Sunday Poster Session
Category: Colorectal Cancer Prevention
P0493 - Is Artificial Intelligence Cost-Effective in Colonoscopy? A Systematic Review and Meta-Analysis of Economic Evaluations and Modeling Studies
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Arashdeep Singh Singh, MBBS (he/him/his)
Government Medical College and Hospital
Amritsar, Punjab, India
Presenting Author(s)
Arashdeep Singh Singh, MBBS1, Sarthak Sharma, MBBS2, Shahdil Khusroo, 3
1Government Medical College and Hospital, Amritsar, Punjab, India; 2Government Medical College, Jammu, Jammu, Jammu and Kashmir, India; 3BHARAT RATNA LATE SHRI ATAL BIHARI VAJPAYEE MEMORIAL MEDICAL COLLEGE , RAJNANDGAON, CHHATTISGARH, Rajnandgaon, Chhattisgarh, India
Introduction: Artificial intelligence (AI) is increasingly being used to enhance colonoscopy and improve adenoma detection rates (ADRs), potentially lowering colorectal cancer (CRC) incidence. However, its cost-effectiveness remains unclear. We conducted a systematic review and meta-analysis to assess whether AI-assisted colonoscopy is a cost-effective or cost-saving strategy across different healthcare systems.
Methods: A systematic literature search was conducted across six databases: PubMed (MEDLINE), Google Scholar, ScienceDirect, PLOS ONE, Cochrane Library, and ClinicalTrials.gov. Studies comparing AI-assisted colonoscopy to standard colonoscopy were included. Outcomes of interest included incremental cost-effectiveness ratios (ICERs), net monetary benefit (NMB), and other modeled cost and effectiveness measures. Data were standardized to USD where applicable and pooled using a random-effects meta-analysis. Risk of bias was assessed using the Philips</span> <span style="font-size: 11pt; font-family: Arial,sans-serif; color: #000000; background-color: transparent; font-weight: 400; font-style: normal; font-variant: normal; text-decoration: none; vertical-align: baseline; white-space: pre-wrap;">checklist for modeling studies. A forest plot and cost-effectiveness plane were constructed to visualize study results in relation to a $50,000/QALY willingness-to-pay threshold using RStudio (Version 2025.05.0+496).
Results: Nine studies were included, seven of which reported ICER or NMB values and were synthesized quantitatively. The pooled net monetary benefit was $1,300 (95% CI: $786–$1,814; p < 0.001), supporting the cost-effectiveness of AI-assisted colonoscopy. Heterogeneity was high (I² = 87.7%) due to variations in model design and healthcare settings. All studies fell within the cost-effective or dominant quadrants of the cost-effectiveness plane. Bustamante-Balén et al. and Barkun et al. showed dominant strategies, while Yu et al. and Hassan et al. reported favorable ICERs below $50,000/QALY. Two studies were assessed qualitatively: Mori et al. reported cost savings using a “diagnose-and-leave” strategy; Halvorsen et al. noted increased surveillance burden despite marginal cancer risk reduction.
Discussion: AI-assisted colonoscopy was consistently cost-effective, with several studies demonstrating dominant strategies. Despite substantial heterogeneity, all studies fell within the cost-effective or dominant regions of the cost-effectiveness plane. Integration into clinical practice should balance potential cost savings with the implications of increased surveillance burden. As current evidence is primarily based on modeling studies, cautious implementation and further validation in diverse real-world settings are warranted.
