Sunday Poster Session
Category: Colorectal Cancer Prevention
P0497 - Boston Bowel Prep Scores of Individual Gastroenterologists and Polyp Detection in the Endoscopy Suite
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall
- PN
Paul Naylor, PhD
Wayne State School of Medicine
Detroit, MI
Presenting Author(s)
Sophie Turner, BS1, Esha Garg, BS1, Ali Mustapha, BS1, Eric Denha, MD1, Bashar Mohamad, MD2, Paul Naylor, PhD1
1Wayne State School of Medicine, Detroit, MI; 2Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI
Introduction: The Boston Bowel Prep Score (BBPS) evaluates bowel preparation by scoring it in three segments providing a more quantitative scoring system. The impact of potential variation in scoring by individual endoscopists and whether a strict definition of < 6 as the definition of a poor prep is valid remains a subject of debate. This study compares the BBPS scores of individual GI endoscopists and total polyp detection with respect to defining a cutoff in a predominantly African American population (82%).
Methods: Using the electronic medical records for patients undergoing screening colonoscopies we identified 132 patients with BBPS seen by 8 GI attendings (identified as A1-A8). Three categories of BBPS were used in this study: Excellent (9-7), Good (6-5) and Poor (4-3). The EMR was used to identify the number of polyps identified in each colonoscopy as well as the number of polyps per bowel segment.
Results: The population was primary African American (84%), female (64% ) and the average age was 60 years. Most patients had a BBPS score of 9 (64%), while only 10% had scores between 5-3. When evaluated for the score that generated significant numbers of polyps detected, 4-3 were worse (16%) as compared to both 6-5 (80%) and 9-7 (60%). There was a modest but significant difference (p=0.02) between the BBPS scoring of the 8 Colonoscopist (Figure 1). The primary variation was the number of patients with scores of 6-5. When total polyps detected and BBPS were evaluated, there was no correlation between the BBPS scores and the number of polyps detected per colonoscopy (Figure 1 and 2). This was also true when expressed as polyp detection ratio (i.e. colonoscopies with at least 1 polyp). When polyp location was identified by each of the five areas (cecal, ascending, transverse, descending, sigmoid or rectum), the only significant variability between the individual gastroenterologists and detection of polyps was the descending colon (p=0.002).
Discussion: This study demonstrates potential variation between the scoring of patient bowel preparations by gastroenterologists using the Boston Bowel Prep Score especially in the intermediate area (5-9). There was however no correlation between the scores and the detection of polyps. While our data confirms that very poor bowel preparation (3-4) results in lower polyp detection, it does suggest that it may be difficult to define a rigid cutoff for BBPS as < 6 aa compared to a more rigorous score of < 5.
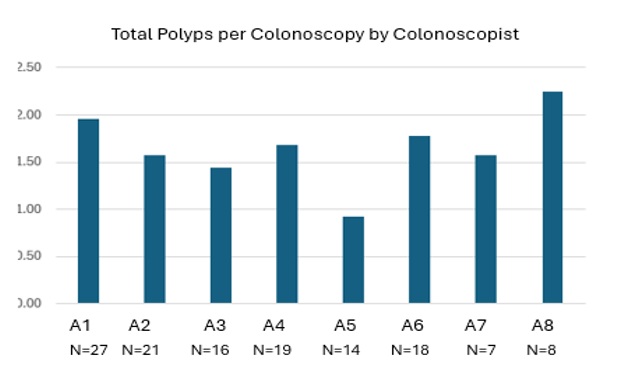
Figure: Figure 1 Boston Bowel Preparation Score is presented for each of 8 Colonoscopists. The three categories are Excellent (7-9), Good (5-6) or Poor (3-4). The variation is significant a p<0.05
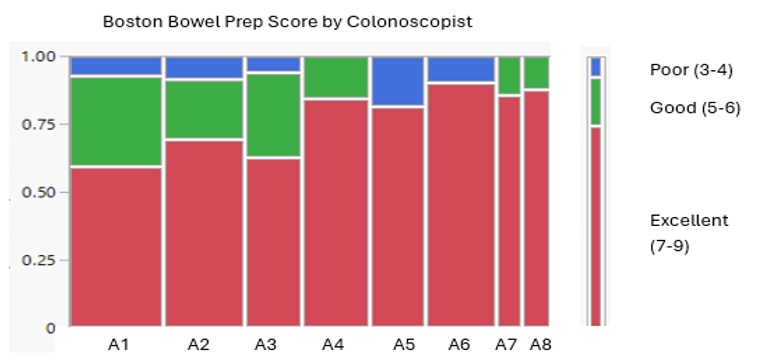
Figure: Figure 2 Polyp detection per colonoscopy is plotted for each colonoscopist (labeled A1-A8). The number of patients is below the label. There was no significant difference between the polyps per colonoscopy and there was no correlation between the polyps detected and the BPS scores as depicted in Figure 1).
Disclosures:
Sophie Turner indicated no relevant financial relationships.
Esha Garg indicated no relevant financial relationships.
Ali Mustapha indicated no relevant financial relationships.
Eric Denha indicated no relevant financial relationships.
Bashar Mohamad indicated no relevant financial relationships.
Paul Naylor: Janssen Biotech Inc – Grant/Research Support. Salix Pharmaceuticals – Grant/Research Support.
