Sunday Poster Session
Category: Esophagus
P0630 - Abnormalities on Barium Esophagram Predict Esophageal Structural and Motility Disorders in Patients With Dysphagia Symptoms
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Sabrina L. Chen, MD (she/her/hers)
UCSF
San Francisco, CA
Presenting Author(s)
Sabrina L. Chen, MD, Diana Partida, MD, Priya Kathpalia, MD, Connie W. Wang, MD
UCSF, San Francisco, CA
Introduction: Barium esophagram is a dynamic radiologic study used to evaluate esophageal anatomy, presence of hiatal hernias, diverticula, and strictures. It may also suggest swallowing disorders, reflux, and dysmotility, though it is not validated for diagnosing motility disorders. High-resolution esophageal manometry remains the gold standard for assessing motility, while esophagogastroduodenoscopy (EGD) is the reference for identifying structural and mucosal etiologies of esophageal dysphagia. Given the non-invasive nature and relative widespread availability of esophagram, this study aimed to assess its concordance with EGD and manometry in diagnosing structural and motility-related causes of esophageal dysphagia.
Methods: We performed a retrospective cohort study of adults referred to gastroenterology for dysphagia between September 2017 and August 2023. Patients who underwent both esophagram and either manometry or EGD within one year were included. Collected data included demographics, initial gastroenterology notes, and results of esophageal testing. Concordance between esophagram findings and subsequent manometry or EGD results was assessed using chi-squared tests. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of esophagram were calculated with 95% confidence intervals.
