Sunday Poster Session
Category: Esophagus
P0632 - Impact of Pre-Transplant Esophageal Findings on Lung Transplant Outcomes: A Single-Center Retrospective Cohort Study
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Jameel Alp, MD (he/him/his)
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Jameel Alp, MD1, Rahul Karna, MD2, Todd De For, MS1, Anupam Kumar, MD1, Joshua Sloan, DO1
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN
Introduction: Chronic lung allograft dysfunction (CLAD) is the leading cause of late morbidity and mortality following lung transplantation. Gastroesophageal reflux disease (GERD) and esophageal dysmotility have been implicated as potential contributors to CLAD. Comprehensive pre-transplant esophageal evaluation is routinely performed in many centers, but whether it predicts rejection or mortality remains uncertain. The primary aim of this study was to evaluate if motility or reflux abnormalities may impact the development of CLAD post-transplant.
Methods: This retrospective cohort study included adults (≥18 years) undergoing lung transplant at a tertiary center (7/2020-7/2024). Data from electronic records included demographics, transplant details, pre-transplant reflux and motility testing. Esophageal findings were defined as GERD and/or esophageal dysmotility. Primary outcome was development of CLAD; secondary outcomes included acute rejection (AR), time to CLAD/AR, and survival. Statistical analyses included competing risk models and survival analysis.
Results: Among 162 lung transplant recipients (median age 64 years, 48% female, 86% White), 54% had a pre-transplant esophageal finding detected in either EGD, high-resolution manometry, or 24-hour pH-impedance. At 2 years post-transplant, cumulative incidence of CLAD was 88%, with no significant difference by esophageal finding status (GERD [+] vs [-]: 84% vs 91% [p=0.39]; dysmotility [+] vs [-]: 88% vs 85% [p=0.79]). AR occurred in 28%, similarly unaffected by esophageal finding (HR 2.00, 95% CI 0.75-5.21, p=0.17). 1- and 3-year survival estimates did not differ significantly between groups (1-year: 86% vs 90%, 3-year: 78% vs 77%, p=0.89). Median time to CLAD was approximately 146 days. (See Table.)
Discussion: More than half of the patients had a pre-transplant esophageal finding in our cohort. However, they were not associated with increased risk of CLAD, AR, or reduced survival post-transplant. These findings challenge the prevailing view that GERD and motility abnormalities independently worsen lung transplant outcomes. Additional evaluation is necessary to elucidate if specific motility findings, or reflux metrics are more likely than others to contribute to the development of CLAD or AR.
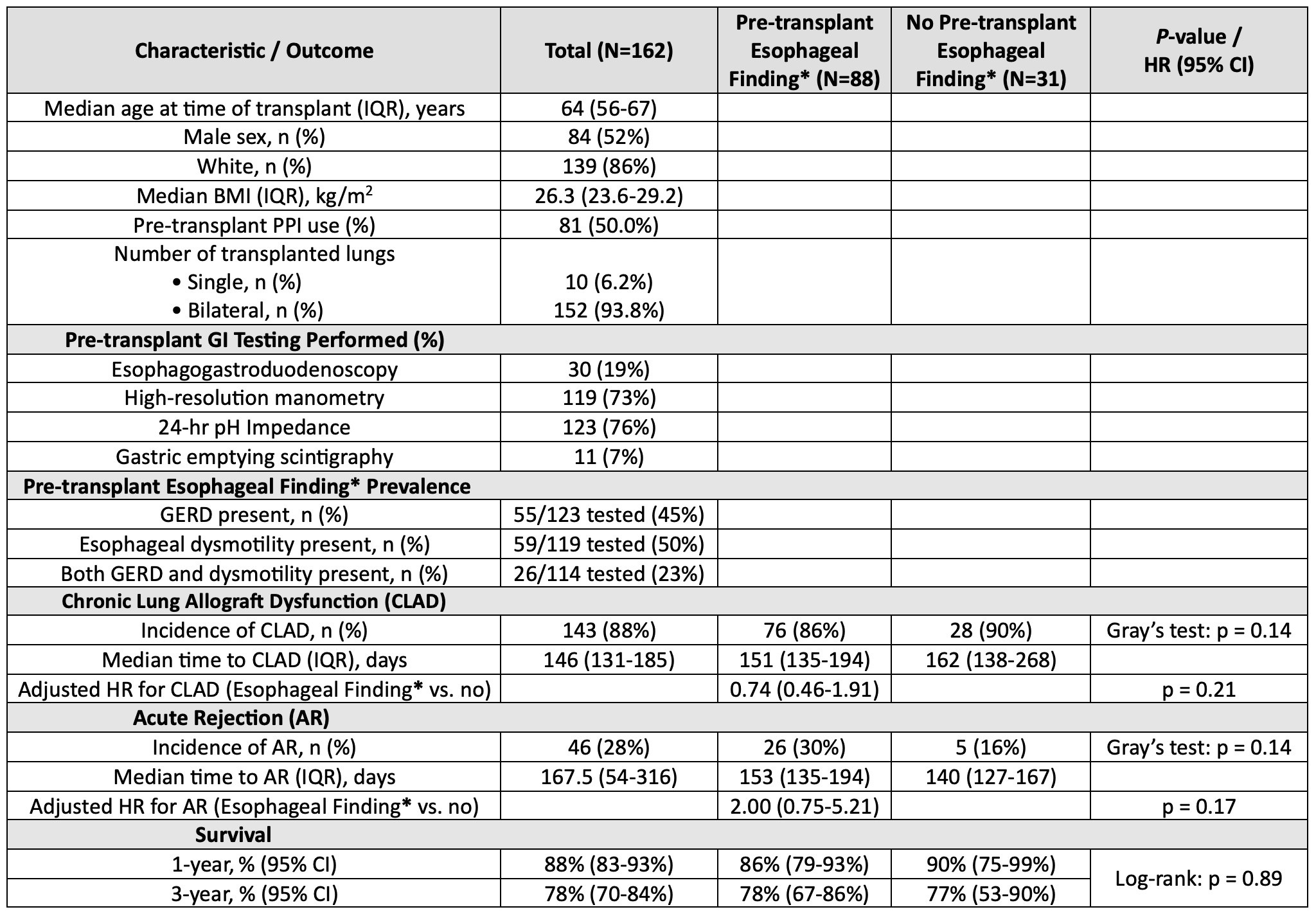
Figure: Table. Patient demographics, pre-transplant gastrointestinal (GI) evaluation, and post-transplant outcomes, including chronic lung allograft dysfunction (CLAD), acute rejection (AR), and survival, stratified by presence of pre-transplant esophageal finding.