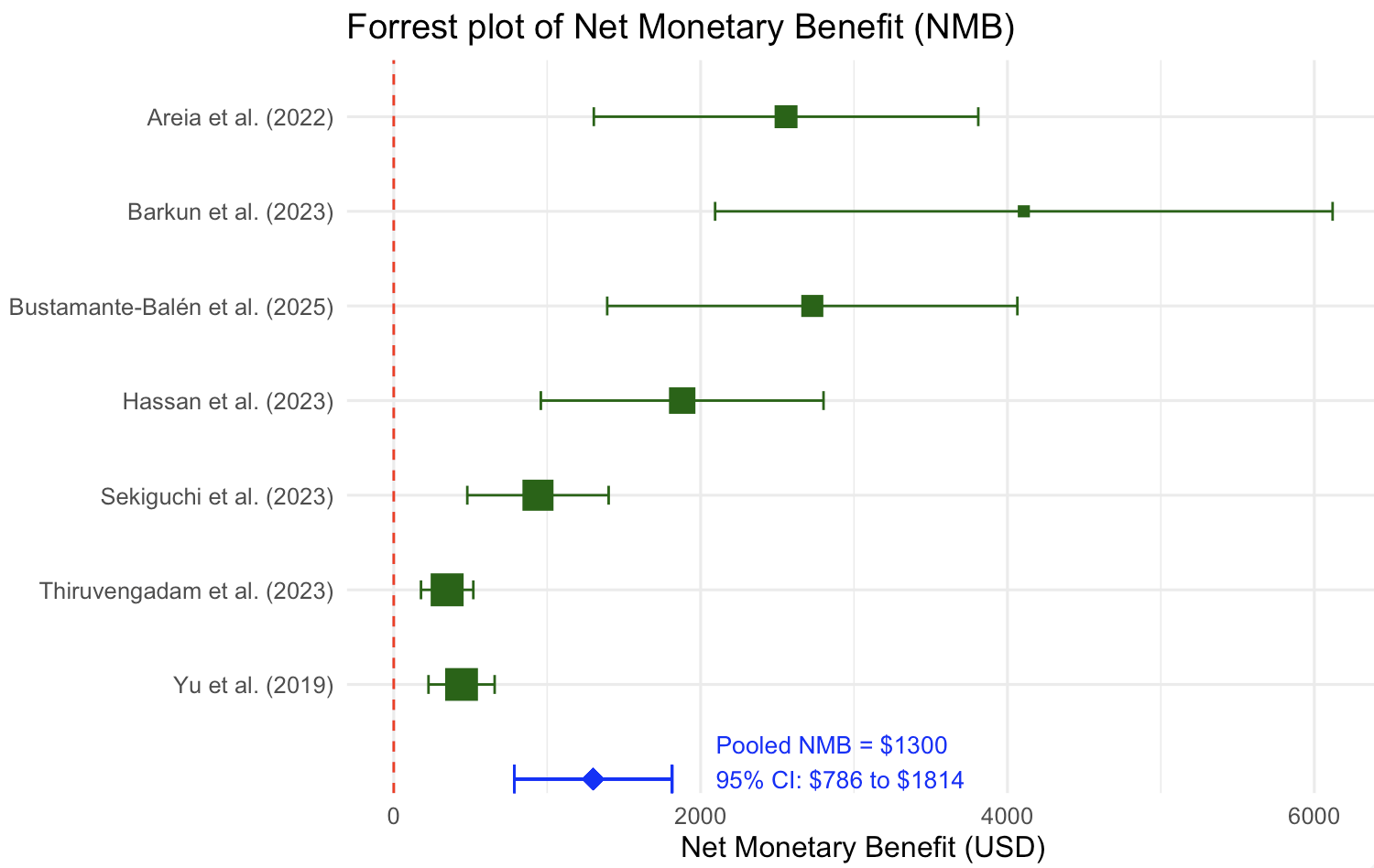
Figure: Forest plot of net monetary benefit (NMB) for AI-assisted colonoscopy compared to standard colonoscopy across seven studies. Each square represents the point estimate of NMB, with horizontal lines indicating 95% confidence intervals. Square size reflects study weight. The pooled NMB (blue diamond) was $1,300 (95% CI: $786 to $1,814), indicating significant cost-effectiveness. The red dashed line represents the cost-effectiveness threshold (NMB = 0).