Results: Of 199 referrals, 69 patients underwent esophagram; 20 also had manometry and 29 underwent EGD. Esophagram identified dysmotility in 31 cases (45.6%), and manometry confirmed dysmotility in 8 (40.0%), showing significant concordance (p< 0.001). Sensitivity and specificity for detecting dysmotility were 100% (CI: 63.1–100%) and 75% (CI: 42.8–94.5%) (Table 2a), respectively. Structural abnormalities were seen in 15 esophagrams (22.1%) and 9 EGDs (31.0%), with significant concordance (p=0.01). Sensitivity and specificity for structural abnormalities were 55.6% (CI: 21.2–86.3%) and 90% (CI: 68.3–98.8%), respectively (Table 2b).
Discussion: Barium esophagram demonstrates strong concordance with manometry and EGD in identifying both motility and structural abnormalities. It may serve as a valuable first-line tool in the evaluation of esophageal dysphagia, particularly in patients seeking non-invasive options or those with higher procedural risks.
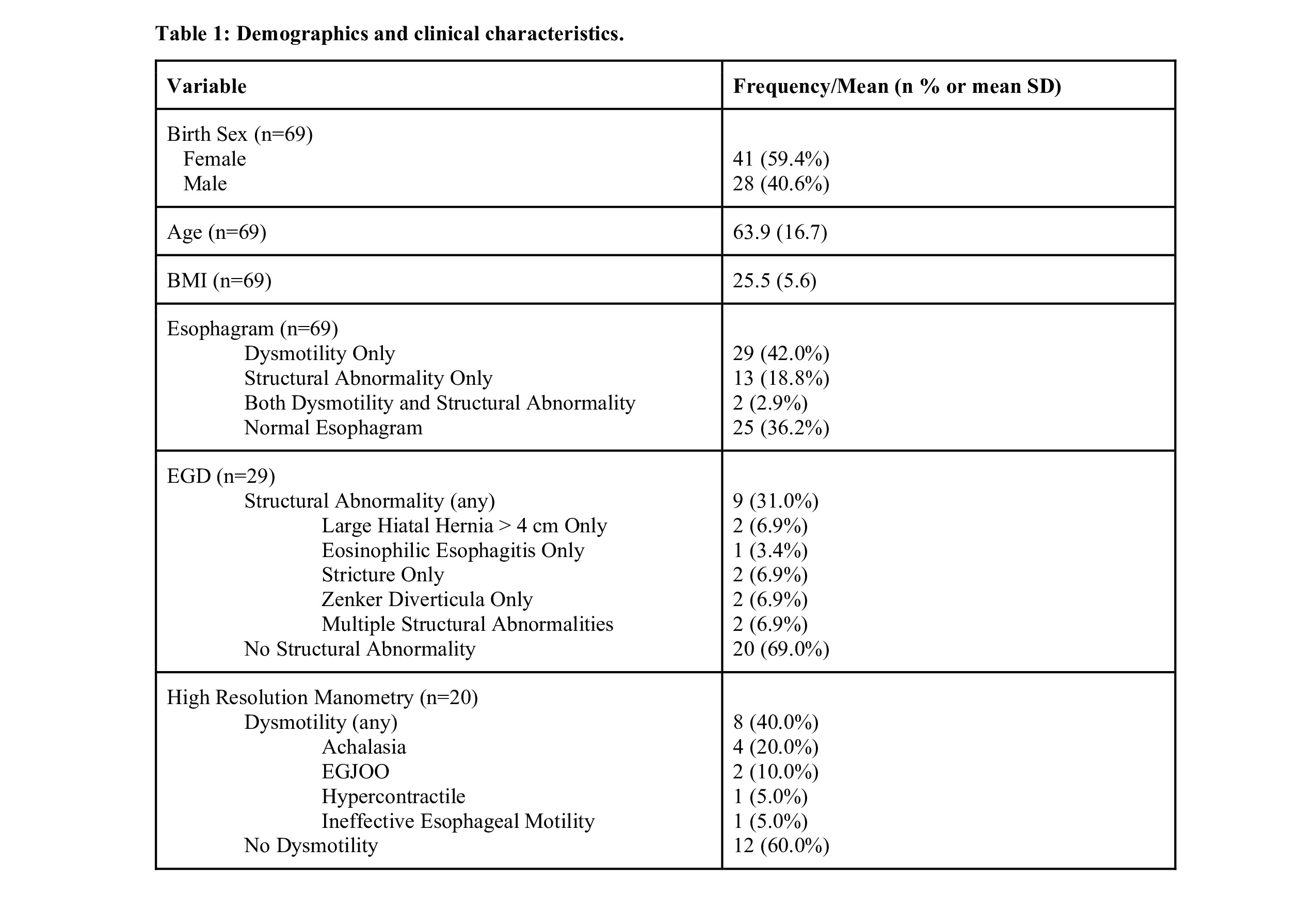
Figure: Table 1: Demographics and clinical characteristics.
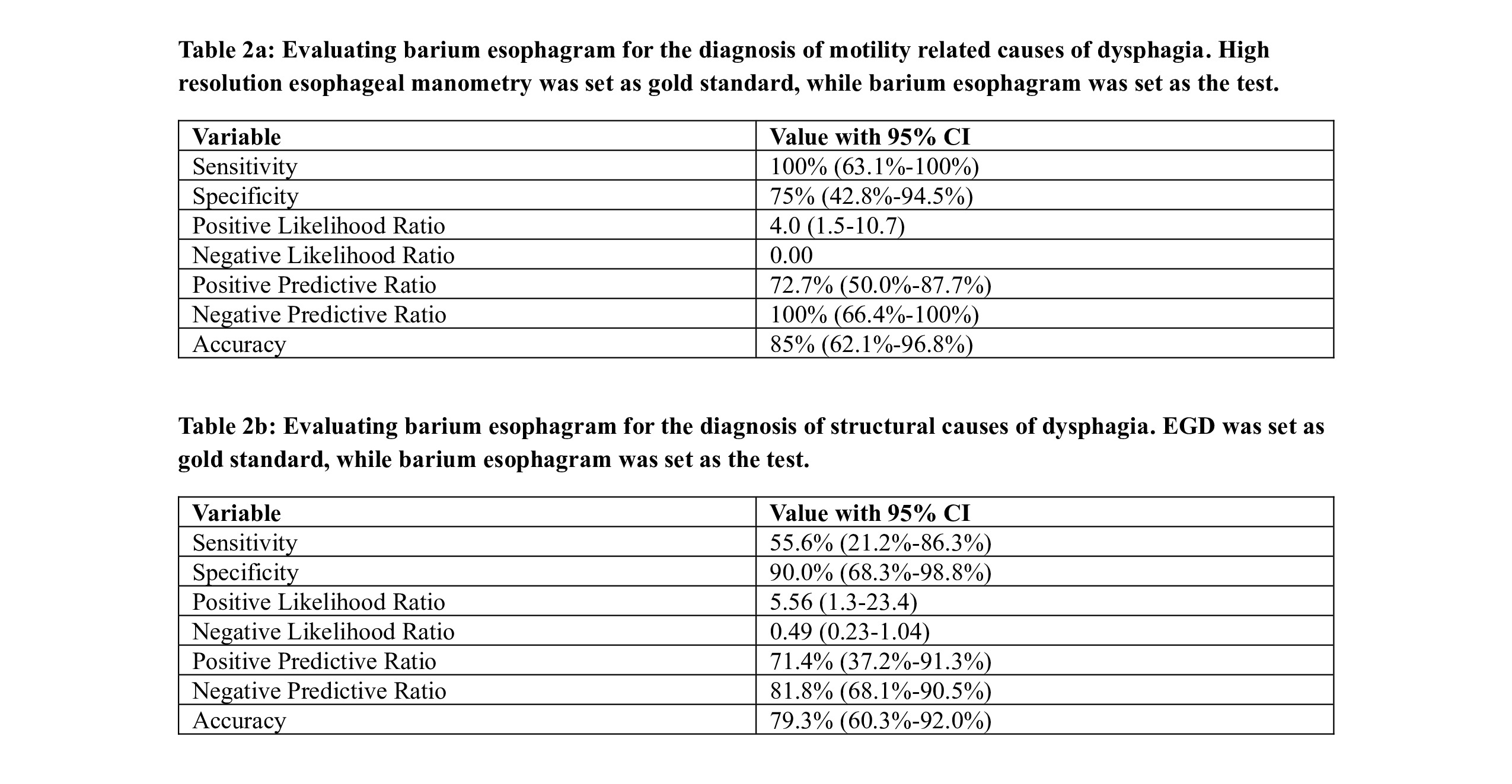
Figure: Table 2a: Evaluating barium esophagram for the diagnosis of motility related causes of dysphagia. High resolution esophageal manometry was set as gold standard, while barium esophagram was set as the test.
Table 2b: Evaluating barium esophagram for the diagnosis of structural causes of dysphagia. EGD was set as gold standard, while barium esophagram was set as the test.
Disclosures:
Sabrina Chen indicated no relevant financial relationships.
Diana Partida indicated no relevant financial relationships.
Priya Kathpalia indicated no relevant financial relationships.
Connie Wang indicated no relevant financial relationships.
Sabrina L. Chen, MD, Diana Partida, MD, Priya Kathpalia, MD, Connie W. Wang, MD. P0630 - Abnormalities on Barium Esophagram Predict Esophageal Structural and Motility Disorders in Patients With Dysphagia Symptoms, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
UCSF, San Francisco, CA
