Sunday Poster Session
Category: Esophagus
P0717 - Cutting Weight, but Losing Iron: Post-Gastric Bypass Plummer-Vinson Syndrome
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- LC
Lorraine I. Chong Tai, MD (she/her/hers)
Broward Health Medical Center
Allentown, PA
Presenting Author(s)
Lorraine Chong Tai, MD1, Haille Joseph, MBBS2
1Broward Health Medical Center, Fort Lauderdale, FL; 2Scarborough General Hospital, Signal Hill, Tobago, Trinidad and Tobago
Introduction: Plummer-Vinson syndrome (PVS) is a rare disease characterized by the triad of iron-deficiency anemia, dysphagia and esophageal webs. The condition was more commonly seen in the earlier half of the 20th century, particularly in middle-aged Scandinavian women with a rapid decline attributable to an improvement in nutritional supplementation as well as the widespread fortification of flour with iron. Our case is particularly noteworthy, not only for its rare prevalence but also for its occurrence in a patient of African American descent.
Case Description/
Methods: A 55-year-old African American female with a history of Roux-en-Y gastric bypass surgery presented to the emergency department complaints of chest pain, shortness of breath and dysphagia to solids. She endorsed weight loss of over 200 pounds since her gastric bypass surgery 18 years prior. Laboratory findings were remarkable for severe Iron Deficiency. An endoscopy showed the classic appearance of a proximal esophageal web with some other milder webs in the mid esophagus consistent with PVS (Figure 1). Gastric bypass anatomy was seen with an intact gastric pouch and a gastric jejunal anastomosis. Colonoscopy findings were unremarkable. She was subsequently discharged with instructions to begin oral iron supplementation.
Discussion: In recent literature there have only been three other reported cases of PVS after gastric bypass surgery. Iron deficiency anemia is a common post-procedural development due to reduced iron absorption, as the surgery bypasses the duodenum—the primary site of iron uptake. The exact pathogenesis of Plummer-Vinson Syndrome remains largely unknown, though several hypotheses have been proposed. One theory suggests that dysfunction in iron-dependent oxidative enzymes results in myasthenic changes in the swallowing muscles, esophageal mucosal atrophy, and subsequent web formation as an epithelial complication. It is believed that persistent epithelial injury caused by iron deficiency leads to mucosal atrophy and pharyngeal muscle degradation, ultimately contributing to the development of esophageal webs. They can be seen on barium swallow or as in our case via direct visualization on endoscopy. The initiation of iron supplementation addresses the underlying deficiency, with patients having excellent outcomes and resolution of symptoms. This case highlights the critical importance of vigilant long-term follow-up after gastric bypass surgery, as serious complications can arise even many years postoperatively.
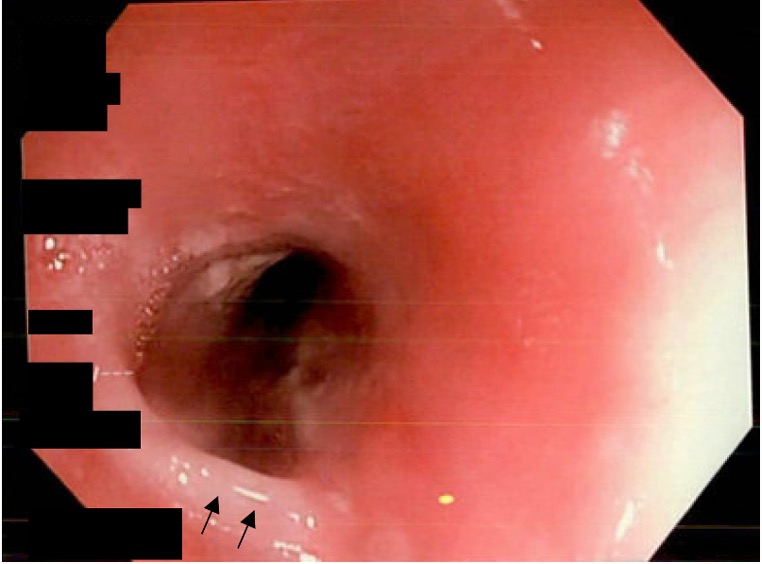
Figure: Figure 1: Proximal Esophageal web demarcated by arrows seen on endoscopy.
Disclosures:
Lorraine Chong Tai indicated no relevant financial relationships.
Haille Joseph indicated no relevant financial relationships.
