Sunday Poster Session
Category: Esophagus
P0604 - Confirming the Concordance of LA Grade B Esophagitis With Gastroesophageal Reflux Disease on Reflux Quantification Testing
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Soha Noorani, DO
Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Soha Noorani, DO1, Rama Hussein, DO2, Yuying Luo, MD3, Daniela Jodorkovsky, MD4
1Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York City, NY; 3Mount Sinai West & Morningside, New York, NY; 4Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: The Lyon Consensus 2.0 included the diagnosis of Los Angeles (LA) Grade B esophagitis as actionable, suggesting that an endoscopic diagnosis alone was sufficient for management without the need for quantitative reflux testing. However, given that symptoms of gastroesophageal reflux disease (GERD) may overlap with other esophageal disorders of the gut-brain interaction, reflux quantification can help elucidate distinctions while also serving as another tool to confirm the severity of LA Grade B esophagitis.
Methods: A retrospective analysis was performed of consecutive patients between October 2022 and September 2023 who had both evidence of LA Grade B esophagitis on esophagogastroduodenoscopy (EGD) and subsequent quantitative reflux testing (24-hour impedance monitoring and 48-hour wireless pH testing). Outcomes included the identification of test factors aligning with a positive pH study, including measurements of acid exposure time (AET), total number of reflux events, symptom index (SI), and symptoms association probability (SAP).
Results: Of the 169 patients with LA Grade B esophagitis on EGD (n= 80 female, average age 55 years +/- 15.9 years), 14 patients (8.2%) underwent subsequent reflux quantification testing off of acid-suppressive medications (Table 1). There were no significant differences in mean age, sex, or smoking history between the patients who underwent reflux monitoring versus those who did not (n = 155).
12 patients (85%) had wireless pH monitoring, while 2 (14%) had 24-hour impedance monitoring. 85.7% had a total AET score >6%, and 100% had an AET >5%. Most patients (71%) had more than 80 total reflux events. 85% had a SI ≥ 50% while 64% had a SAP ≥ 95%, supporting positive symptom correlation for the majority of patients. 71% of patients were recommended a change in therapy following testing, including medication escalation (50%) and referral for anti-reflux surgery (21%).
Discussion: In our cohort, there was a positive concordance between quantitative reflux testing and the presence of LA grade B on endoscopy. This study supports the concept of LA grade B as “actionable” reflux. Future studies with larger sample sizes could provide deeper insight as to the utility of EGD alone without quantitative reflux monitoring when referring to more invasive treatment options, such as surgery in patients with LA Grade B esophagitis.
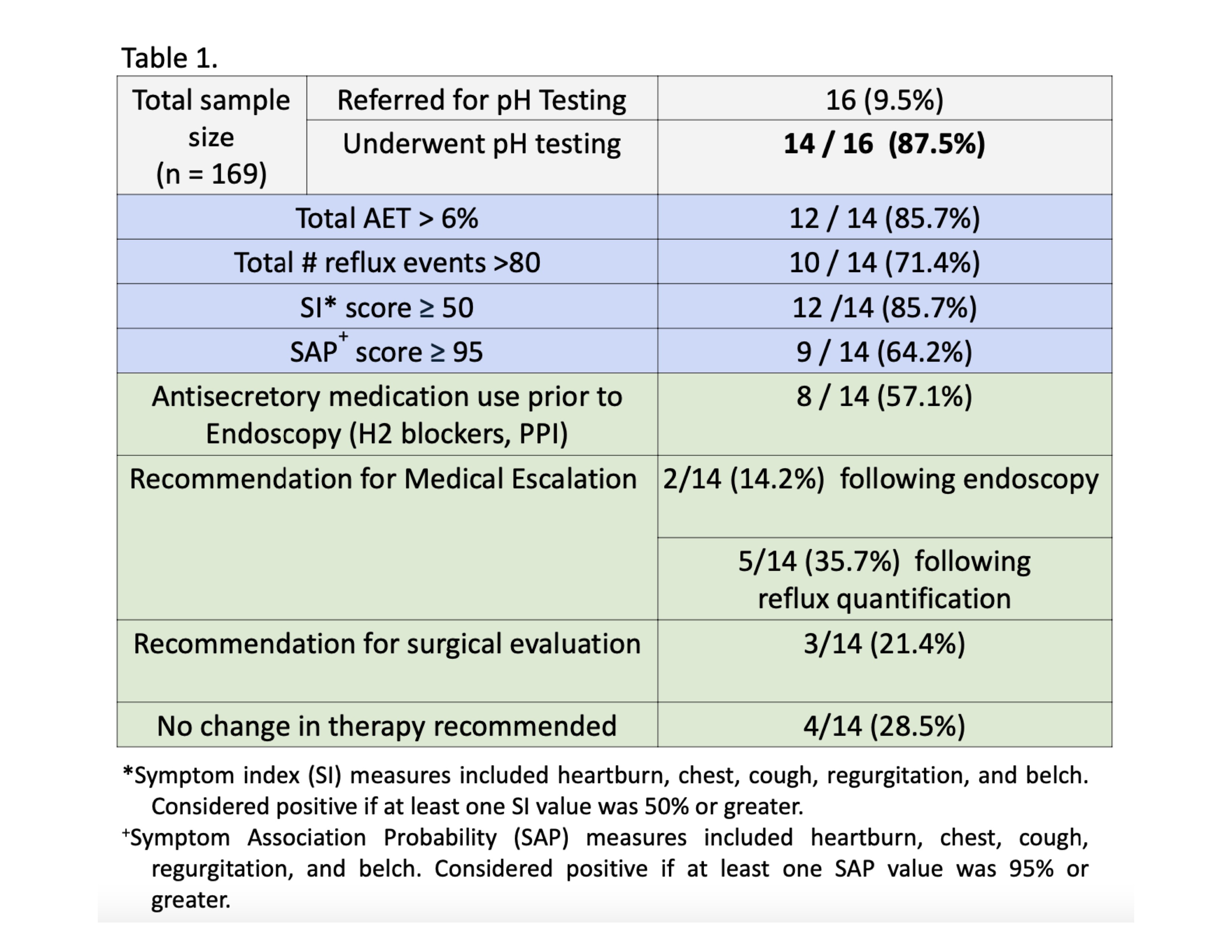
Figure: Treatment recommendations for patients diagnosed with LA Grade B esophagitis and GERD.
