Sunday Poster Session
Category: Diet, Nutrition, and Obesity
P0569 - Reevaluating the Role of Parenteral Nutrition in Severe Alcoholic Hepatitis: Insights From a National Inpatient Cohort
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Suman Sharma, MD
Baystate Medical Center
East Longmeadow, MA
Presenting Author(s)
Suman Sharma, MD1, Nilisha Regmi, MD1, Uchit Thapa, MD2, Subash Ghimire, MD3
1Baystate Medical Center, East Longmeadow, MA; 2Baystate Medical Center, Hartford, CT; 3Guthrie Robert Packer Hospital, Department of Gastroenterology, Sayre, PA
Introduction: Severe alcoholic hepatitis (AH) is associated with significant inpatient mortality, especially in malnourished patients. Although nutritional support is important in hospitalized patients, the role of total parenteral nutrition (TPN) remains controversial due to its potential complications. This study tries to evaluate the association between TPN use and inpatient outcomes in patients hospitalized with severe AH.
Methods: A retrospective cohort study was done using the National Inpatient Sample from 2018 to 2021. Adult patients (≥18 years) hospitalized with a primary diagnosis of AH (ICD-10-CM: K70.1) were included. TPN administration was identified using ICD-10-PCS codes (3E043XZ, 3E053XZ, 3E033XZ). Propensity score matching (1:1 nearest neighbor, caliper 0.05) was performed using demographic, socioeconomic status, Elixhauser comorbidity index and presence of cirrhosis. Average treatment effect on treated (ATT) and weights were generated followed by adjusted analyses using double robust logistic and linear regression.