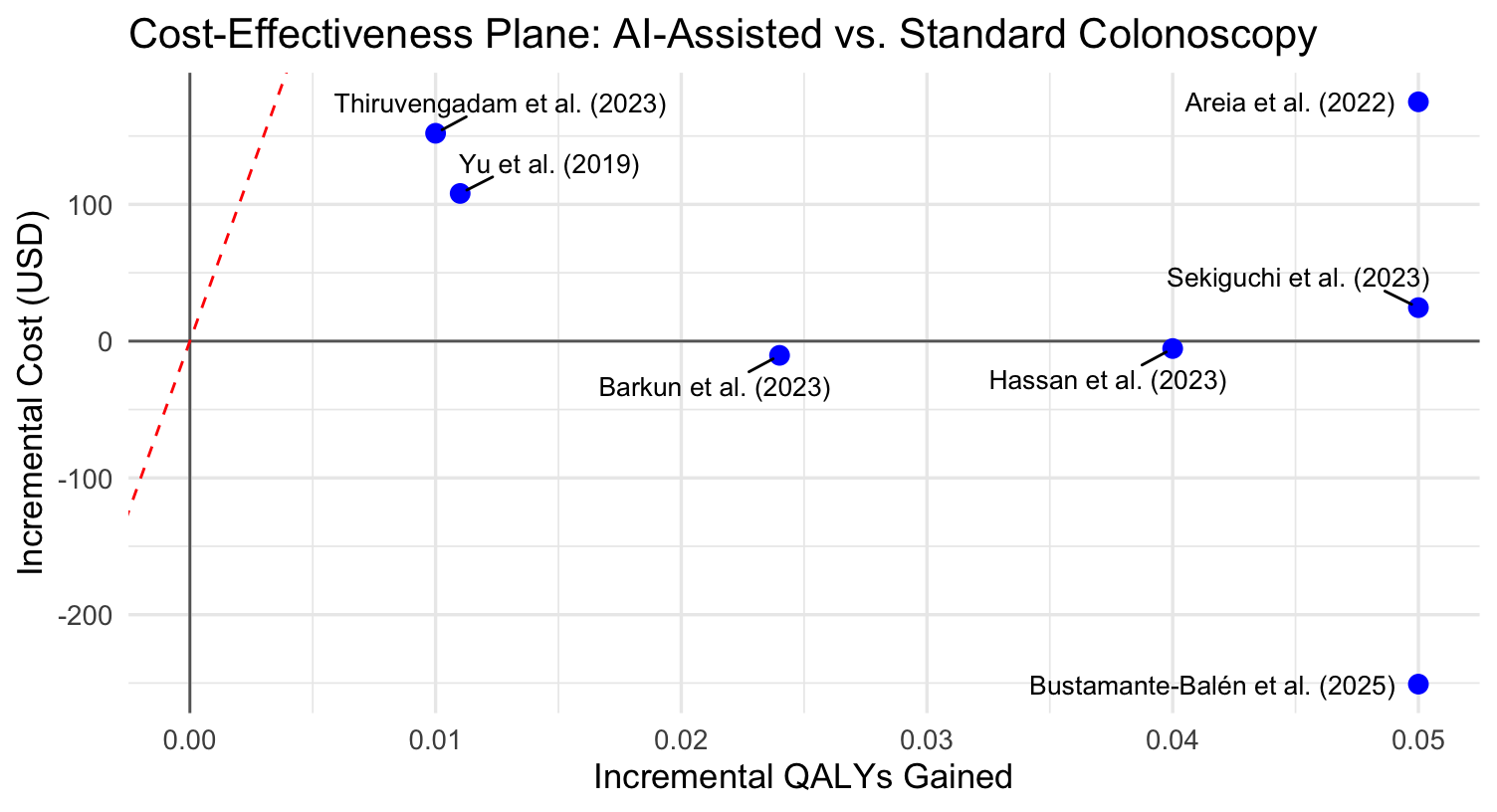
Figure: Cost-effectiveness plane comparing AI-assisted colonoscopy to standard colonoscopy across seven economic evaluation studies. Each point represents a study's incremental cost and incremental QALYs gained. The red dashed line indicates the willingness-to-pay threshold of $50,000 per QALY. Points below the line are considered cost-effective; points in the lower-right quadrant are classified as dominant (more effective and less costly).
Disclosures:
Arashdeep Singh Singh indicated no relevant financial relationships.
Sarthak Sharma indicated no relevant financial relationships.
Shahdil Khusroo indicated no relevant financial relationships.
