Sunday Poster Session
Category: Esophagus
P0681 - Unresectable GE Junction SCC with Mid-Esophageal Extension: Diagnostic and Therapeutic Challenges
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Hamsika Moparty, MD
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Hamsika Moparty, MD1, Manasa Ginjupalli, MD2, Taranika Sarkar Das, MD3, Oleksandr Shumeiko, MD2, Amr Dokmak, MD2, Jeeva Jaganathan, MD3, Ying Xian Liu, MD2, Madhavi Reddy, MD3, Jamil Shah, MD3
1Rutgers New Jersey Medical School, Brooklyn, NY; 2Brooklyn Hospital Center, Brooklyn, NY; 3The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Squamous cell carcinoma (SCC) accounts for approximately 86% of esophageal cancers worldwide (1). Men are more commonly affected than women, with a significantly higher incidence attributed to greater exposure to tobacco and alcohol use. In contrast, most tumors at the gastroesophageal (GE) junction are adenocarcinomas, often associated with Barrett’s esophagus. Primary GE junction SCC is rare and diagnostically challenging. We present a case of GE junction SCC with synchronous mid-esophageal involvement and rapid progression in a female with a history of chronic smoking.
Case Description/
Methods: A 62-year-old female with a 40-pack-year smoking history presented with one month of progressive abdominal pain, constipation, and 15-pound unintentional weight loss. CT imaging revealed an 8.7 cm mass along the lesser curvature of the stomach with retroperitoneal lymphadenopathy. EGD demonstrated a mass involving the gastric cardia, fundus, and lesser curvature, with mid-esophageal extension; Biopsies confirmed squamous cell carcinoma. Endoscopic ultrasound showed periaortic nodal involvement, and PET-CT demonstrated metastases to the liver, mediastinum, retroperitoneum, and pancreas. Immunohistochemistry was positive for PanCK, p40, and p53. Molecular profiling showed HER2 1+, PIK3CA mutation, MSS, and low tumor mutational burden (TMB 6). The tumor was deemed unresectable due to para-aortic nodal disease and encasement of the celiac axis. Palliative chemotherapy was initiated.
Discussion: GEJ SCC is a rare but aggressive malignancy that may progress rapidly and present without classic symptoms, making early detection challenging. This case illustrates such an atypical presentation, with rapid systemic spread and minimal symptomatology. Unlike the more common GEJ adenocarcinomas, SCC generally lacks actionable molecular targets. Despite comprehensive molecular profiling, the patient was not eligible for HER2-targeted therapy or immunotherapy. While a PIK3CA mutation suggested potential for future targeted options, extensive vascular encasement and nodal involvement at presentation limited surgical management. Clinicians should maintain a high index of suspicion in high-risk individuals, such as smokers, and consider early endoscopy to improve the likelihood of identifying resectable tumors. Further research is needed to define better treatment strategies for GEJ SCC.
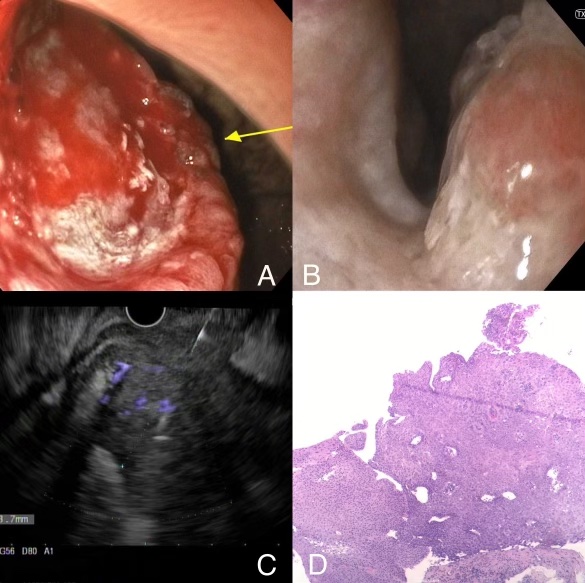
Figure: Fig 1. (A) EGD- Gastric body mass (B) EGD- Middle third Esophageal mass (C) EUS- Gastric body mass (involving mucosa) with enlarged lymph nodes (D) Esophageal mass biopsy showing invasive squamous cell carcinoma (H&E 40X).
Disclosures:
Hamsika Moparty indicated no relevant financial relationships.
Manasa Ginjupalli indicated no relevant financial relationships.
Taranika Sarkar Das indicated no relevant financial relationships.
Oleksandr Shumeiko indicated no relevant financial relationships.
Amr Dokmak indicated no relevant financial relationships.
Jeeva Jaganathan indicated no relevant financial relationships.
Ying Xian Liu indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Jamil Shah indicated no relevant financial relationships.