Results: Of 111,321 AH hospitalizations, 1.73% received TPN. After matching (n=3,344), TPN use was associated with increased in-hospital mortality (aOR:16.99,95%CI:12.86–22.45,p< 0.001). ATT showed a 40.5% absolute mortality increase (45.2% vs. 4.7%,p< 0.001). TPN was also linked to higher odds of sepsis (aOR:12.82,p< 0.001), acute kidney injury (aOR:10.53,p< 0.001), and hepatic encephalopathy (aOR:2.02,p< 0.001). It was further associated with longer length of stay (+5.5 days) and increased hospital charges (+$138,750), both p< 0.001.
Discussion: Our study in this NIS sample shows that TPN use in hospitalized patients with severe AH was strongly associated with worse clinical outcomes, including mortality and major complications such as sepsis, AKI, HE. These findings are consistent with concerns raised in earlier clinical studies regarding infection risk, metabolic stress, and fluid imbalance associated with TPN in liver disease (Cabré et al., 2000; Mendenhall et al., 1995). Although this analysis adjusted for key confounders, limitations remain due to its retrospective nature. Unmeasured factors such as severity of malnutrition, functional status, or contraindications to enteral feeding could influence both treatment selection and the outcomes. Caution should be exercised when considering TPN in severe alcoholic hepatitis patients. More prospective randomized trials are needed to evaluate TPN's safety and efficacy in this high-risk population.
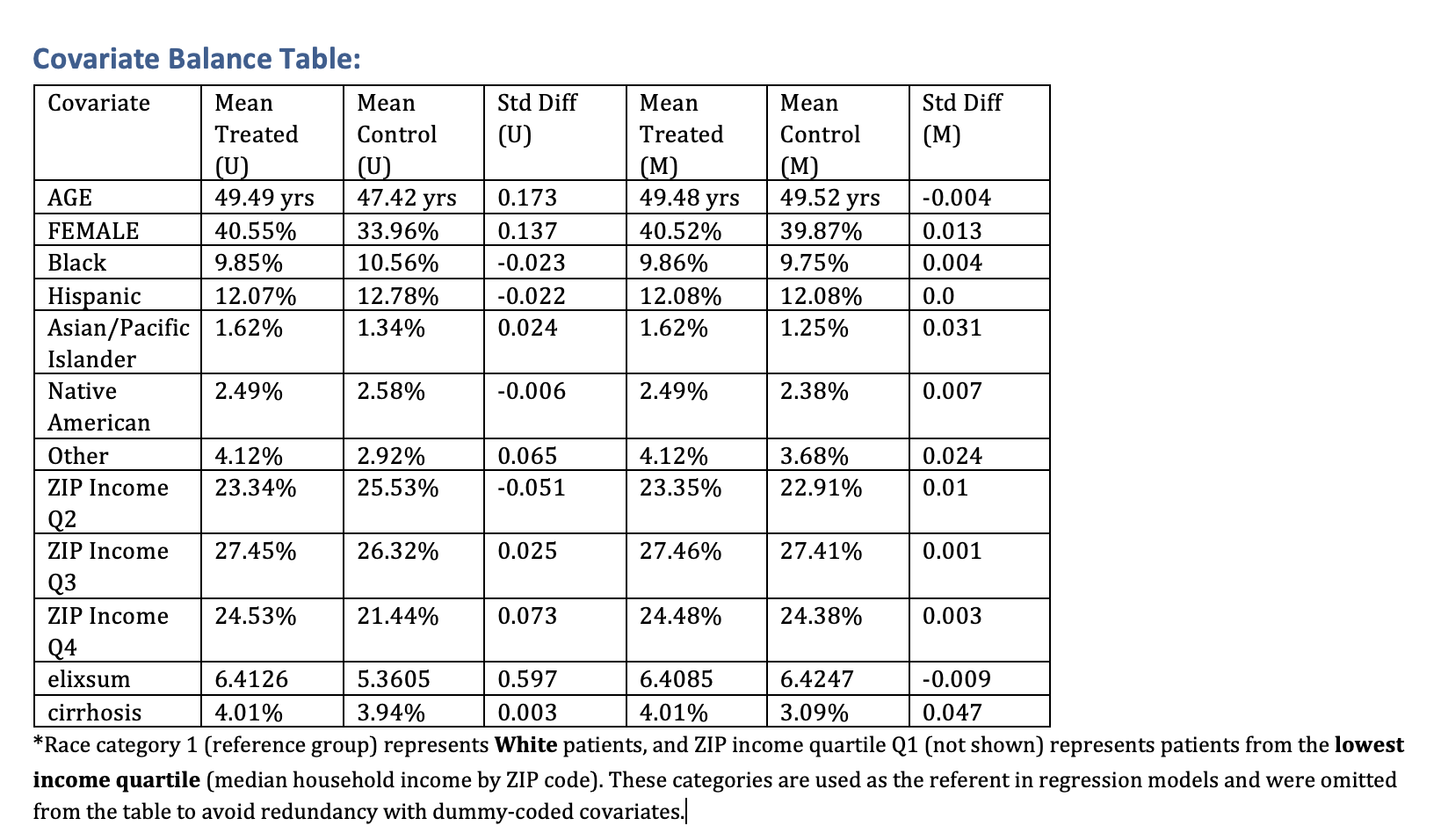
Figure: Covariate Balance Table
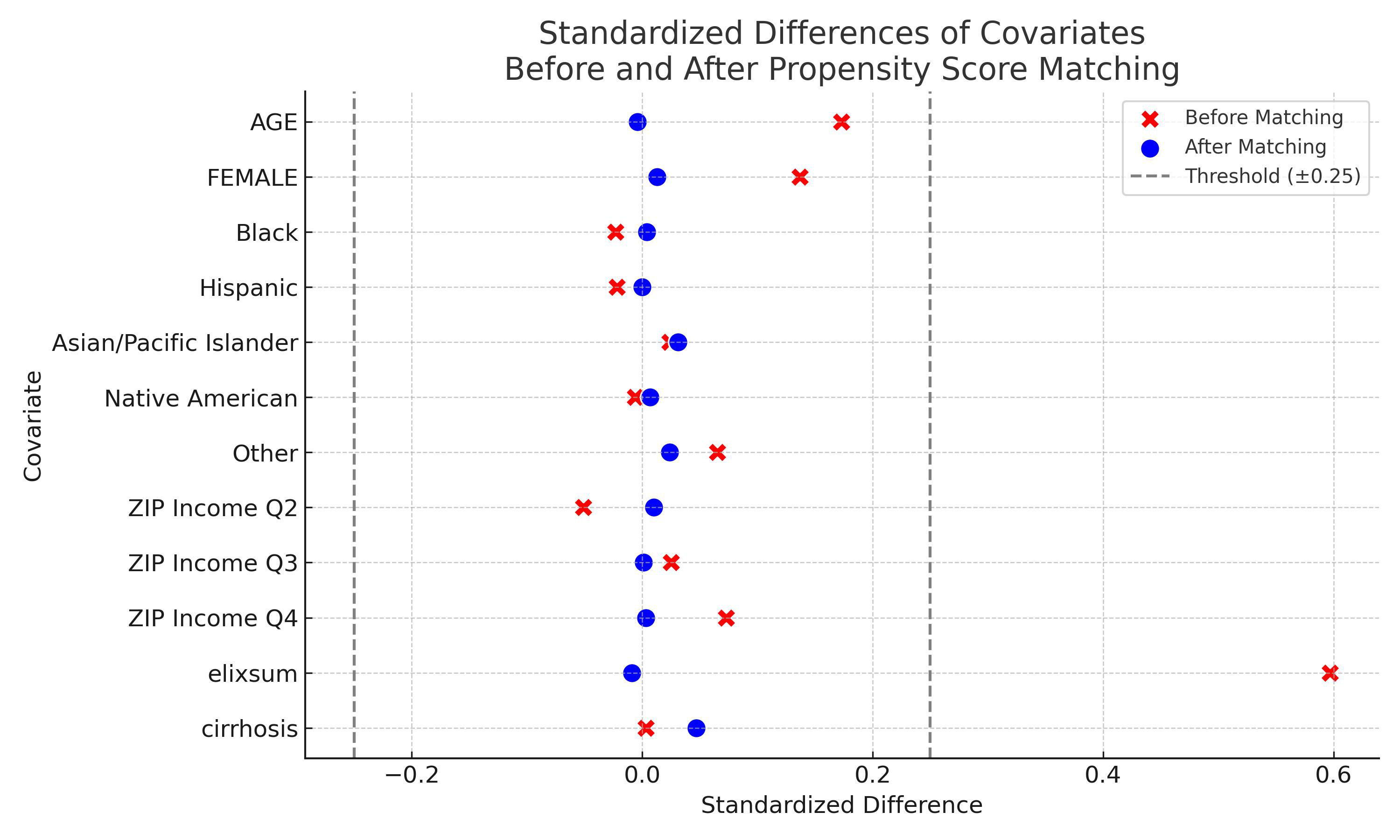
Figure: Standardized Difference Plot Before and After Matching
Disclosures:
Suman Sharma indicated no relevant financial relationships.
Nilisha Regmi indicated no relevant financial relationships.
Uchit Thapa indicated no relevant financial relationships.
Subash Ghimire indicated no relevant financial relationships.
