Sunday Poster Session
Category: Esophagus
P0649 - Esophageal Peroral Endoscopic Myotomy or Laparoscopic Heller Myotomy Plus Dor Fundoplication for Achalasia? Real-World Evidence on GERD and Reflux Complications
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Babak Mirminachi, MD (he/him/his)
University of Pittsburgh Medical Center
Harrisburg, PA
Presenting Author(s)
Babak Mirminachi, MD1, Anas Atrash, MD1, Jake D. Fanizza, BS2, David Levinthal, MD, PhD3, Ijlal Akbar. Ali, MD4, Aylin Tansel, MD3, Sultan Mahmood, MD3
1University of Pittsburgh Medical Center, Harrisburg, PA; 2Drexel University College of Medicine, Harrisburg, PA; 3University of Pittsburgh Medical Center, Pittsburgh, PA; 4University of Oklahoma, Oklahoma City, OK
Introduction: Esophageal Peroral Endoscopic Myotomy (E-POEM) is a minimally invasive treatment for achalasia, offering an effective alternative to Laparoscopic Heller Myotomy (LHM). However, its lack of anti-reflux mechanisms like fundoplication raises concerns about reflux control. This study compares the need for repeat fundoplication, incidence of gastroesophageal reflux disease (GERD), esophagitis, and reflux-related complications in achalasia patients undergoing E-POEM versus Laparoscopic Heller Myotomy plus Dor Fundoplication (LHM+DF).
Methods: We conducted a retrospective cohort study using the U.S. multi-institutional TriNetX database to identify achalasia patients who underwent E-POEM or LHM+DF between January 2015 and January 2025. Ten-year outcomes included rates of anti-reflux surgery and incidence of GERD, esophagitis, Barrett’s esophagus, esophageal cancer, and strictures. Propensity score matching was applied to balance baseline characteristics between groups.
Results: During the study period, 4,660 underwent E-POEM and 4,321 underwent LHM-DF. The average follow-up duration was 849.43 ± 858.71 days for the E-POEM group and 1129.68 ± 999.69 days for the LHM+DF group. In the E-POEM group, 102 patients (2.18%) subsequently underwent surgical or transoral fundoplication within ten years post-procedure, compared to 133 patients (3.07%) in the LHM+DF group who required redo fundoplication. After propensity score matching, the risk of reintervention was significantly lower in the E-POEM group (2.3% vs 3.13, P=0.02).
The incidence of post-procedure esophagitis was significantly higher in the E-POEM group compared to the LHM+DF group (9.97% vs 7.1%, p < 0.01). Additionally, there was a trend toward a higher incidence of Barrett’s esophagus and esophageal stricture in the LHM+DF group; however, these differences did not reach statistical significance. The rate of esophageal cancer was comparable between the two groups (0.42% vs 0.44%, p = 0.86). The incidence of post-procedure GERD was significantly higher in the E-POEM group (37.4%), as opposed to the LHM-DF group (26.11%, P< 0.01).
Discussion: In this large real-world cohort, E-POEM was associated with a significantly lower need for fundoplication compared to LHM+DF. Although rates of post-procedure GERD and esophagitis were modestly higher with E-PEOM, the incidence of reflux-related complications including Barrett’s esophagus, esophageal cancer and esophageal strictures was comparable between the two groups.
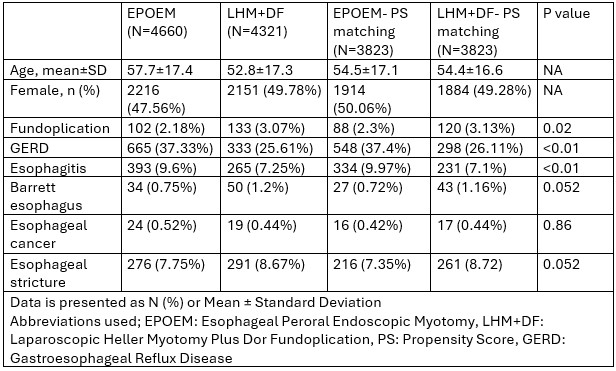
Figure: Table 1- Demographics and Clinical Outcomes in Achalasia Patients Undergoing E-POEM vs. LHM+DF
Disclosures:
Babak Mirminachi indicated no relevant financial relationships.
Anas Atrash indicated no relevant financial relationships.
Jake Fanizza indicated no relevant financial relationships.
David Levinthal: Azurity Pharmaceuticals – Consultant. Gemelli Biotech – Advisory Committee/Board Member. Mahana Therapeutics – Advisor or Review Panel Member. Takeda Pharmaceuticals – Consultant.
Ijlal Ali indicated no relevant financial relationships.
Aylin Tansel indicated no relevant financial relationships.
Sultan Mahmood indicated no relevant financial relationships.