Introduction: Barium esophagram is a dynamic radiologic study used to evaluate esophageal anatomy, presence of hiatal hernias, diverticula, and strictures. It may also suggest swallowing disorders, reflux, and dysmotility, though it is not validated for diagnosing motility disorders. High-resolution esophageal manometry remains the gold standard for assessing motility, while esophagogastroduodenoscopy (EGD) is the reference for identifying structural and mucosal etiologies of esophageal dysphagia. Given the non-invasive nature and relative widespread availability of esophagram, this study aimed to assess its concordance with EGD and manometry in diagnosing structural and motility-related causes of esophageal dysphagia.
Methods: We performed a retrospective cohort study of adults referred to gastroenterology for dysphagia between September 2017 and August 2023. Patients who underwent both esophagram and either manometry or EGD within one year were included. Collected data included demographics, initial gastroenterology notes, and results of esophageal testing. Concordance between esophagram findings and subsequent manometry or EGD results was assessed using chi-squared tests. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of esophagram were calculated with 95% confidence intervals.
Results: Of 199 referrals, 69 patients underwent esophagram; 20 also had manometry and 29 underwent EGD. Esophagram identified dysmotility in 31 cases (45.6%), and manometry confirmed dysmotility in 8 (40.0%), showing significant concordance (p< 0.001). Sensitivity and specificity for detecting dysmotility were 100% (CI: 63.1–100%) and 75% (CI: 42.8–94.5%) (Table 2a), respectively. Structural abnormalities were seen in 15 esophagrams (22.1%) and 9 EGDs (31.0%), with significant concordance (p=0.01). Sensitivity and specificity for structural abnormalities were 55.6% (CI: 21.2–86.3%) and 90% (CI: 68.3–98.8%), respectively (Table 2b).
Discussion: Barium esophagram demonstrates strong concordance with manometry and EGD in identifying both motility and structural abnormalities. It may serve as a valuable first-line tool in the evaluation of esophageal dysphagia, particularly in patients seeking non-invasive options or those with higher procedural risks.
