Sunday Poster Session
Category: Colorectal Cancer Prevention
P0481 - Choosing Stool DNA vs Colonoscopy: Racial, Geographic, and Age Disparities in Colorectal Cancer Screening From BRFSS Data (2022–2023)
Sunday, October 26, 2025
3:30 PM - 7:00 PM PDT
Location: Exhibit Hall

Kobina Essilfie-Quaye, MD (he/him/his)
University of Central Florida, HCA Healthcare GME
Gainesville, FL
Presenting Author(s)
Kobina Essilfie-Quaye, MD1, Dennis Dela. Tsagli, MD2, Yeshika Thapa, MD3, Bahar Rehan, MD1, Mohammed Janajri, MD3, Dennis Collins, MD3
1University of Central Florida, HCA Healthcare GME, Gainesville, FL; 2Washington University in St Louis, St. Louis, MO; 3University of Central Florida, Gainesville, FL
Introduction: Colorectal cancer (CRC) remains a leading cause of cancer-related mortality in the United States. Despite the proven effectiveness of screening, significant disparities persist in modality uptake especially among racial/ethnic minorities, rural residents, and younger adults. This study examined sociodemographic predictors of choosing stool DNA testing over endoscopic methods (colonoscopy/sigmoidoscopy) using pooled Behavioral Risk Factor Surveillance System (BRFSS) 2022–2023 data.
Methods: We analyzed adults aged 45–75 years who reported undergoing either stool DNA or endoscopic CRC screening. Bivariate associations were assessed using chi-square tests. Multivariable logistic regression evaluated predictors of stool DNA-only use, adjusting for sex, age, race/ethnicity, residence, and insurance.
Results: Among 30,932 screening-eligible respondents, 2,780 (9.0%) used stool DNA testing exclusively. Women (AOR: 1.48; 95% CI: 1.37–1.60) and rural residents (AOR: 1.23; 95% CI: 1.10–1.38) had higher odds of stool DNA use. Asians (AOR: 1.55; 95% CI: 1.18–2.03) and Hispanics (AOR: 1.49; 95% CI: 1.28–1.73) were significantly more likely than Whites to use stool DNA. Use declined steeply with age, with adults ≥70 years having nearly 80% lower odds compared to those aged 45–49.
Discussion: Stool DNA testing is more frequently adopted among rural residents, Asians, Hispanics, and younger adults, groups historically underserved by endoscopy-based screening. These trends suggest that non-invasive stool-based modalities, such as Cologuard and FIT, may serve as vital tools for bridging colorectal cancer screening gaps across marginalized populations, especially given that endoscopy-based screening tends to favor urban, white, and older populations. Public health programs should prioritize expanding access to these tests to improve equity in CRC screening and reduce the long-standing disparities tied to geography, age, and race.
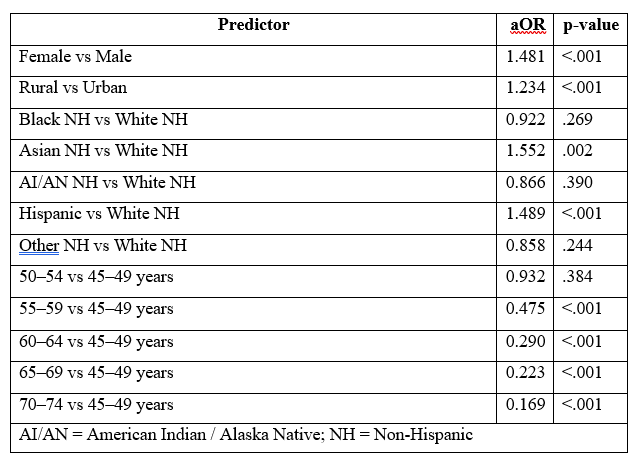
Figure: Table 1: Adjusted Odds Ratios (aOR) for Stool DNA vs. Endoscopy Use, BRFSS 2022–2023
Disclosures:
Kobina Essilfie-Quaye indicated no relevant financial relationships.
Dennis Tsagli indicated no relevant financial relationships.
Yeshika Thapa indicated no relevant financial relationships.
Bahar Rehan indicated no relevant financial relationships.
Mohammed Janajri indicated no relevant financial relationships.
Dennis Collins indicated no relevant financial relationships.