Suman Sharma, MD1, Nilisha Regmi, MD1, Uchit Thapa, MD2, Subash Ghimire, MD3. P0569 - Reevaluating the Role of Parenteral Nutrition in Severe Alcoholic Hepatitis: Insights From a National Inpatient Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Baystate Medical Center, East Longmeadow, MA; 2Baystate Medical Center, Hartford, CT; 3Guthrie Robert Packer Hospital, Department of Gastroenterology, Sayre, PA
Introduction: Severe alcoholic hepatitis (AH) is associated with significant inpatient mortality, especially in malnourished patients. Although nutritional support is important in hospitalized patients, the role of total parenteral nutrition (TPN) remains controversial due to its potential complications. This study tries to evaluate the association between TPN use and inpatient outcomes in patients hospitalized with severe AH.
Methods: A retrospective cohort study was done using the National Inpatient Sample from 2018 to 2021. Adult patients (≥18 years) hospitalized with a primary diagnosis of AH (ICD-10-CM: K70.1) were included. TPN administration was identified using ICD-10-PCS codes (3E043XZ, 3E053XZ, 3E033XZ). Propensity score matching (1:1 nearest neighbor, caliper 0.05) was performed using demographic, socioeconomic status, Elixhauser comorbidity index and presence of cirrhosis. Average treatment effect on treated (ATT) and weights were generated followed by adjusted analyses using double robust logistic and linear regression.
Results: Of 111,321 AH hospitalizations, 1.73% received TPN. After matching (n=3,344), TPN use was associated with increased in-hospital mortality (aOR:16.99,95%CI:12.86–22.45,p< 0.001). ATT showed a 40.5% absolute mortality increase (45.2% vs. 4.7%,p< 0.001). TPN was also linked to higher odds of sepsis (aOR:12.82,p< 0.001), acute kidney injury (aOR:10.53,p< 0.001), and hepatic encephalopathy (aOR:2.02,p< 0.001). It was further associated with longer length of stay (+5.5 days) and increased hospital charges (+$138,750), both p< 0.001.