Arashdeep Singh Singh, MBBS1, Sarthak Sharma, MBBS2, Shahdil Khusroo, 3. P0493 - Is Artificial Intelligence Cost-Effective in Colonoscopy? A Systematic Review and Meta-Analysis of Economic Evaluations and Modeling Studies, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Government Medical College and Hospital, Amritsar, Punjab, India; 2Government Medical College, Jammu, Jammu, Jammu and Kashmir, India; 3BHARAT RATNA LATE SHRI ATAL BIHARI VAJPAYEE MEMORIAL MEDICAL COLLEGE , RAJNANDGAON, CHHATTISGARH, Rajnandgaon, Chhattisgarh, India
Introduction: Artificial intelligence (AI) is increasingly being used to enhance colonoscopy and improve adenoma detection rates (ADRs), potentially lowering colorectal cancer (CRC) incidence. However, its cost-effectiveness remains unclear. We conducted a systematic review and meta-analysis to assess whether AI-assisted colonoscopy is a cost-effective or cost-saving strategy across different healthcare systems.
Methods: A systematic literature search was conducted across six databases: PubMed (MEDLINE), Google Scholar, ScienceDirect, PLOS ONE, Cochrane Library, and ClinicalTrials.gov. Studies comparing AI-assisted colonoscopy to standard colonoscopy were included. Outcomes of interest included incremental cost-effectiveness ratios (ICERs), net monetary benefit (NMB), and other modeled cost and effectiveness measures. Data were standardized to USD where applicable and pooled using a random-effects meta-analysis. Risk of bias was assessed using the Philips</span> <span style="font-size: 11pt; font-family: Arial,sans-serif; color: #000000; background-color: transparent; font-weight: 400; font-style: normal; font-variant: normal; text-decoration: none; vertical-align: baseline; white-space: pre-wrap;">checklist for modeling studies. A forest plot and cost-effectiveness plane were constructed to visualize study results in relation to a $50,000/QALY willingness-to-pay threshold using RStudio (Version 2025.05.0+496).
Results: Nine studies were included, seven of which reported ICER or NMB values and were synthesized quantitatively. The pooled net monetary benefit was $1,300 (95% CI: $786–$1,814; p < 0.001), supporting the cost-effectiveness of AI-assisted colonoscopy. Heterogeneity was high (I² = 87.7%) due to variations in model design and healthcare settings. All studies fell within the cost-effective or dominant quadrants of the cost-effectiveness plane. Bustamante-Balén et al. and Barkun et al. showed dominant strategies, while Yu et al. and Hassan et al. reported favorable ICERs below $50,000/QALY. Two studies were assessed qualitatively: Mori et al. reported cost savings using a “diagnose-and-leave” strategy; Halvorsen et al. noted increased surveillance burden despite marginal cancer risk reduction.
Discussion: AI-assisted colonoscopy was consistently cost-effective, with several studies demonstrating dominant strategies. Despite substantial heterogeneity, all studies fell within the cost-effective or dominant regions of the cost-effectiveness plane. Integration into clinical practice should balance potential cost savings with the implications of increased surveillance burden. As current evidence is primarily based on modeling studies, cautious implementation and further validation in diverse real-world settings are warranted.
