Sunday Poster Session
Category: Diet, Nutrition, and Obesity
P0549 - Assessing the Risk of Recurrent Pancreatitis in Patients on GLP-1 Agonists
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
.jpg)
Arvind Bussetty, MD (he/him/his)
Rutgers Robert Wood Johnson Medical School
New Brunswick, NJ
Presenting Author(s)
Arvind Bussetty, MD1, Debra Scheiner, BA1, Nikhil Reddy, MD1, Andrew A. Wang, MD2, Alexander Chen, MD1, Keerthana Kesavarapu, MD1
1Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1RAs) are utilized in the management of type 2 diabetes (T2DM) and obesity. While these agents have been implicated in the development of acute pancreatitis, most large-scale randomized control trials and meta-analyses have not found a statistically significant increased risk of AP in patients without a history of prior AP. This study aims to characterize the clinical features and potential risk factors associated with recurrent acute pancreatitis in patients initiated on GLP-1RA therapy.
Methods: This retrospective cohort study identified patients with a diagnosis of acute pancreatitis (AP) who were subsequently prescribed a GLP-1 receptor agonist (GLP-1RA) prior to 3/15/2024. The primary outcome was recurrent acute pancreatitis (RAP), defined as any AP episode occurring after GLP-1RA initiation. Variables analyzed included patient demographics, body mass index, suspected etiology of the initial AP episode, time interval from GLP-1RA initiation to RAP, diabetes status, and peak lipase levels during the initial AP episode. We employed Fisher's exact test to compare baseline characteristics between patients with and without RAP, and logistic regression to determine odds ratios and identify independent risk factors associated with RAP development.
Results: Of the 131 patients, 16 (12.2%) experienced recurrent pancreatitis after starting GLP-1RA therapy. Patients with recurrence had a mean age of 58.8 years and were on GLP-1RAs for a mean duration of 23.6 months. In univariate analysis, age < 65 years was significantly associated with recurrence (OR 5.78, 95% CI: 1.26–26.59). In multivariable logistic regression adjusting for sex, BMI, T2DM status, lipase level, duration of GLP-1RA exposure, and pancreatitis etiology, age < 65 remained an independent predictor of recurrence (adjusted OR 8.05, 95% CI: 1.30–50.08). No other variables were significantly associated with recurrence in the adjusted model.
Discussion: In this cohort of patients with prior pancreatitis, recurrence after GLP-1RA initiation was uncommon. Younger age (< 65 years) was significantly associated with increased odds of recurrence, even after adjusting for relevant covariates. These findings underscore the importance of cautious use and close monitoring of GLP-1RAs in younger patients with a history of pancreatitis.
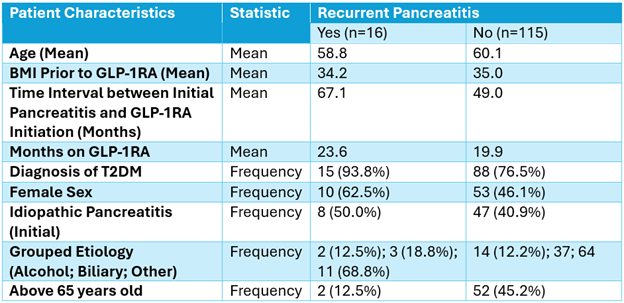
Figure: Comparing Characteristics Between Patients with and without Recurrent Pancreatitis after GLP-1RA
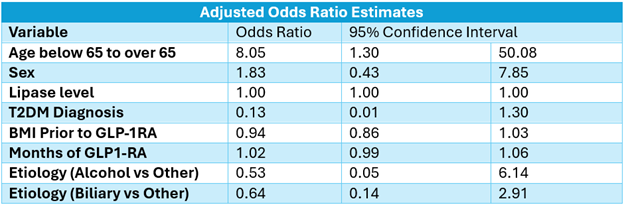
Figure: Adjusted Odds Ratio Estimations of Variables Influencing Recurrent Pancreatitis
Disclosures:
Arvind Bussetty indicated no relevant financial relationships.
Debra Scheiner indicated no relevant financial relationships.
Nikhil Reddy indicated no relevant financial relationships.
Andrew Wang indicated no relevant financial relationships.
Alexander Chen indicated no relevant financial relationships.
Keerthana Kesavarapu indicated no relevant financial relationships.
