Sunday Poster Session
Category: Colorectal Cancer Prevention
P0523 - Accuracy of Visual Prediction of Colorectal Polyp Pathology in a Real-World Setting
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- JA
Jayati Anand, MD
Beth Israel Deaconess Medical Center
Boston, MA
Presenting Author(s)
Jayati Anand, MD1, Yuvaraj Singh, MD2, Curuchi Anand, MD3, Maya Gogtay, MD4
1Beth Israel Deaconess Medical Center, Boston, MA; 2University of Massachusetts, Worcester, MA; 3St. Vincent Hospital, Worcester, MA; 4University of Nebraska Medical Center, Omaha, NE
Introduction: Predicting the histology of colon polyps during colonoscopy using real-time visual assessment has clinical relevance. Accurate characterization guides immediate clinical decisions, like the need for polypectomy, and reduces unnecessary procedures, risks and costs. Traditionally, polyps are classified by histopathology, but emerging tools, including artificial intelligence, offer real-time, non-invasive characterization. Experienced gastroenterologists can make accurate predictions without these tools. The purpose of this study was to determine the accuracy of visual prediction of colon polyp pathology in a community based colonoscopy setting.
Methods: Consecutive patients undergoing screening or surveillance colonoscopy at a community hospital with identified polyps over two months were included. Visually predicted pathology on white light (WL) and narrow band imaging (NBI) was recorded. Histopathology results were then reviewed to confirm polyp pathology. Predicted and confirmed pathologies were compared. Colonoscopies were performed with Olympus PCF HQ190L colonoscopes.