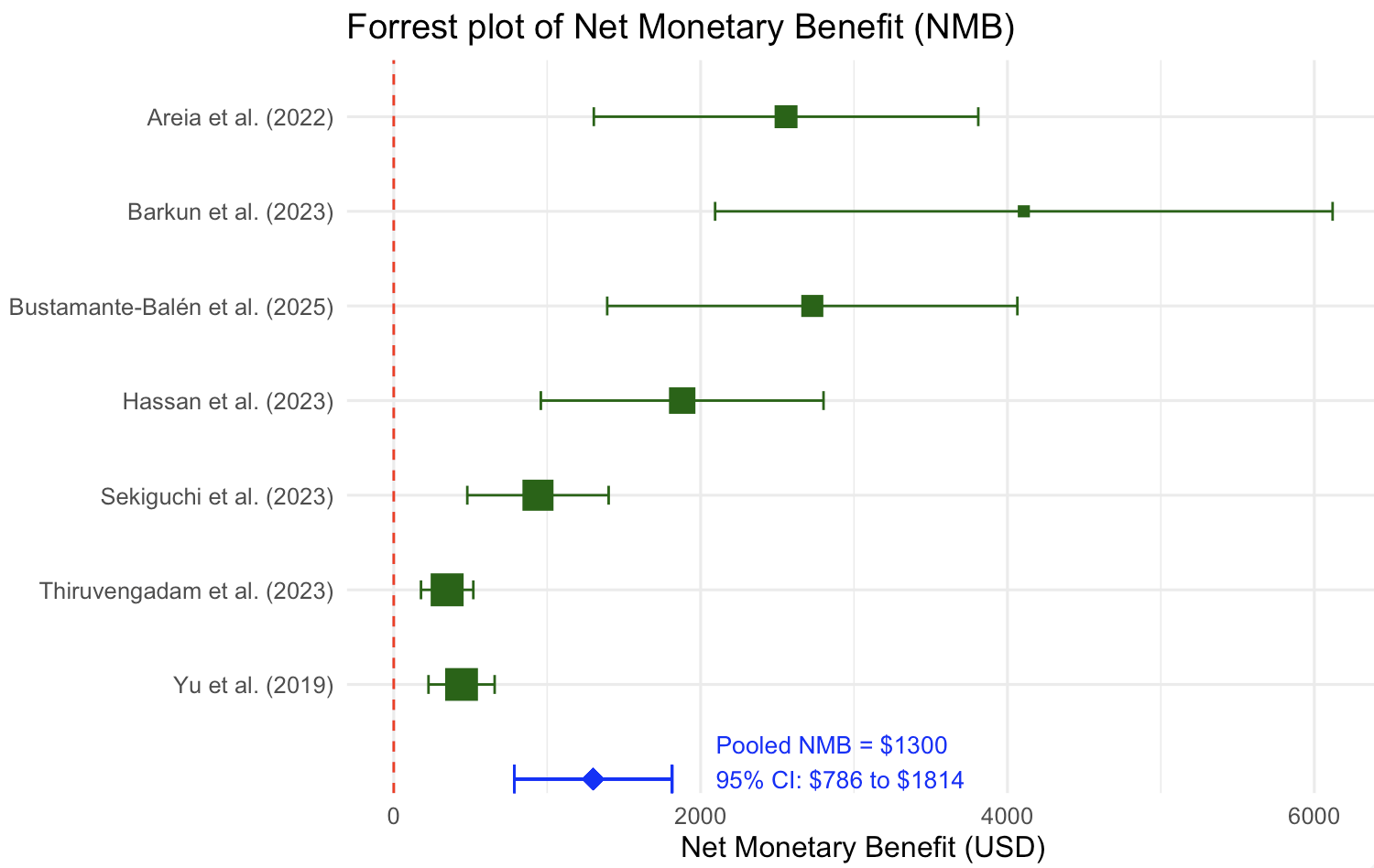
Figure: Forest plot of net monetary benefit (NMB) for AI-assisted colonoscopy compared to standard colonoscopy across seven studies. Each square represents the point estimate of NMB, with horizontal lines indicating 95% confidence intervals. Square size reflects study weight. The pooled NMB (blue diamond) was $1,300 (95% CI: $786 to $1,814), indicating significant cost-effectiveness. The red dashed line represents the cost-effectiveness threshold (NMB = 0).