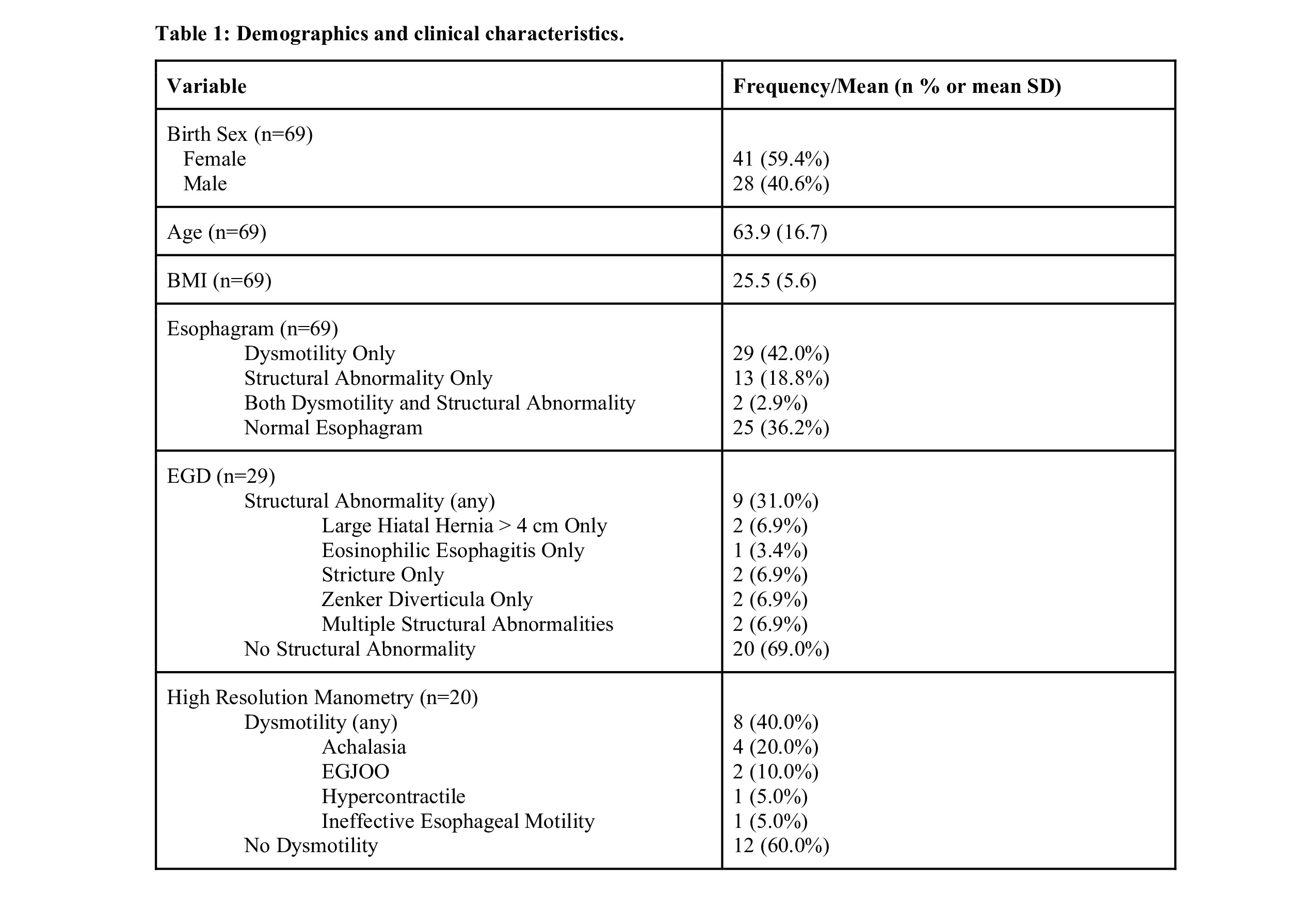
Figure: Table 1: Demographics and clinical characteristics.