Results: The 197 patients had a total of 238 polyps. Final pathology classification included hyperplastic polyps, tubular adenomas, and sessile serrated adenomas. WL and NBI predictions were compared to histopathology. Identification of tubular adenomas had AUROC values of 0.92 (NBI) and 0.91 (WL) and sensitivity/specificity of 0.91/0.92 (NBI) and 0.88/0.94 (WL). For hyperplastic polyps, AUROCs were 0.88 (NBI) and 0.87 (WL), with sensitivity/specificity of 0.81/0.95 (NBI) and 0.82/0.93 (WL). Sessile serrated adenomas were identified with AUROCs of 0.84 (NBI) and 0.78 (WL) and sensitivity/specificity of 0.73/0.94 (NBI) and 0.67/0.92 (WL). Chi-square analysis confirmed statistical significance between both modalities and final pathology (p< 0.001 for WL and NBI).
Discussion: These results demonstrate that experienced gastroenterologists can use real-time visual assessment to achieve high diagnostic accuracy in polyp characterization across all major histological types. When compared to recent AI-based systems, which report AUROC values between 0.83–0.94, these results show that trained endoscopists perform on par with or even exceed the precision of machine learning tools. This study reinforces the enduring value of endoscopic expertise and supports the continued emphasis on training and visual recognition skills among gastroenterologists.
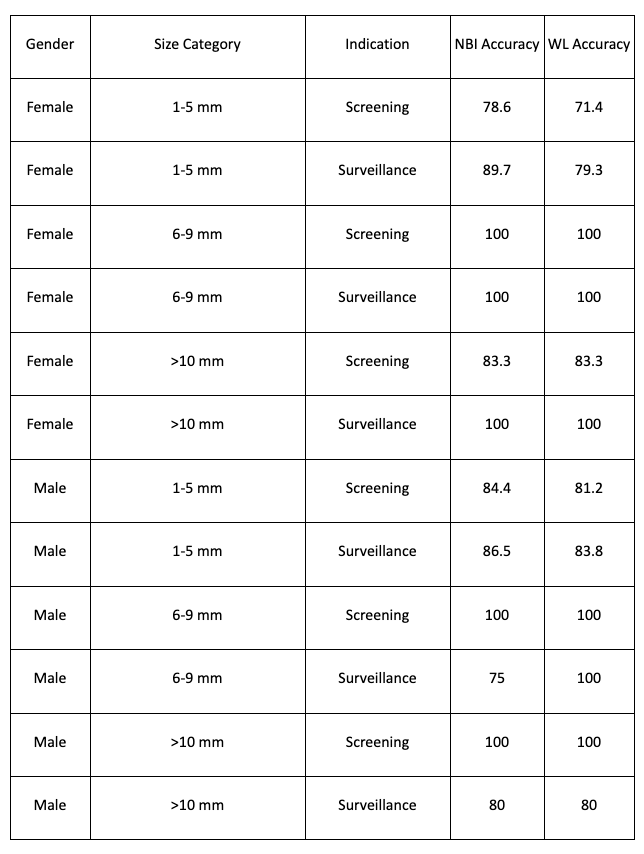
Figure: Accuracy of prediction by Pathology Type and Modality
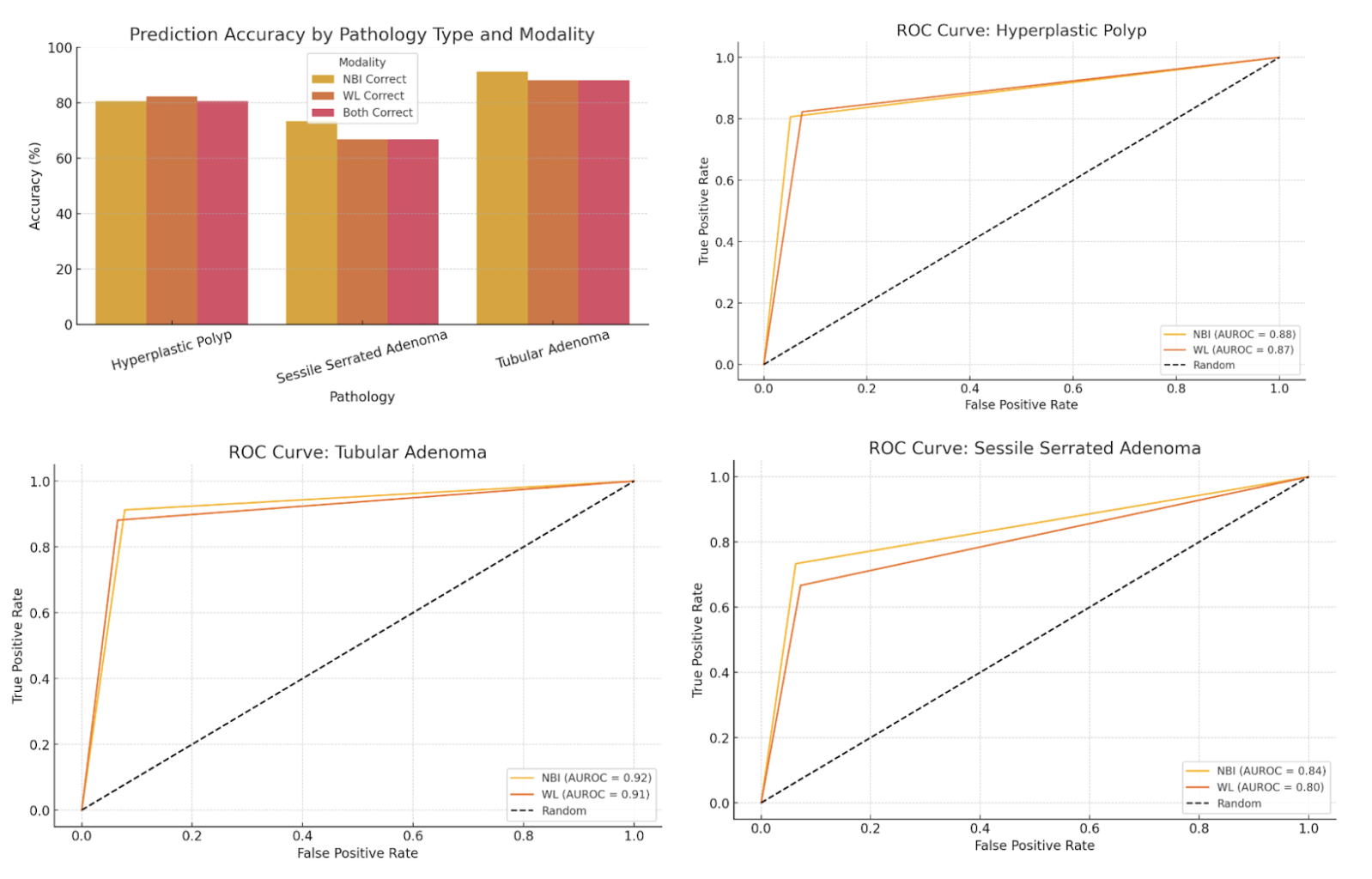
Figure: Accuracy of prediction by Polyp Size and Indication
Disclosures:
Jayati Anand indicated no relevant financial relationships.
Yuvaraj Singh indicated no relevant financial relationships.
Curuchi Anand indicated no relevant financial relationships.
Maya Gogtay indicated no relevant financial relationships.