* Pre-transplant esophageal finding is defined as gastroesophageal reflux disease (GERD) and/or an esophageal dysmotility (e.g., achalasia, esophagogastric junction outflow obstruction, absent contractility etc.). GERD was defined as an acid exposure time (AET) >6%, number of reflux episodes >80 on 24-hour pH impedance testing, and/or Los Angeles (LA) grade B, C, or D esophagitis on esophagogastroduodenoscopy (EGD).
Disclosures:
Jameel Alp indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Todd De For indicated no relevant financial relationships.
Anupam Kumar indicated no relevant financial relationships.
Joshua Sloan: Phathom Pharmaceuticals – Speakers Bureau. Sanofi-Regeneron – Advisory Committee/Board Member, Speakers Bureau. Takeda Pharmaceuticals – Advisory Committee/Board Member.
Jameel Alp, MD1, Rahul Karna, MD2, Todd De For, MS1, Anupam Kumar, MD1, Joshua Sloan, DO1. P0632 - Impact of Pre-Transplant Esophageal Findings on Lung Transplant Outcomes: A Single-Center Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2University of Minnesota Medical Center, Minneapolis, MN
Introduction: Chronic lung allograft dysfunction (CLAD) is the leading cause of late morbidity and mortality following lung transplantation. Gastroesophageal reflux disease (GERD) and esophageal dysmotility have been implicated as potential contributors to CLAD. Comprehensive pre-transplant esophageal evaluation is routinely performed in many centers, but whether it predicts rejection or mortality remains uncertain. The primary aim of this study was to evaluate if motility or reflux abnormalities may impact the development of CLAD post-transplant.
Methods: This retrospective cohort study included adults (≥18 years) undergoing lung transplant at a tertiary center (7/2020-7/2024). Data from electronic records included demographics, transplant details, pre-transplant reflux and motility testing. Esophageal findings were defined as GERD and/or esophageal dysmotility. Primary outcome was development of CLAD; secondary outcomes included acute rejection (AR), time to CLAD/AR, and survival. Statistical analyses included competing risk models and survival analysis.
Results: Among 162 lung transplant recipients (median age 64 years, 48% female, 86% White), 54% had a pre-transplant esophageal finding detected in either EGD, high-resolution manometry, or 24-hour pH-impedance. At 2 years post-transplant, cumulative incidence of CLAD was 88%, with no significant difference by esophageal finding status (GERD [+] vs [-]: 84% vs 91% [p=0.39]; dysmotility [+] vs [-]: 88% vs 85% [p=0.79]). AR occurred in 28%, similarly unaffected by esophageal finding (HR 2.00, 95% CI 0.75-5.21, p=0.17). 1- and 3-year survival estimates did not differ significantly between groups (1-year: 86% vs 90%, 3-year: 78% vs 77%, p=0.89). Median time to CLAD was approximately 146 days. (See Table.)
Discussion: More than half of the patients had a pre-transplant esophageal finding in our cohort. However, they were not associated with increased risk of CLAD, AR, or reduced survival post-transplant. These findings challenge the prevailing view that GERD and motility abnormalities independently worsen lung transplant outcomes. Additional evaluation is necessary to elucidate if specific motility findings, or reflux metrics are more likely than others to contribute to the development of CLAD or AR.
