masoud indicated no relevant financial relationships.
Bianca Thakkar, DO1, Rachael Hagen, DO1, Minh Thu T.. Nguyen, MD2, Amir Masoud, MD3. P0727 - Superior Mesenteric Artery (SMA) Syndrome After Colectomy: A Complex Postoperative Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