Kobina Essilfie-Quaye, MD1, Dennis Dela. Tsagli, MD2, Yeshika Thapa, MD3, Bahar Rehan, MD1, Mohammed Janajri, MD3, Dennis Collins, MD3. P0481 - Choosing Stool DNA vs Colonoscopy: Racial, Geographic, and Age Disparities in Colorectal Cancer Screening From BRFSS Data (2022–2023), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, HCA Healthcare GME, Gainesville, FL; 2Washington University in St Louis, St. Louis, MO; 3University of Central Florida, Gainesville, FL
Introduction: Colorectal cancer (CRC) remains a leading cause of cancer-related mortality in the United States. Despite the proven effectiveness of screening, significant disparities persist in modality uptake especially among racial/ethnic minorities, rural residents, and younger adults. This study examined sociodemographic predictors of choosing stool DNA testing over endoscopic methods (colonoscopy/sigmoidoscopy) using pooled Behavioral Risk Factor Surveillance System (BRFSS) 2022–2023 data.
Methods: We analyzed adults aged 45–75 years who reported undergoing either stool DNA or endoscopic CRC screening. Bivariate associations were assessed using chi-square tests. Multivariable logistic regression evaluated predictors of stool DNA-only use, adjusting for sex, age, race/ethnicity, residence, and insurance.
Results: Among 30,932 screening-eligible respondents, 2,780 (9.0%) used stool DNA testing exclusively. Women (AOR: 1.48; 95% CI: 1.37–1.60) and rural residents (AOR: 1.23; 95% CI: 1.10–1.38) had higher odds of stool DNA use. Asians (AOR: 1.55; 95% CI: 1.18–2.03) and Hispanics (AOR: 1.49; 95% CI: 1.28–1.73) were significantly more likely than Whites to use stool DNA. Use declined steeply with age, with adults ≥70 years having nearly 80% lower odds compared to those aged 45–49.
Discussion: Stool DNA testing is more frequently adopted among rural residents, Asians, Hispanics, and younger adults, groups historically underserved by endoscopy-based screening. These trends suggest that non-invasive stool-based modalities, such as Cologuard and FIT, may serve as vital tools for bridging colorectal cancer screening gaps across marginalized populations, especially given that endoscopy-based screening tends to favor urban, white, and older populations. Public health programs should prioritize expanding access to these tests to improve equity in CRC screening and reduce the long-standing disparities tied to geography, age, and race.
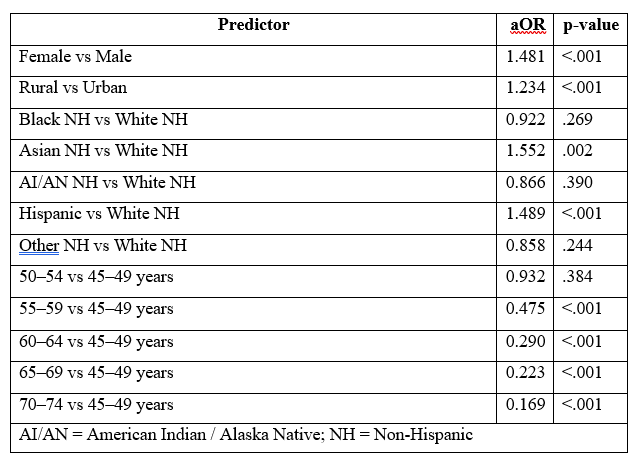
Figure: Table 1: Adjusted Odds Ratios (aOR) for Stool DNA vs. Endoscopy Use, BRFSS 2022–2023
Disclosures:
Kobina Essilfie-Quaye indicated no relevant financial relationships.
Dennis Tsagli indicated no relevant financial relationships.
Yeshika Thapa indicated no relevant financial relationships.
Bahar Rehan indicated no relevant financial relationships.
Mohammed Janajri indicated no relevant financial relationships.
Dennis Collins indicated no relevant financial relationships.
Kobina Essilfie-Quaye, MD1, Dennis Dela. Tsagli, MD2, Yeshika Thapa, MD3, Bahar Rehan, MD1, Mohammed Janajri, MD3, Dennis Collins, MD3. P0481 - Choosing Stool DNA vs Colonoscopy: Racial, Geographic, and Age Disparities in Colorectal Cancer Screening From BRFSS Data (2022–2023), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