Arvind Bussetty, MD1, Debra Scheiner, BA1, Nikhil Reddy, MD1, Andrew A. Wang, MD2, Alexander Chen, MD1, Keerthana Kesavarapu, MD1. P0549 - Assessing the Risk of Recurrent Pancreatitis in Patients on GLP-1 Agonists, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Robert Wood Johnson Medical School, Rutgers University, New Brunswick, NJ
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1RAs) are utilized in the management of type 2 diabetes (T2DM) and obesity. While these agents have been implicated in the development of acute pancreatitis, most large-scale randomized control trials and meta-analyses have not found a statistically significant increased risk of AP in patients without a history of prior AP. This study aims to characterize the clinical features and potential risk factors associated with recurrent acute pancreatitis in patients initiated on GLP-1RA therapy.
Methods: This retrospective cohort study identified patients with a diagnosis of acute pancreatitis (AP) who were subsequently prescribed a GLP-1 receptor agonist (GLP-1RA) prior to 3/15/2024. The primary outcome was recurrent acute pancreatitis (RAP), defined as any AP episode occurring after GLP-1RA initiation. Variables analyzed included patient demographics, body mass index, suspected etiology of the initial AP episode, time interval from GLP-1RA initiation to RAP, diabetes status, and peak lipase levels during the initial AP episode. We employed Fisher's exact test to compare baseline characteristics between patients with and without RAP, and logistic regression to determine odds ratios and identify independent risk factors associated with RAP development.
Results: Of the 131 patients, 16 (12.2%) experienced recurrent pancreatitis after starting GLP-1RA therapy. Patients with recurrence had a mean age of 58.8 years and were on GLP-1RAs for a mean duration of 23.6 months. In univariate analysis, age < 65 years was significantly associated with recurrence (OR 5.78, 95% CI: 1.26–26.59). In multivariable logistic regression adjusting for sex, BMI, T2DM status, lipase level, duration of GLP-1RA exposure, and pancreatitis etiology, age < 65 remained an independent predictor of recurrence (adjusted OR 8.05, 95% CI: 1.30–50.08). No other variables were significantly associated with recurrence in the adjusted model.
Discussion: In this cohort of patients with prior pancreatitis, recurrence after GLP-1RA initiation was uncommon. Younger age (< 65 years) was significantly associated with increased odds of recurrence, even after adjusting for relevant covariates. These findings underscore the importance of cautious use and close monitoring of GLP-1RAs in younger patients with a history of pancreatitis.
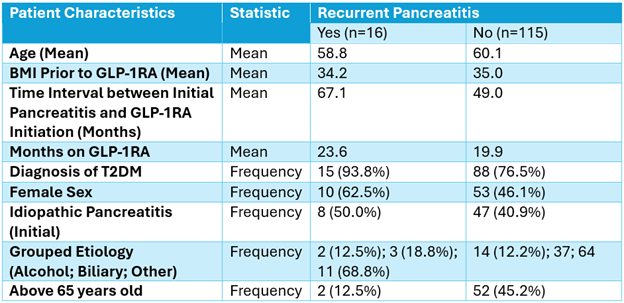
Figure: Comparing Characteristics Between Patients with and without Recurrent Pancreatitis after GLP-1RA
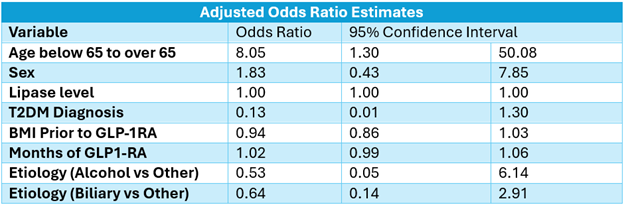
Figure: Adjusted Odds Ratio Estimations of Variables Influencing Recurrent Pancreatitis
Disclosures:
Arvind Bussetty indicated no relevant financial relationships.
Debra Scheiner indicated no relevant financial relationships.
Nikhil Reddy indicated no relevant financial relationships.
Andrew Wang indicated no relevant financial relationships.
Alexander Chen indicated no relevant financial relationships.
Keerthana Kesavarapu indicated no relevant financial relationships.
Arvind Bussetty, MD1, Debra Scheiner, BA1, Nikhil Reddy, MD1, Andrew A. Wang, MD2, Alexander Chen, MD1, Keerthana Kesavarapu, MD1. P0549 - Assessing the Risk of Recurrent Pancreatitis in Patients on GLP-1 Agonists, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
