Sunday Poster Session
Category: Endoscopy Video Forum
P0582 - Hemobilia Secondary to Choledochal Varices: A Rare Cause of GI Bleeding Managed Endoscopically With Biliary Stenting
- PH
Paul Hong, MD
University of Chicago, NorthShore University Health Systems
Chicago, IL
Presenting Author(s)
1University of Chicago, NorthShore University Health Systems, Chicago, IL; 2University of Chicago, NorthShore Gastroenterology, Evanston, IL; 3University of Chicago, Northshore University Healthsystem, Chicago, IL
Introduction:
Choledochal varices are an uncommon cause of hemobilia and can mimic neoplasia on cross-sectional imaging, especially during active bleeding or in the presence of an intraductal blood clot. Historically, management has been with portosystemic shunting.
Case Description/
Methods:
A 68-year-old male was admitted to our system with new, worsening abdominal distention and abdominal pain. On computed tomography (CT), notable findings included cirrhotic liver morphology, large-intra-abdominal ascites, a portal venous thrombus with cavernous transformation, an ill-defined hypoattenuation near the portal venous thrombus concerning for a mass, and pancreatic calcification suggestive of chronic pancreatitis. The patient was found to be hepatitis C positive and did endorse a longstanding alcohol abuse.
During his admission, the patient also developed melena with an acute hemoglobin decline to 11.4 g/dL. After a multi-disciplinary discussion, the decision was made to pursue esophagogastroduodenoscopy (EGD) evaluation for melena; Endoscopic Ultrasound (EUS) to evaluate the hypoattenuation on CT scan; and Endoscopic Retrograde Cholangiopancreatography (ERCP) with Cholangioscopy.
Aside from small, non-bleeding esophageal varices and portal hypertensive gastropathy, the EGD was unremarkable. On EUS, there was well-defined, heteroechoic lesion within the lumen of the bile duct; the bile duct in this region was also surrounded by doppler-positive structures consistent with choledochal varices. ERCP was performed, showing a large intraductal filling defect that was freely mobile, and cholangioscopy
confirmed a large blood clot, not a mass. Extraction of the clot was successful, and classic features of choledochal varices were seen on the post-extraction cholangiogram. A transpapillary fully covered metal stent was placed with resulting hemostasis and no recurrence of hemorrhage.
The patient ultimately was discharged, but prior to liver transplant evaluation, he was readmitted with septic shock from aspiration pneumonia with Enterobacter cloacae bacteremia and ultimately died in hospice.
Discussion:
Bile duct varices can cause extrinsic biliary compression (even mimicking a malignant stricture on cholangiogram) with rare cases of hemobilia described in old literature. While portosystemic shunting is the typical management strategy, we describe a successful case of endoscopic management with biliary stenting, which could be considered in patients who are poor candidates for portosystemic shunting or transplantation.
Figure: Figure 1: EUS with doppler demonstrating varices surrounding the bile duct with intraductal lesion (clot)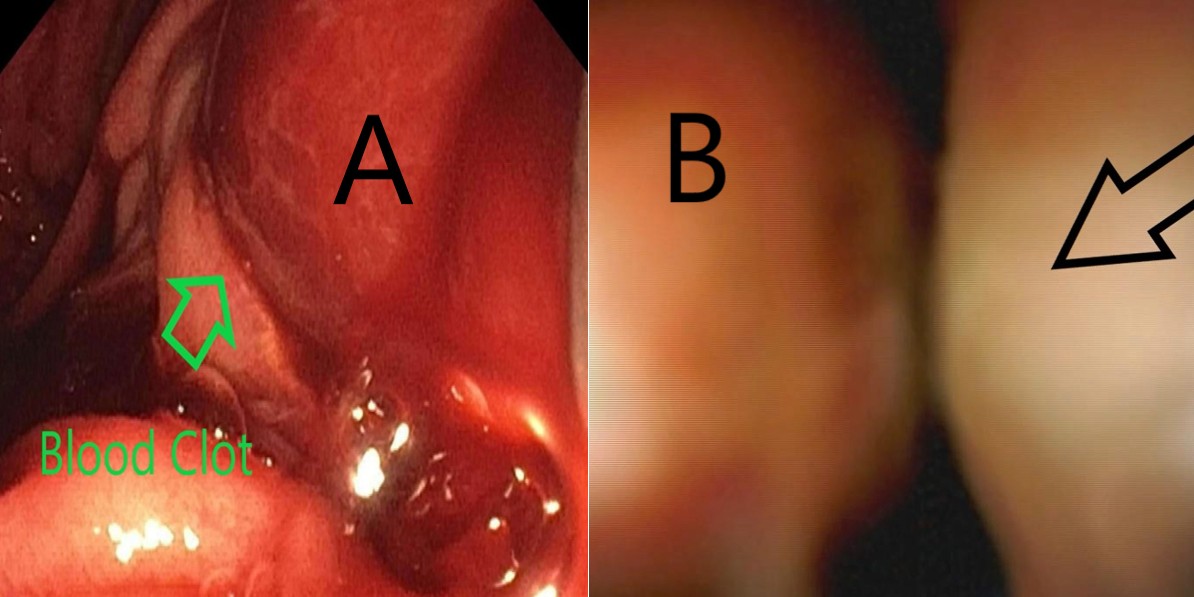
Figure: Figure 2A and 2B: Extracted blood clot from bile duct (A) and cholangioscopic view of extrinsic biliary compression from choledochal varices (B).
Disclosures:
Paul Hong indicated no relevant financial relationships.
Sarah Burroughs indicated no relevant financial relationships.
Edward Villa: Olympus Corporation – Consultant.
Paul Hong, MD1, Sarah Burroughs, DO2, Edward C. Villa, MD3. P0582 - Hemobilia Secondary to Choledochal Varices: A Rare Cause of GI Bleeding Managed Endoscopically With Biliary Stenting, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