Disclosures:
Soha Noorani indicated no relevant financial relationships.
Rama Hussein indicated no relevant financial relationships.
Yuying Luo: Ardelyx – Grant/Research Support.
Daniela Jodorkovsky indicated no relevant financial relationships.
Soha Noorani, DO1, Rama Hussein, DO2, Yuying Luo, MD3, Daniela Jodorkovsky, MD4. P0604 - Confirming the Concordance of LA Grade B Esophagitis With Gastroesophageal Reflux Disease on Reflux Quantification Testing, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York City, NY; 3Mount Sinai West & Morningside, New York, NY; 4Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: The Lyon Consensus 2.0 included the diagnosis of Los Angeles (LA) Grade B esophagitis as actionable, suggesting that an endoscopic diagnosis alone was sufficient for management without the need for quantitative reflux testing. However, given that symptoms of gastroesophageal reflux disease (GERD) may overlap with other esophageal disorders of the gut-brain interaction, reflux quantification can help elucidate distinctions while also serving as another tool to confirm the severity of LA Grade B esophagitis.
Methods: A retrospective analysis was performed of consecutive patients between October 2022 and September 2023 who had both evidence of LA Grade B esophagitis on esophagogastroduodenoscopy (EGD) and subsequent quantitative reflux testing (24-hour impedance monitoring and 48-hour wireless pH testing). Outcomes included the identification of test factors aligning with a positive pH study, including measurements of acid exposure time (AET), total number of reflux events, symptom index (SI), and symptoms association probability (SAP).
Results: Of the 169 patients with LA Grade B esophagitis on EGD (n= 80 female, average age 55 years +/- 15.9 years), 14 patients (8.2%) underwent subsequent reflux quantification testing off of acid-suppressive medications (Table 1). There were no significant differences in mean age, sex, or smoking history between the patients who underwent reflux monitoring versus those who did not (n = 155).
12 patients (85%) had wireless pH monitoring, while 2 (14%) had 24-hour impedance monitoring. 85.7% had a total AET score >6%, and 100% had an AET >5%. Most patients (71%) had more than 80 total reflux events. 85% had a SI ≥ 50% while 64% had a SAP ≥ 95%, supporting positive symptom correlation for the majority of patients. 71% of patients were recommended a change in therapy following testing, including medication escalation (50%) and referral for anti-reflux surgery (21%).
Discussion: In our cohort, there was a positive concordance between quantitative reflux testing and the presence of LA grade B on endoscopy. This study supports the concept of LA grade B as “actionable” reflux. Future studies with larger sample sizes could provide deeper insight as to the utility of EGD alone without quantitative reflux monitoring when referring to more invasive treatment options, such as surgery in patients with LA Grade B esophagitis.