Babak Mirminachi, MD1, Anas Atrash, MD1, Jake D. Fanizza, BS2, David Levinthal, MD, PhD3, Ijlal Akbar. Ali, MD4, Aylin Tansel, MD3, Sultan Mahmood, MD3. P0649 - Esophageal Peroral Endoscopic Myotomy or Laparoscopic Heller Myotomy Plus Dor Fundoplication for Achalasia? Real-World Evidence on GERD and Reflux Complications, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Pittsburgh Medical Center, Harrisburg, PA; 2Drexel University College of Medicine, Harrisburg, PA; 3University of Pittsburgh Medical Center, Pittsburgh, PA; 4University of Oklahoma, Oklahoma City, OK
Introduction: Esophageal Peroral Endoscopic Myotomy (E-POEM) is a minimally invasive treatment for achalasia, offering an effective alternative to Laparoscopic Heller Myotomy (LHM). However, its lack of anti-reflux mechanisms like fundoplication raises concerns about reflux control. This study compares the need for repeat fundoplication, incidence of gastroesophageal reflux disease (GERD), esophagitis, and reflux-related complications in achalasia patients undergoing E-POEM versus Laparoscopic Heller Myotomy plus Dor Fundoplication (LHM+DF).
Methods: We conducted a retrospective cohort study using the U.S. multi-institutional TriNetX database to identify achalasia patients who underwent E-POEM or LHM+DF between January 2015 and January 2025. Ten-year outcomes included rates of anti-reflux surgery and incidence of GERD, esophagitis, Barrett’s esophagus, esophageal cancer, and strictures. Propensity score matching was applied to balance baseline characteristics between groups.
Results: During the study period, 4,660 underwent E-POEM and 4,321 underwent LHM-DF. The average follow-up duration was 849.43 ± 858.71 days for the E-POEM group and 1129.68 ± 999.69 days for the LHM+DF group. In the E-POEM group, 102 patients (2.18%) subsequently underwent surgical or transoral fundoplication within ten years post-procedure, compared to 133 patients (3.07%) in the LHM+DF group who required redo fundoplication. After propensity score matching, the risk of reintervention was significantly lower in the E-POEM group (2.3% vs 3.13, P=0.02).
The incidence of post-procedure esophagitis was significantly higher in the E-POEM group compared to the LHM+DF group (9.97% vs 7.1%, p < 0.01). Additionally, there was a trend toward a higher incidence of Barrett’s esophagus and esophageal stricture in the LHM+DF group; however, these differences did not reach statistical significance. The rate of esophageal cancer was comparable between the two groups (0.42% vs 0.44%, p = 0.86). The incidence of post-procedure GERD was significantly higher in the E-POEM group (37.4%), as opposed to the LHM-DF group (26.11%, P< 0.01).
Discussion: In this large real-world cohort, E-POEM was associated with a significantly lower need for fundoplication compared to LHM+DF. Although rates of post-procedure GERD and esophagitis were modestly higher with E-PEOM, the incidence of reflux-related complications including Barrett’s esophagus, esophageal cancer and esophageal strictures was comparable between the two groups.
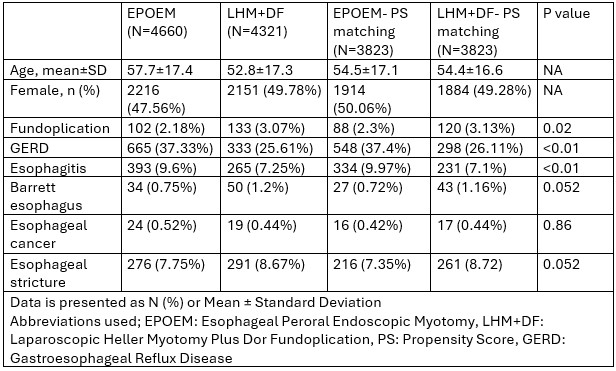
Figure: Table 1- Demographics and Clinical Outcomes in Achalasia Patients Undergoing E-POEM vs. LHM+DF
Disclosures:
Babak Mirminachi indicated no relevant financial relationships.
Anas Atrash indicated no relevant financial relationships.
Jake Fanizza indicated no relevant financial relationships.
David Levinthal: Azurity Pharmaceuticals – Consultant. Gemelli Biotech – Advisory Committee/Board Member. Mahana Therapeutics – Advisor or Review Panel Member. Takeda Pharmaceuticals – Consultant.
Ijlal Ali indicated no relevant financial relationships.
Aylin Tansel indicated no relevant financial relationships.
Sultan Mahmood indicated no relevant financial relationships.
Babak Mirminachi, MD1, Anas Atrash, MD1, Jake D. Fanizza, BS2, David Levinthal, MD, PhD3, Ijlal Akbar. Ali, MD4, Aylin Tansel, MD3, Sultan Mahmood, MD3. P0649 - Esophageal Peroral Endoscopic Myotomy or Laparoscopic Heller Myotomy Plus Dor Fundoplication for Achalasia? Real-World Evidence on GERD and Reflux Complications, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