Hamsika Moparty, MD1, Manasa Ginjupalli, MD2, Taranika Sarkar Das, MD3, Oleksandr Shumeiko, MD2, Amr Dokmak, MD2, Jeeva Jaganathan, MD3, Ying Xian Liu, MD2, Madhavi Reddy, MD3, Jamil Shah, MD3. P0681 - Unresectable GE Junction SCC with Mid-Esophageal Extension: Diagnostic and Therapeutic Challenges, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Brooklyn, NY; 2Brooklyn Hospital Center, Brooklyn, NY; 3The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Squamous cell carcinoma (SCC) accounts for approximately 86% of esophageal cancers worldwide (1). Men are more commonly affected than women, with a significantly higher incidence attributed to greater exposure to tobacco and alcohol use. In contrast, most tumors at the gastroesophageal (GE) junction are adenocarcinomas, often associated with Barrett’s esophagus. Primary GE junction SCC is rare and diagnostically challenging. We present a case of GE junction SCC with synchronous mid-esophageal involvement and rapid progression in a female with a history of chronic smoking.
Case Description/
Methods: A 62-year-old female with a 40-pack-year smoking history presented with one month of progressive abdominal pain, constipation, and 15-pound unintentional weight loss. CT imaging revealed an 8.7 cm mass along the lesser curvature of the stomach with retroperitoneal lymphadenopathy. EGD demonstrated a mass involving the gastric cardia, fundus, and lesser curvature, with mid-esophageal extension; Biopsies confirmed squamous cell carcinoma. Endoscopic ultrasound showed periaortic nodal involvement, and PET-CT demonstrated metastases to the liver, mediastinum, retroperitoneum, and pancreas. Immunohistochemistry was positive for PanCK, p40, and p53. Molecular profiling showed HER2 1+, PIK3CA mutation, MSS, and low tumor mutational burden (TMB 6). The tumor was deemed unresectable due to para-aortic nodal disease and encasement of the celiac axis. Palliative chemotherapy was initiated.
Discussion: GEJ SCC is a rare but aggressive malignancy that may progress rapidly and present without classic symptoms, making early detection challenging. This case illustrates such an atypical presentation, with rapid systemic spread and minimal symptomatology. Unlike the more common GEJ adenocarcinomas, SCC generally lacks actionable molecular targets. Despite comprehensive molecular profiling, the patient was not eligible for HER2-targeted therapy or immunotherapy. While a PIK3CA mutation suggested potential for future targeted options, extensive vascular encasement and nodal involvement at presentation limited surgical management. Clinicians should maintain a high index of suspicion in high-risk individuals, such as smokers, and consider early endoscopy to improve the likelihood of identifying resectable tumors. Further research is needed to define better treatment strategies for GEJ SCC.
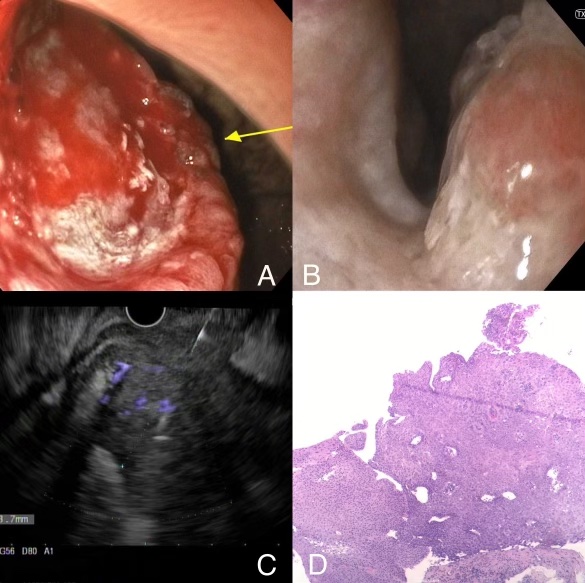
Figure: Fig 1. (A) EGD- Gastric body mass (B) EGD- Middle third Esophageal mass (C) EUS- Gastric body mass (involving mucosa) with enlarged lymph nodes (D) Esophageal mass biopsy showing invasive squamous cell carcinoma (H&E 40X).
Disclosures:
Hamsika Moparty indicated no relevant financial relationships.
Manasa Ginjupalli indicated no relevant financial relationships.
Taranika Sarkar Das indicated no relevant financial relationships.
Oleksandr Shumeiko indicated no relevant financial relationships.
Amr Dokmak indicated no relevant financial relationships.
Jeeva Jaganathan indicated no relevant financial relationships.
Ying Xian Liu indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Jamil Shah indicated no relevant financial relationships.
Hamsika Moparty, MD1, Manasa Ginjupalli, MD2, Taranika Sarkar Das, MD3, Oleksandr Shumeiko, MD2, Amr Dokmak, MD2, Jeeva Jaganathan, MD3, Ying Xian Liu, MD2, Madhavi Reddy, MD3, Jamil Shah, MD3. P0681 - Unresectable GE Junction SCC with Mid-Esophageal Extension: Diagnostic and Therapeutic Challenges, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