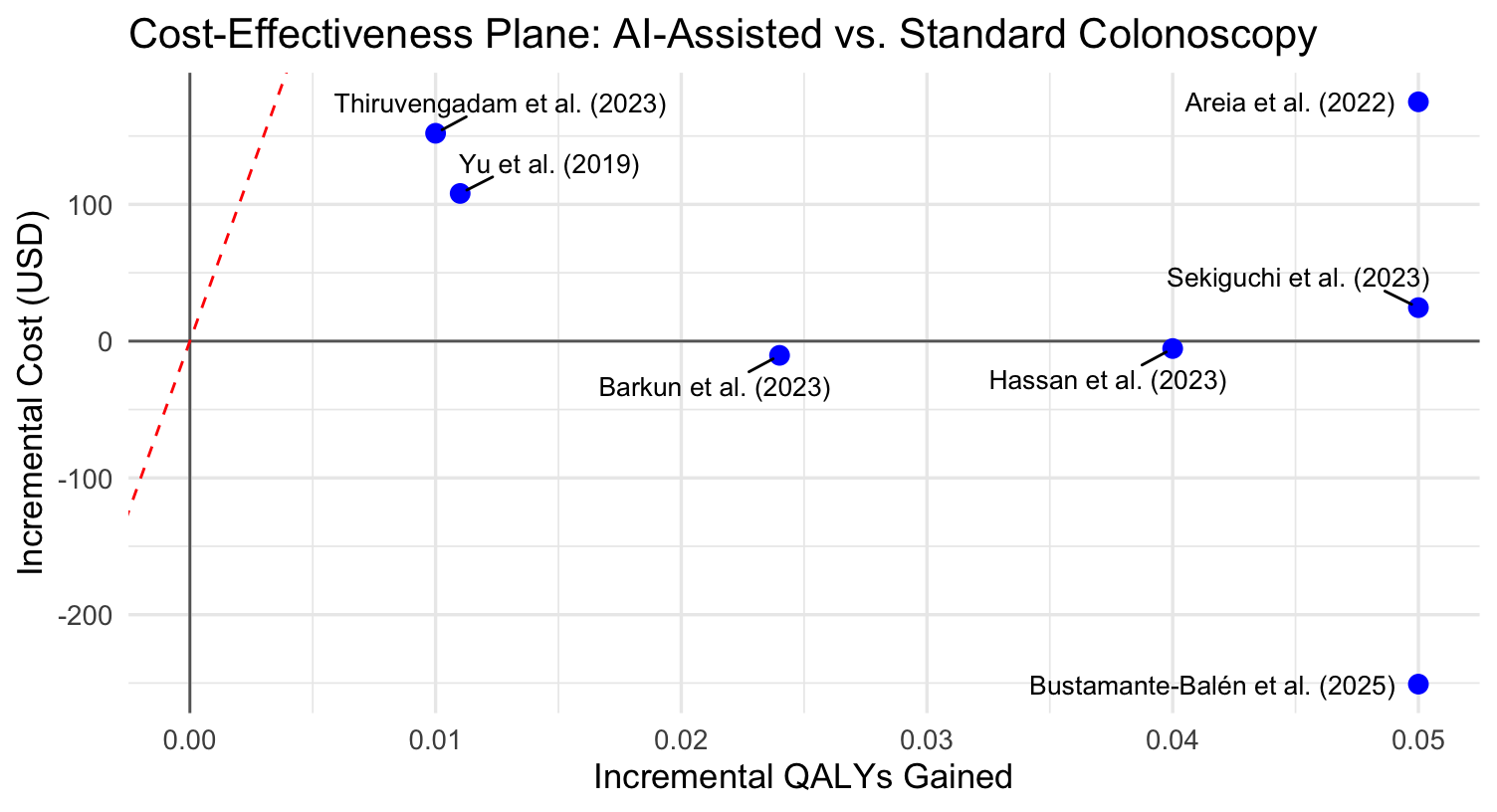
Figure: Cost-effectiveness plane comparing AI-assisted colonoscopy to standard colonoscopy across seven economic evaluation studies. Each point represents a study's incremental cost and incremental QALYs gained. The red dashed line indicates the willingness-to-pay threshold of $50,000 per QALY. Points below the line are considered cost-effective; points in the lower-right quadrant are classified as dominant (more effective and less costly).
Disclosures:
Arashdeep Singh Singh indicated no relevant financial relationships.
Sarthak Sharma indicated no relevant financial relationships.
Shahdil Khusroo indicated no relevant financial relationships.
Arashdeep Singh Singh, MBBS1, Sarthak Sharma, MBBS2, Shahdil Khusroo, 3. P0493 - Is Artificial Intelligence Cost-Effective in Colonoscopy? A Systematic Review and Meta-Analysis of Economic Evaluations and Modeling Studies, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
