Sunday Poster Session
Category: Esophagus
P0640 - Machine Learning Tool to Identify Risk Factors for Incomplete Resection During Endoscopic Submucosal Dissection of Esophageal Adenocarcinoma
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Rishi Bolla, MD
University of South Florida Morsani College of Medicine
Tampa, FL
Presenting Author(s)
Rishi Bolla, MD1, Yi Luo, PhD2, Jeffrey Huang, MD2, Aamir Dam, MD2, Anjuli K. Luthra, MD2, Luis Pena, MD2, Saraswathi Cappelle, MD2, Mark Friedman, MD2, Schaffer Mok, MD2
1University of South Florida Morsani College of Medicine, Tampa, FL; 2Moffitt Cancer Center, Tampa, FL
Introduction: Esophageal adenocarcinoma with submucosal involvement is generally excised by endoscopic submucosal dissection (ESD). Residual tumor status of the dissected specimen is determined via pathology, and incomplete resection as evidenced by microscopic tumor present in the margins is classified as R1. Here we describe a novel, machine-learning tool which can analyze multiple variables and identify risk factors for having an R1 tumor status in esophageal adenocarcinoma patients undergoing ESD.
Methods: We developed a machine learning tool to explore associations among esophageal adenocarcinoma patients’ multiple variables and their R1 tumor status by using a generative explainable Bayesian Network (BN). The BN is a directed acyclic graph with nodes depicting symptoms and predictive outcome, and edges signifying association between connected two nodes. Also, human experts were allowed to guide the BN structure development. We used the area under receiver-operating characteristic curve (AUC) to evaluate the BN’s accuracy. The BN not only shows the dependency among nodes but also illustrates the strength (r) of dependency among them.
Results: A total of 45 patients with esophageal adenocarcinoma who underwent ESD were included in the study. The machine-learning tool was able to identify several associations between R1 tumor status and patient variables such en-bloc resection (r=0.36) and number of cryoablations performed (r=0.64). Furthermore, a strong association between SM2 submucosal involvement and cryoablations performed (r=1.00) was demonstrated by the tool. Additionally, the tool identified tobacco use history, gastroesophageal junction involvement of the tumor, and number of cryoablations performed as predictive for follow up endoscopy (r=0.39, 0.59, and 0.85 respectively). The BN’s prediction performance (AUC) is 0.67 with 95% confidence interval: 0.57-0.80 based on 2000 stratified bootstrap replicates.
Discussion: Our study demonstrates the feasibility of using a machine learning tool to predict associations and outcomes in patients with esophageal adenocarcinoma status post ESD. Clinically, these tools could be used to risk-stratify patients and guide anticipated treatment courses and follow-up recommendations. Further investigation including more patients and expanding the types of gastrointestinal cancers and endoscopic interventions studied may identify even more associations and could represent an expanded role for machine learning models in clinical decision-making.
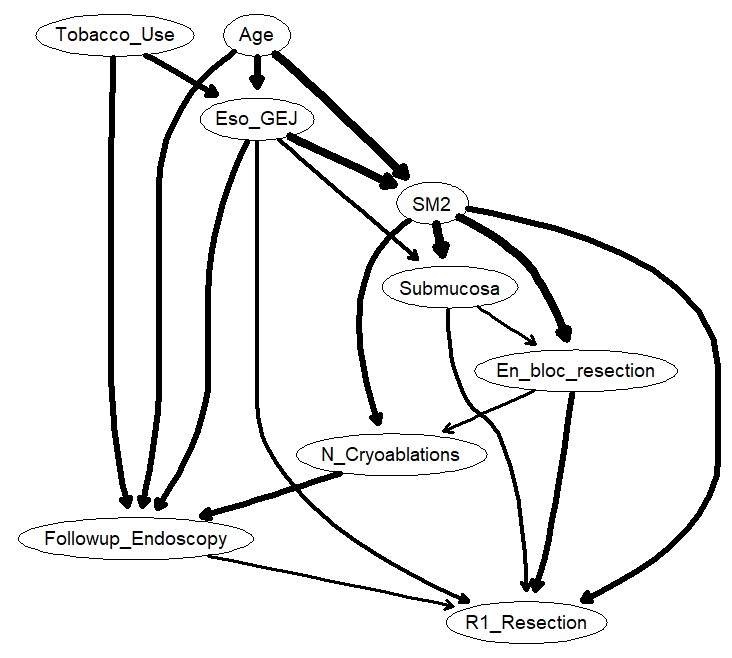
Figure: Figure 1: Diagram representation of various patient variables and R1 resection status as identified by the machine-learning tool.
Disclosures:
Rishi Bolla indicated no relevant financial relationships.
Yi Luo indicated no relevant financial relationships.
Jeffrey Huang indicated no relevant financial relationships.
Aamir Dam indicated no relevant financial relationships.
Anjuli Luthra: Boston Scientific – Consultant. Cook Medical – Speakers Bureau.
Luis Pena indicated no relevant financial relationships.
Saraswathi Cappelle: Olympus – Consultant.
Mark Friedman indicated no relevant financial relationships.
Schaffer Mok: Amgen – Consultant. Steris – Consultant.