Lorraine Chong Tai, MD1, Haille Joseph, MBBS2. P0717 - Cutting Weight, but Losing Iron: Post-Gastric Bypass Plummer-Vinson Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Broward Health Medical Center, Fort Lauderdale, FL; 2Scarborough General Hospital, Signal Hill, Tobago, Trinidad and Tobago
Introduction: Plummer-Vinson syndrome (PVS) is a rare disease characterized by the triad of iron-deficiency anemia, dysphagia and esophageal webs. The condition was more commonly seen in the earlier half of the 20th century, particularly in middle-aged Scandinavian women with a rapid decline attributable to an improvement in nutritional supplementation as well as the widespread fortification of flour with iron. Our case is particularly noteworthy, not only for its rare prevalence but also for its occurrence in a patient of African American descent.
Case Description/
Methods: A 55-year-old African American female with a history of Roux-en-Y gastric bypass surgery presented to the emergency department complaints of chest pain, shortness of breath and dysphagia to solids. She endorsed weight loss of over 200 pounds since her gastric bypass surgery 18 years prior. Laboratory findings were remarkable for severe Iron Deficiency. An endoscopy showed the classic appearance of a proximal esophageal web with some other milder webs in the mid esophagus consistent with PVS (Figure 1). Gastric bypass anatomy was seen with an intact gastric pouch and a gastric jejunal anastomosis. Colonoscopy findings were unremarkable. She was subsequently discharged with instructions to begin oral iron supplementation.
Discussion: In recent literature there have only been three other reported cases of PVS after gastric bypass surgery. Iron deficiency anemia is a common post-procedural development due to reduced iron absorption, as the surgery bypasses the duodenum—the primary site of iron uptake. The exact pathogenesis of Plummer-Vinson Syndrome remains largely unknown, though several hypotheses have been proposed. One theory suggests that dysfunction in iron-dependent oxidative enzymes results in myasthenic changes in the swallowing muscles, esophageal mucosal atrophy, and subsequent web formation as an epithelial complication. It is believed that persistent epithelial injury caused by iron deficiency leads to mucosal atrophy and pharyngeal muscle degradation, ultimately contributing to the development of esophageal webs. They can be seen on barium swallow or as in our case via direct visualization on endoscopy. The initiation of iron supplementation addresses the underlying deficiency, with patients having excellent outcomes and resolution of symptoms. This case highlights the critical importance of vigilant long-term follow-up after gastric bypass surgery, as serious complications can arise even many years postoperatively.
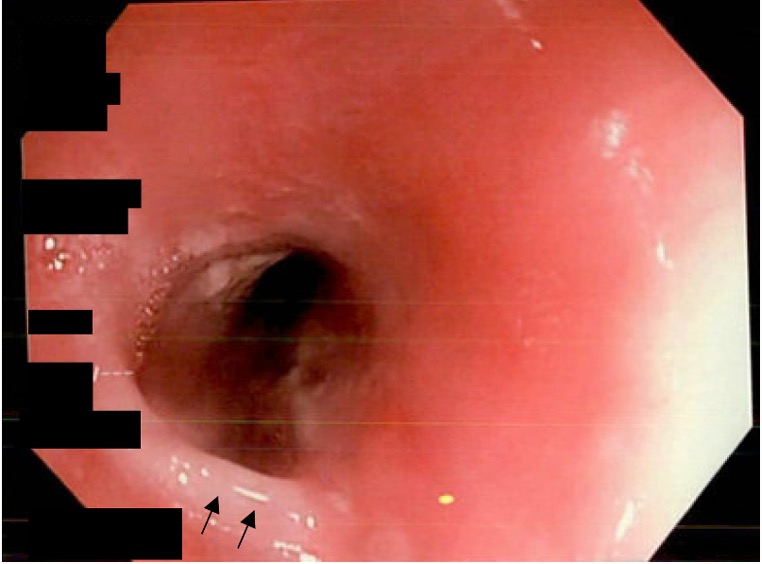
Figure: Figure 1: Proximal Esophageal web demarcated by arrows seen on endoscopy.
Disclosures:
Lorraine Chong Tai indicated no relevant financial relationships.
Haille Joseph indicated no relevant financial relationships.
Lorraine Chong Tai, MD1, Haille Joseph, MBBS2. P0717 - Cutting Weight, but Losing Iron: Post-Gastric Bypass Plummer-Vinson Syndrome, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