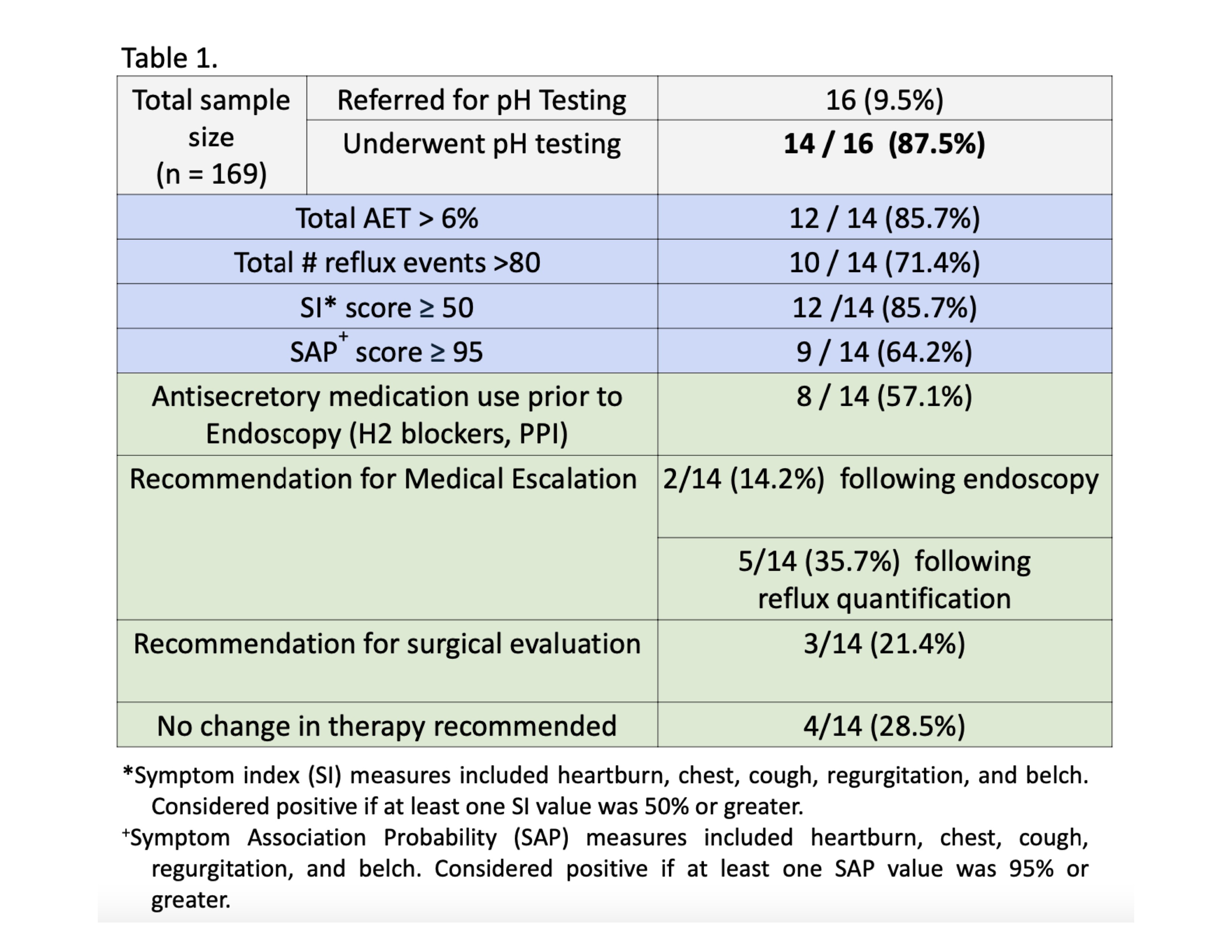
Figure: Treatment recommendations for patients diagnosed with LA Grade B esophagitis and GERD.
Disclosures:
Soha Noorani indicated no relevant financial relationships.
Rama Hussein indicated no relevant financial relationships.
Yuying Luo: Ardelyx – Grant/Research Support.
Daniela Jodorkovsky indicated no relevant financial relationships.
Soha Noorani, DO1, Rama Hussein, DO2, Yuying Luo, MD3, Daniela Jodorkovsky, MD4. P0604 - Confirming the Concordance of LA Grade B Esophagitis With Gastroesophageal Reflux Disease on Reflux Quantification Testing, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