Rishi Bolla, MD1, Yi Luo, PhD2, Jeffrey Huang, MD2, Aamir Dam, MD2, Anjuli K. Luthra, MD2, Luis Pena, MD2, Saraswathi Cappelle, MD2, Mark Friedman, MD2, Schaffer Mok, MD2. P0640 - Machine Learning Tool to Identify Risk Factors for Incomplete Resection During Endoscopic Submucosal Dissection of Esophageal Adenocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of South Florida Morsani College of Medicine, Tampa, FL; 2Moffitt Cancer Center, Tampa, FL
Introduction: Esophageal adenocarcinoma with submucosal involvement is generally excised by endoscopic submucosal dissection (ESD). Residual tumor status of the dissected specimen is determined via pathology, and incomplete resection as evidenced by microscopic tumor present in the margins is classified as R1. Here we describe a novel, machine-learning tool which can analyze multiple variables and identify risk factors for having an R1 tumor status in esophageal adenocarcinoma patients undergoing ESD.
Methods: We developed a machine learning tool to explore associations among esophageal adenocarcinoma patients’ multiple variables and their R1 tumor status by using a generative explainable Bayesian Network (BN). The BN is a directed acyclic graph with nodes depicting symptoms and predictive outcome, and edges signifying association between connected two nodes. Also, human experts were allowed to guide the BN structure development. We used the area under receiver-operating characteristic curve (AUC) to evaluate the BN’s accuracy. The BN not only shows the dependency among nodes but also illustrates the strength (r) of dependency among them.
Results: A total of 45 patients with esophageal adenocarcinoma who underwent ESD were included in the study. The machine-learning tool was able to identify several associations between R1 tumor status and patient variables such en-bloc resection (r=0.36) and number of cryoablations performed (r=0.64). Furthermore, a strong association between SM2 submucosal involvement and cryoablations performed (r=1.00) was demonstrated by the tool. Additionally, the tool identified tobacco use history, gastroesophageal junction involvement of the tumor, and number of cryoablations performed as predictive for follow up endoscopy (r=0.39, 0.59, and 0.85 respectively). The BN’s prediction performance (AUC) is 0.67 with 95% confidence interval: 0.57-0.80 based on 2000 stratified bootstrap replicates.
Discussion: Our study demonstrates the feasibility of using a machine learning tool to predict associations and outcomes in patients with esophageal adenocarcinoma status post ESD. Clinically, these tools could be used to risk-stratify patients and guide anticipated treatment courses and follow-up recommendations. Further investigation including more patients and expanding the types of gastrointestinal cancers and endoscopic interventions studied may identify even more associations and could represent an expanded role for machine learning models in clinical decision-making.
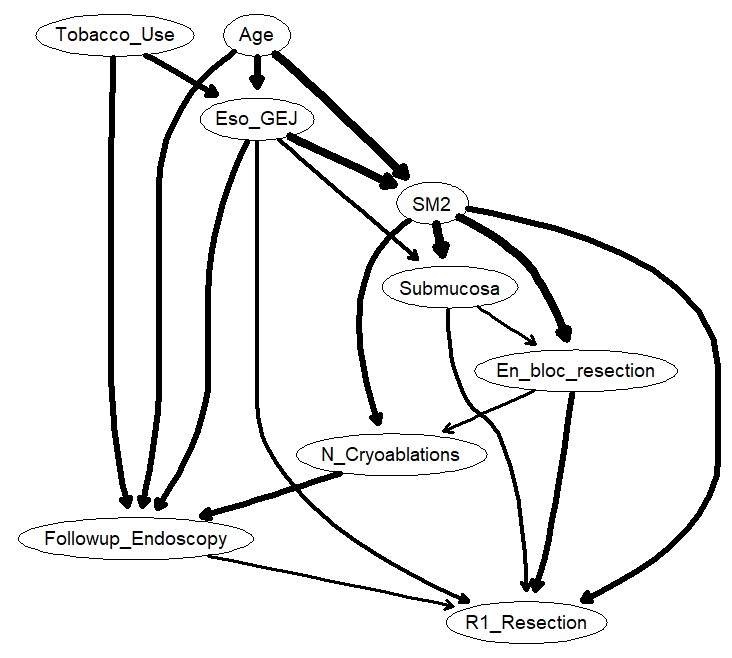
Figure: Figure 1: Diagram representation of various patient variables and R1 resection status as identified by the machine-learning tool.
Disclosures:
Rishi Bolla indicated no relevant financial relationships.
Yi Luo indicated no relevant financial relationships.
Jeffrey Huang indicated no relevant financial relationships.
Aamir Dam indicated no relevant financial relationships.
Anjuli Luthra: Boston Scientific – Consultant. Cook Medical – Speakers Bureau.
Luis Pena indicated no relevant financial relationships.
Saraswathi Cappelle: Olympus – Consultant.
Mark Friedman indicated no relevant financial relationships.
Schaffer Mok: Amgen – Consultant. Steris – Consultant.
Rishi Bolla, MD1, Yi Luo, PhD2, Jeffrey Huang, MD2, Aamir Dam, MD2, Anjuli K. Luthra, MD2, Luis Pena, MD2, Saraswathi Cappelle, MD2, Mark Friedman, MD2, Schaffer Mok, MD2. P0640 - Machine Learning Tool to Identify Risk Factors for Incomplete Resection During Endoscopic Submucosal Dissection of Esophageal Adenocarcinoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