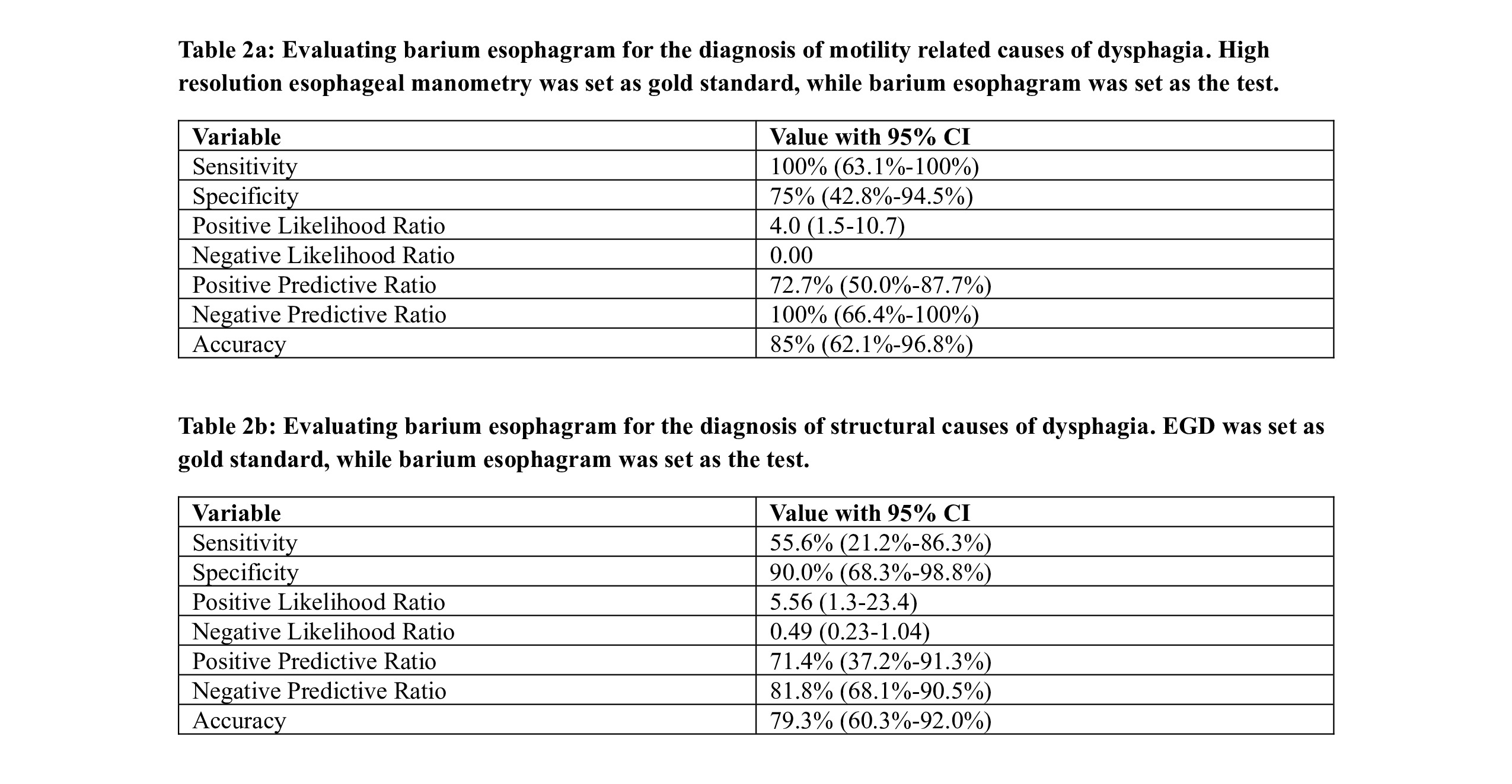
Figure: Table 2a: Evaluating barium esophagram for the diagnosis of motility related causes of dysphagia. High resolution esophageal manometry was set as gold standard, while barium esophagram was set as the test.
Table 2b: Evaluating barium esophagram for the diagnosis of structural causes of dysphagia. EGD was set as gold standard, while barium esophagram was set as the test.
Disclosures:
Sabrina Chen indicated no relevant financial relationships.
Diana Partida indicated no relevant financial relationships.
Priya Kathpalia indicated no relevant financial relationships.
Connie Wang indicated no relevant financial relationships.
Sabrina L. Chen, MD, Diana Partida, MD, Priya Kathpalia, MD, Connie W. Wang, MD. P0630 - Abnormalities on Barium Esophagram Predict Esophageal Structural and Motility Disorders in Patients With Dysphagia Symptoms, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