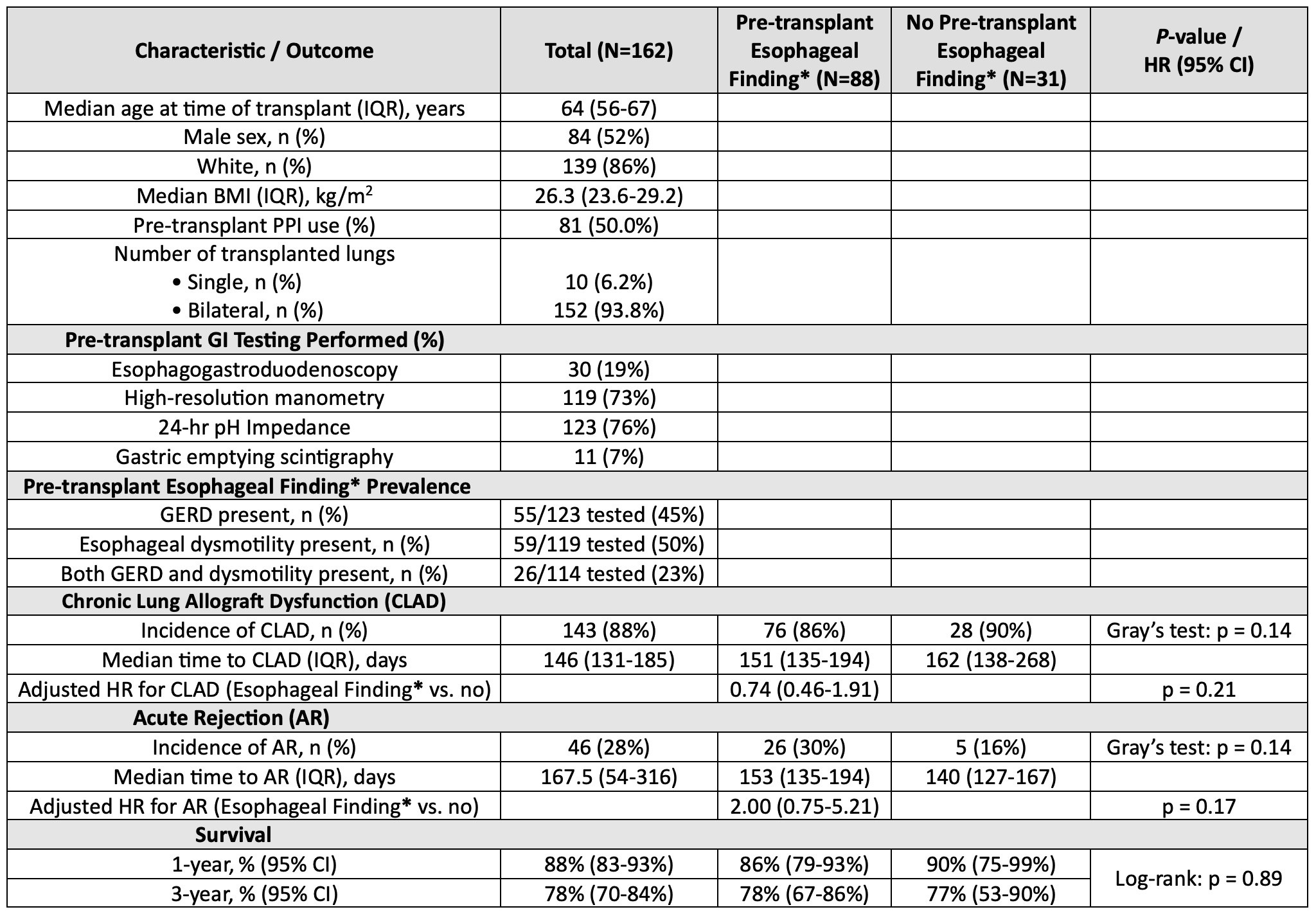
Figure: Table. Patient demographics, pre-transplant gastrointestinal (GI) evaluation, and post-transplant outcomes, including chronic lung allograft dysfunction (CLAD), acute rejection (AR), and survival, stratified by presence of pre-transplant esophageal finding.
* Pre-transplant esophageal finding is defined as gastroesophageal reflux disease (GERD) and/or an esophageal dysmotility (e.g., achalasia, esophagogastric junction outflow obstruction, absent contractility etc.). GERD was defined as an acid exposure time (AET) >6%, number of reflux episodes >80 on 24-hour pH impedance testing, and/or Los Angeles (LA) grade B, C, or D esophagitis on esophagogastroduodenoscopy (EGD).
Disclosures:
Jameel Alp indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Todd De For indicated no relevant financial relationships.
Anupam Kumar indicated no relevant financial relationships.
Joshua Sloan: Phathom Pharmaceuticals – Speakers Bureau. Sanofi-Regeneron – Advisory Committee/Board Member, Speakers Bureau. Takeda Pharmaceuticals – Advisory Committee/Board Member.
Jameel Alp, MD1, Rahul Karna, MD2, Todd De For, MS1, Anupam Kumar, MD1, Joshua Sloan, DO1. P0632 - Impact of Pre-Transplant Esophageal Findings on Lung Transplant Outcomes: A Single-Center Retrospective Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