Jayati Anand, MD1, Yuvaraj Singh, MD2, Curuchi Anand, MD3, Maya Gogtay, MD4. P0523 - Accuracy of Visual Prediction of Colorectal Polyp Pathology in a Real-World Setting, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Beth Israel Deaconess Medical Center, Boston, MA; 2University of Massachusetts, Worcester, MA; 3St. Vincent Hospital, Worcester, MA; 4University of Nebraska Medical Center, Omaha, NE
Introduction: Predicting the histology of colon polyps during colonoscopy using real-time visual assessment has clinical relevance. Accurate characterization guides immediate clinical decisions, like the need for polypectomy, and reduces unnecessary procedures, risks and costs. Traditionally, polyps are classified by histopathology, but emerging tools, including artificial intelligence, offer real-time, non-invasive characterization. Experienced gastroenterologists can make accurate predictions without these tools. The purpose of this study was to determine the accuracy of visual prediction of colon polyp pathology in a community based colonoscopy setting.
Methods: Consecutive patients undergoing screening or surveillance colonoscopy at a community hospital with identified polyps over two months were included. Visually predicted pathology on white light (WL) and narrow band imaging (NBI) was recorded. Histopathology results were then reviewed to confirm polyp pathology. Predicted and confirmed pathologies were compared. Colonoscopies were performed with Olympus PCF HQ190L colonoscopes.
Results: The 197 patients had a total of 238 polyps. Final pathology classification included hyperplastic polyps, tubular adenomas, and sessile serrated adenomas. WL and NBI predictions were compared to histopathology. Identification of tubular adenomas had AUROC