Sophie Turner, BS1, Esha Garg, BS1, Ali Mustapha, BS1, Eric Denha, MD1, Bashar Mohamad, MD2, Paul Naylor, PhD1. P0497 - Boston Bowel Prep Scores of Individual Gastroenterologists and Polyp Detection in the Endoscopy Suite, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Wayne State School of Medicine, Detroit, MI; 2Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI
Introduction: The Boston Bowel Prep Score (BBPS) evaluates bowel preparation by scoring it in three segments providing a more quantitative scoring system. The impact of potential variation in scoring by individual endoscopists and whether a strict definition of < 6 as the definition of a poor prep is valid remains a subject of debate. This study compares the BBPS scores of individual GI endoscopists and total polyp detection with respect to defining a cutoff in a predominantly African American population (82%).
Methods: Using the electronic medical records for patients undergoing screening colonoscopies we identified 132 patients with BBPS seen by 8 GI attendings (identified as A1-A8). Three categories of BBPS were used in this study: Excellent (9-7), Good (6-5) and Poor (4-3). The EMR was used to identify the number of polyps identified in each colonoscopy as well as the number of polyps per bowel segment.
Results: The population was primary African American (84%), female (64% ) and the average age was 60 years. Most patients had a BBPS score of 9 (64%), while only 10% had scores between 5-3. When evaluated for the score that generated significant numbers of polyps detected, 4-3 were worse (16%) as compared to both 6-5 (80%) and 9-7 (60%). There was a modest but significant difference (p=0.02) between the BBPS scoring of the 8 Colonoscopist (Figure 1). The primary variation was the number of patients with scores of 6-5. When total polyps detected and BBPS were evaluated, there was no correlation between the BBPS scores and the number of polyps detected per colonoscopy (Figure 1 and 2). This was also true when expressed as polyp detection ratio (i.e. colonoscopies with at least 1 polyp). When polyp location was identified by each of the five areas (cecal, ascending, transverse, descending, sigmoid or rectum), the only significant variability between the individual gastroenterologists and detection of polyps was the descending colon (p=0.002).
Discussion: This study demonstrates potential variation between the scoring of patient bowel preparations by gastroenterologists using the Boston Bowel Prep Score especially in the intermediate area (5-9). There was however no correlation between the scores and the detection of polyps. While our data confirms that very poor bowel preparation (3-4) results in lower polyp detection, it does suggest that it may be difficult to define a rigid cutoff for BBPS as < 6 aa compared to a more rigorous score of < 5.
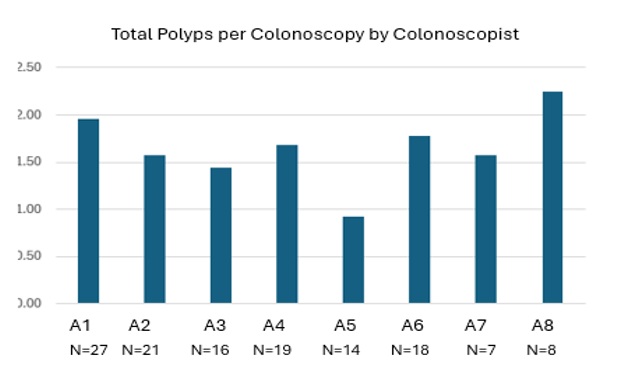
Figure: Figure 1 Boston Bowel Preparation Score is presented for each of 8 Colonoscopists. The three categories are Excellent (7-9), Good (5-6) or Poor (3-4). The variation is significant a p<0.05
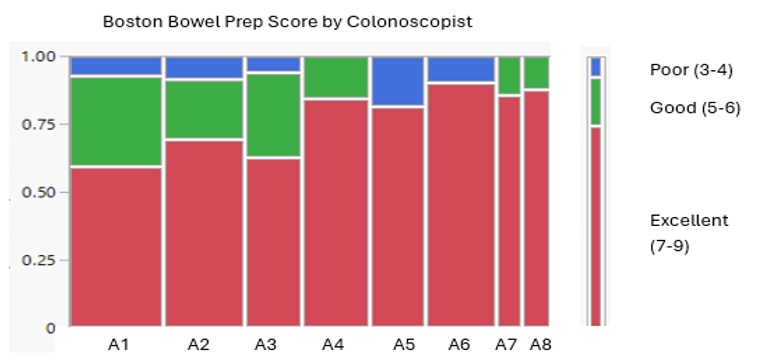
Figure: Figure 2 Polyp detection per colonoscopy is plotted for each colonoscopist (labeled A1-A8). The number of patients is below the label. There was no significant difference between the polyps per colonoscopy and there was no correlation between the polyps detected and the BPS scores as depicted in Figure 1).
Disclosures:
Sophie Turner indicated no relevant financial relationships.
Esha Garg indicated no relevant financial relationships.
Ali Mustapha indicated no relevant financial relationships.
Eric Denha indicated no relevant financial relationships.
Bashar Mohamad indicated no relevant financial relationships.
Paul Naylor: Janssen Biotech Inc – Grant/Research Support. Salix Pharmaceuticals – Grant/Research Support.
Sophie Turner, BS1, Esha Garg, BS1, Ali Mustapha, BS1, Eric Denha, MD1, Bashar Mohamad, MD2, Paul Naylor, PhD1. P0497 - Boston Bowel Prep Scores of Individual Gastroenterologists and Polyp Detection in the Endoscopy Suite, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