Discussion: Our study in this NIS sample shows that TPN use in hospitalized patients with severe AH was strongly associated with worse clinical outcomes, including mortality and major complications such as sepsis, AKI, HE. These findings are consistent with concerns raised in earlier clinical studies regarding infection risk, metabolic stress, and fluid imbalance associated with TPN in liver disease (Cabré et al., 2000; Mendenhall et al., 1995). Although this analysis adjusted for key confounders, limitations remain due to its retrospective nature. Unmeasured factors such as severity of malnutrition, functional status, or contraindications to enteral feeding could influence both treatment selection and the outcomes. Caution should be exercised when considering TPN in severe alcoholic hepatitis patients. More prospective randomized trials are needed to evaluate TPN's safety and efficacy in this high-risk population.
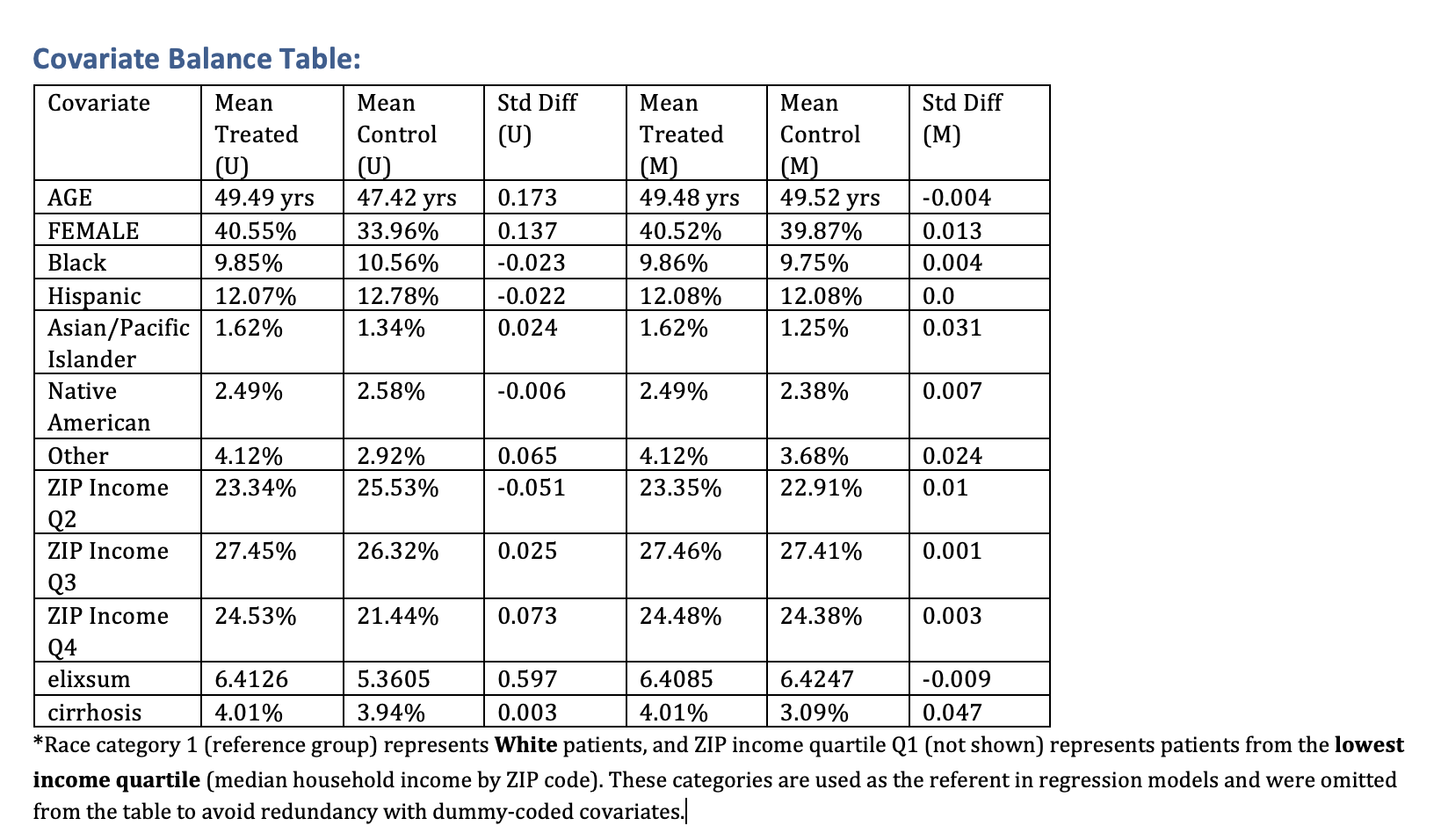
Figure: Covariate Balance Table
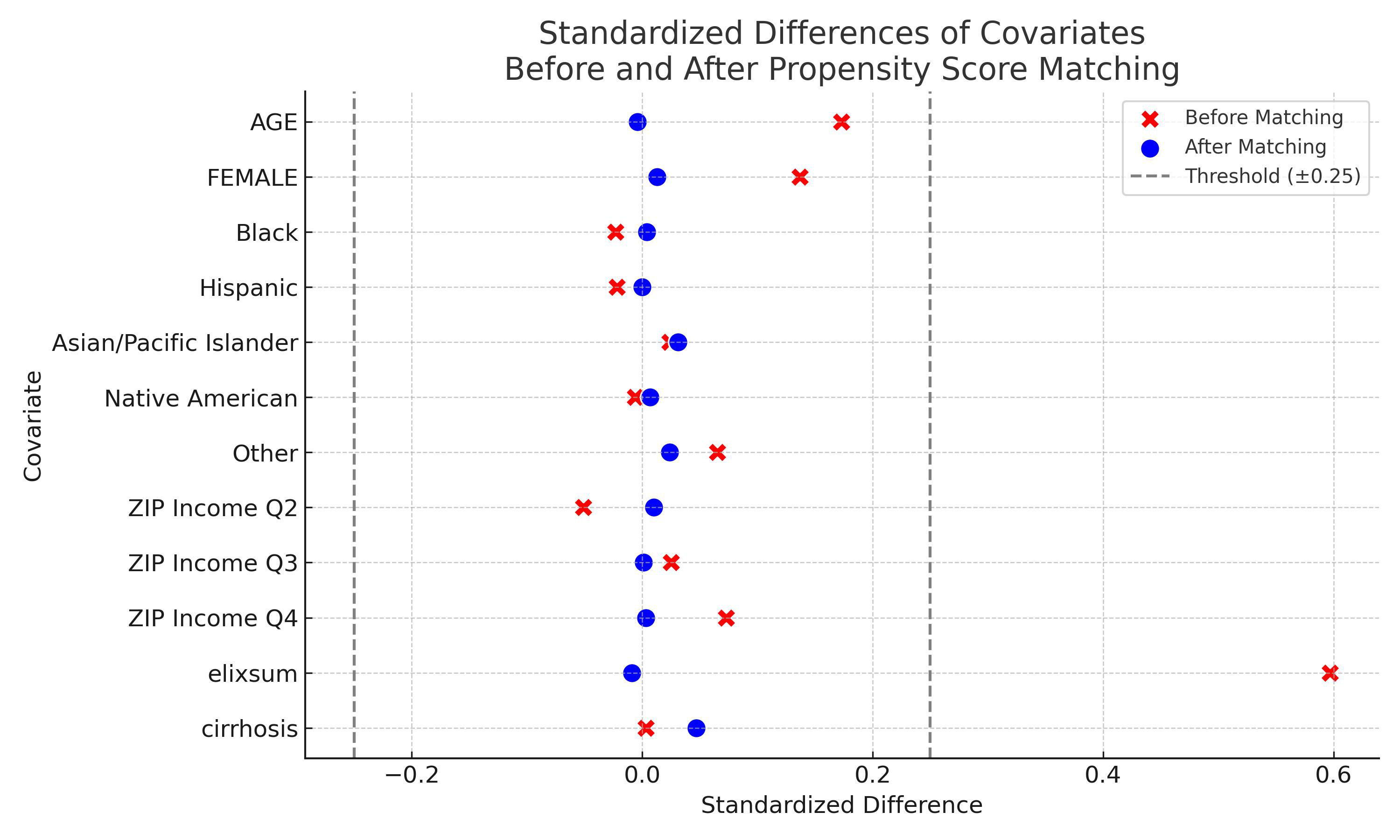
Figure: Standardized Difference Plot Before and After Matching
Disclosures:
Suman Sharma indicated no relevant financial relationships.
Nilisha Regmi indicated no relevant financial relationships.
Uchit Thapa indicated no relevant financial relationships.
Subash Ghimire indicated no relevant financial relationships.
Suman Sharma, MD1, Nilisha Regmi, MD1, Uchit Thapa, MD2, Subash Ghimire, MD3. P0569 - Reevaluating the Role of Parenteral Nutrition in Severe Alcoholic Hepatitis: Insights From a National Inpatient Cohort, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