values of 0.92 (NBI) and 0.91 (WL) and sensitivity/specificity of 0.91/0.92 (NBI) and 0.88/0.94 (WL). For hyperplastic polyps, AUROCs were 0.88 (NBI) and 0.87 (WL), with sensitivity/specificity of 0.81/0.95 (NBI) and 0.82/0.93 (WL). Sessile serrated adenomas were identified with AUROCs of 0.84 (NBI) and 0.78 (WL) and sensitivity/specificity of 0.73/0.94 (NBI) and 0.67/0.92 (WL). Chi-square analysis confirmed statistical significance between both modalities and final pathology (p< 0.001 for WL and NBI).
Discussion: These results demonstrate that experienced gastroenterologists can use real-time visual assessment to achieve high diagnostic accuracy in polyp characterization across all major histological types. When compared to recent AI-based systems, which report AUROC values between 0.83–0.94, these results show that trained endoscopists perform on par with or even exceed the precision of machine learning tools. This study reinforces the enduring value of endoscopic expertise and supports the continued emphasis on training and visual recognition skills among gastroenterologists.
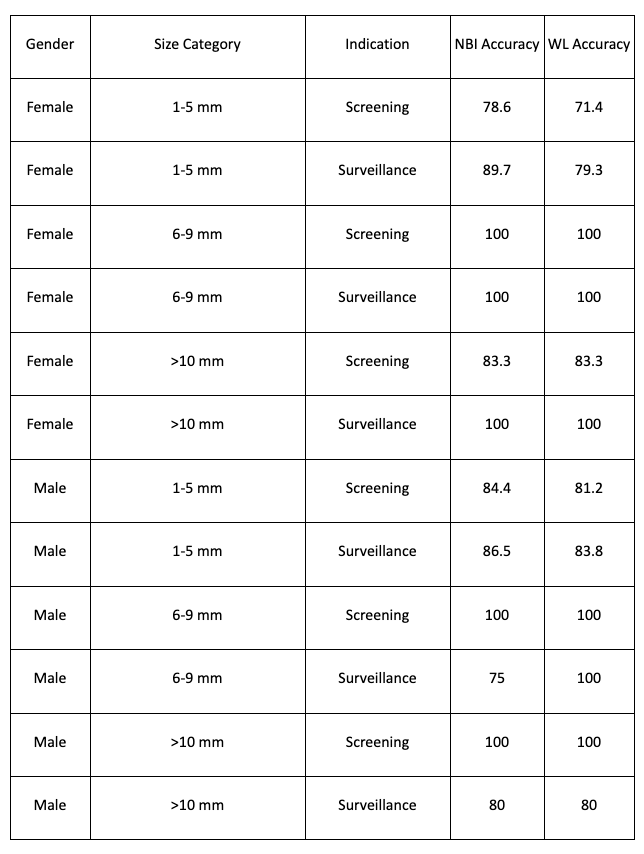
Figure: Accuracy of prediction by Pathology Type and Modality
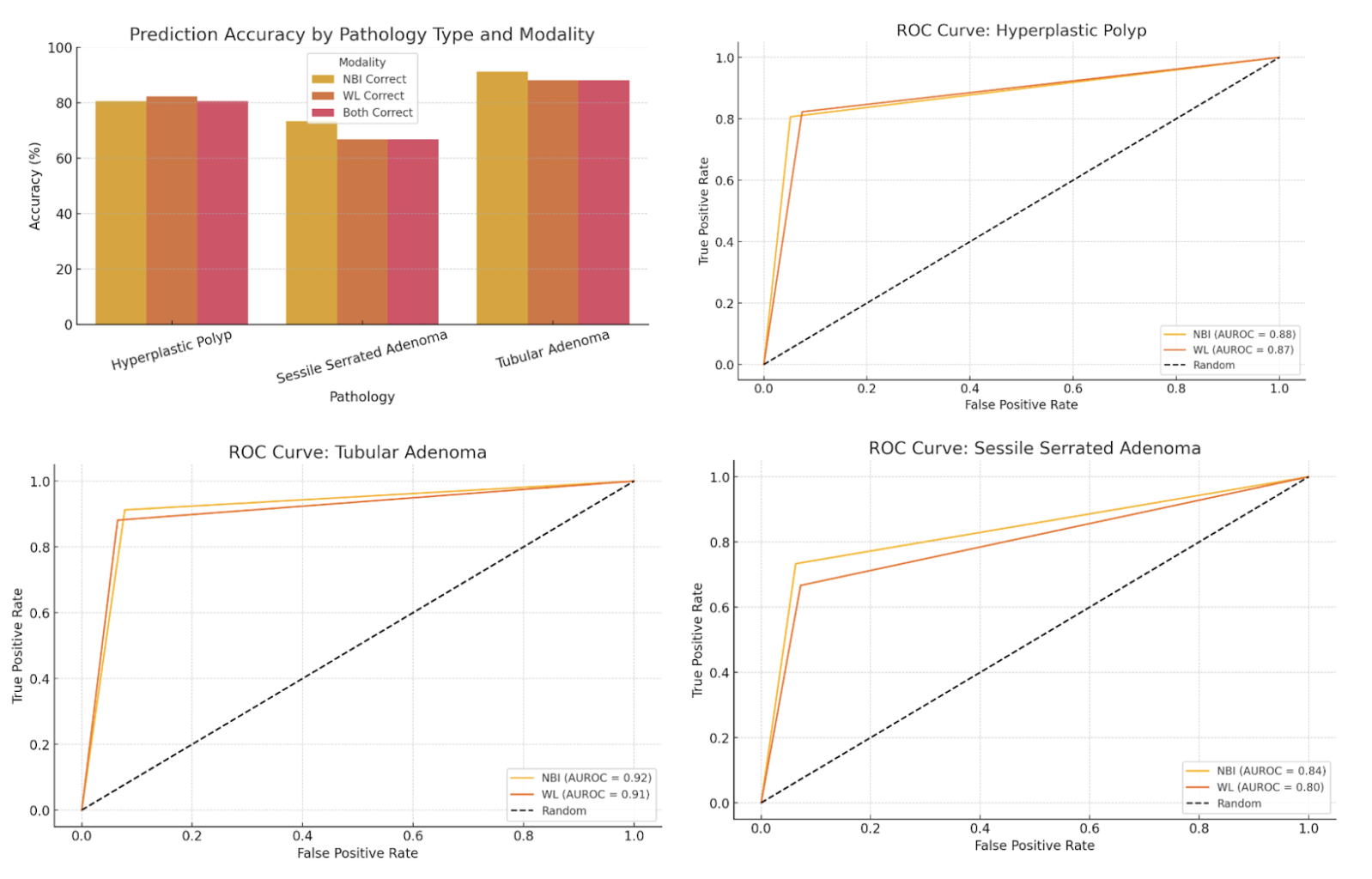
Figure: Accuracy of prediction by Polyp Size and Indication
Disclosures:
Jayati Anand indicated no relevant financial relationships.
Yuvaraj Singh indicated no relevant financial relationships.
Curuchi Anand indicated no relevant financial relationships.
Maya Gogtay indicated no relevant financial relationships.
Jayati Anand, MD1, Yuvaraj Singh, MD2, Curuchi Anand, MD3, Maya Gogtay, MD4. P0523 - Accuracy of Visual Prediction of Colorectal Polyp Pathology in a Real-World Setting, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
